Abstract
Adrenal myelolipoma is a benign metaplastic collection of reticuloendothelial cells and adipose tissue, believed to be secondary to chronic stimulation of the adrenals. Keratoconus is the most common corneal ectasia of unknown pathogenesis. Altered expression of proteinases, proteinases inhibitors, and cytokines are believed to have a role. We report for the first time, the occurrence of adrenal myelolipoma in a 52-year-old man with bilateral keratoconus with right corneal scarring for 13 years, who had presented with abdominal pain and heaviness for 4 weeks. Computerized tomography abdomen revealed 7.4 × 7.0 × 6.6 cm hypo-dense variegated left adrenal mass [–71 to –51 Hounsfield Unit (HU)] with smooth borders and poor contrast uptake, suggestive of adrenal myelolipoma, which was biochemically non-functional in view of normal overnight dexamethasone suppressed cortisol (1.4 mcg/dl), 24 h urinary fractionated metanephrines [metanephrines 57 mcg/day (53-341); normetanephrines 95 mcg/day (88-444)], androgen levels [dehydroepiandrostenedione-sulphate 112 mcg/dl (21-123); testosterone 542 ng/dl (275-1200)] with normal visualization of the contralateral adrenal. The cause of this association could not be determined. However, it may be hypothesized that altered adrenal steroid metabolism may have some role in the development of myelolipoma in our patient with keratoconus; in view of increased occurrence of myelolipoma in patients with congenital adrenal hyperplasia (CAH), isolated report of keratoconus in twins with CAH and mice model of keratoconus demonstrating the role of androgens in the development of keratoconus.
Keywords: Adrenal myelolipoma, keratoconus, steroid metabolism
INTRODUCTION
Myelolipomas are rare benign tumors, composed of adipose and hematopoietic tissue in varying proportions, a result of metaplasia of reticuloendothelial cells, most commonly located in the adrenals. The cause of this metaplasia is not well-known, but it is believed to be due to chronic adrenal stimulation by ACTH [congenital adrenal hyperplasia (CAH), Addison's disease, Cushing's syndrome], chronic infection, necrosis, stress, or exogenous steroid use.[1] They occur most commonly in fifth to seventh decade without any sex preponderance.[1] Keratoconus is the most common ectatic corneal disorder characterized by conical shape of cornea due to thinning of cornea as a result of degeneration, usually bilateral, leading to severe myopia and astigmatism.[2] The association of adrenal myelolipoma with keratoconus has not been reported previously.
CASE REPORT
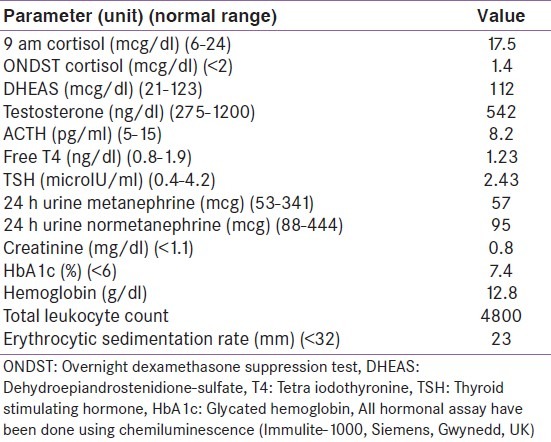
A 52-year-old gentleman, diagnosed with bilateral keratoconus 13 years back during evaluation for decreased vision in right eye [Figure 1a and b], hypertensive for last 4 years on amlodipine 5 mg/day, diagnosed diabetic 2 months back on metformin 1 g/day, was detected to have right adrenal mass on ultrasonography abdomen done as a part of evaluation for pain and heaviness in the left lumbar region of 4 weeks duration. Examination was significant for obesity (BMI –32.6 kg/m2), with acanthosis, absence of stigmata of Cushing's syndrome, normal blood pressure, soft hepatomegaly without any other palpable abdominal mass. Computerized tomography abdomen revealed 7.4 × 7.0 × 6.6 cm hypo-dense variegated left adrenal mass [–71 to –51 Hounsfield Unit (HU)] with smooth borders suggestive of adrenal myelolipoma. The right adrenal was normally visualized [Figure 2]. Hemogram, renal function, 9 am cortisol, over-night dexamethasone suppressed serum cortisol, 24 h urine fractionated metanephrines, and electrolytes were normal [Table 1]. He was referred to the surgeon for removal of the left adrenal mass.
Figure 1a.

Picture of eyes showing bilateral keratoconus, with presence of corneal opacity (scarring) of right eye
Figure 1b.

Picture of left eye showing keratoconus (lateral view)
Figure 2.
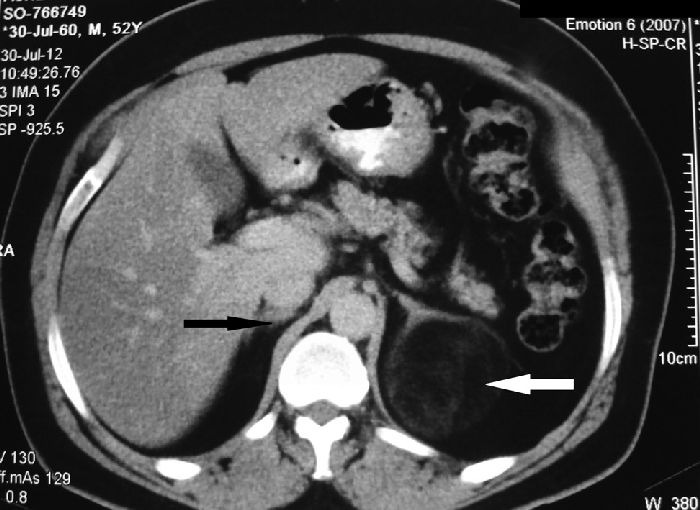
Computerized tomography (CT) abdomen showing 7.4 × 7 × 6.6 cm hypointense variegated left adrenal mass with smooth borders with poor contrast uptake (–71 to –51 Hounsfield Unit) without any areas of calcification suggestive of myelolipoma (white arrow). Right adrenal is normal (black arrow)
Table 1.
Hormonal and biochemical parameters
DISCUSSION
Keratoconus is relatively common disorder in India with a prevalence of 2300 per 100,000 population.[2] Its etiopathogenesis is not well-known. Degeneration of cornea may be the result of increased proteolytic enzyme activity (acid phosphatase, acid esterase, cathepsin B, cathepsin G, cathepsin K, and trypsin-2) along with decreased proteinase inhibitors (alpha2-macroglobulin, alpha1-antiprotease) in the cornea. Increased inflammatory markers and cytokines (IL-1, IL1R, IL-6, ICAM-1, VCAM- 1) have been documented in keratoconus, which may promote keratinocyte apoptosis.[2] Increased expression of pro-apoptotic protein secreted frizzled related protein-1 (SFRP- 1) and Fas-ligand has been documented in keratoconus.[2] Increased eye rubbing (associated with increased corneal inflammatory markers) along with contact lens use (non-gas permeable) are risk factors for keratoconus. Eye rubbing may also explain its increased occurrence in patients with atopy and asthma.[2]
There is only a single report till date linking adrenal pathology to keratoconus. Keratoconus was observed in 2 dizygotic twins with non-classical CAH (21-hydroxylase deficiency).[3] Increased circulating androgens (due to CAH) were believed to effect the normal development of cornea, inducing stromal abnormalities leading to keratoconus in these twins.[3] An association between keratoconus and major histocompatibility complex (MHC) region has been reported in humans.[4]
Expression of androgen receptors on keratinocytes, epithelial and endothelial cells of mice have been documented.[4] In an animal model of keratoconus (SKC mice), keratoconus was observed only in sexually matured male but not in female mice. Females developed keratoconus on receiving androgen injection.[4] Slp gene in the MHC region encoding a sex-limited protein in males, which can also be induced in females by androgens, is believed to have a role in the development of keratoconus.[4] The occurrence of keratoconus, mostly after the onset of puberty in humans with a higher prevalence in males (1.5-2:1), may suggest the role of sex hormones in its pathogenesis.[2,4]
There is an increased occurrence of adrenal myelolipoma in patients with CAH with more than 31 cases reported till date, believed to be due to chronic adrenal stimulation by ACTH.[5] However, the occurrence of myelolipoma in a patient with keratoconus has not been reported. Our patient had left adrenal myelolipoma, which was non-functional as evidenced by normal hormone status [Table 1] and visualization of the contralateral adrenal [Figure 2]. He had long-standing keratoconus with right corneal scarring. In view of the previous observation of altered androgen metabolism having a role in the development of keratoconus, we believe some unknown alternation in adrenal steroid metabolism may have some role in the development of myelolipoma as well as keratoconus in our patient. However, androgen levels, cortisol, and ACTH were normal in our patient. This report intends to highlight this novel association, the cause of which could not be determined. Keen watch out for similar such observation with further study is warranted.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Doddi S, Singhal T, Leake T, Sinha P. Management of an incidentally found large adrenal myelolipoma: A case report. Cases J. 2009;2:8414. doi: 10.4076/1757-1626-2-8414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kok YO, Tan GF, Loon SC. Review: Keratoconus in Asia. Cornea. 2012;31:581–93. doi: 10.1097/ICO.0b013e31820cd61d. [DOI] [PubMed] [Google Scholar]
- 3.Incorvaia C, Parmeggiani F, Costagliola C, Perri P, Tittoni M, Sebastiani A. Congenital adrenal hyperplasia due to 21-hydroxylase deficiency associated with bilateral keratoconus. Am J Ophthalmol. 2003;135:557–9. doi: 10.1016/s0002-9394(02)01979-7. [DOI] [PubMed] [Google Scholar]
- 4.Tachibana M, Adachi W, Kinoshita S, Kobayashi Y, Honma Y, Hiai H, et al. Androgen-dependent hereditary mouse keratoconus: Linkage to an MHC region. Invest Ophthalmol Vis Sci. 2002;43:51–7. [PubMed] [Google Scholar]
- 5.German-Mena E, Zibari GB, Levine SN. Adrenal myelolipomas in patients with congenital adrenal hyperplasia: Review of the literature and a case report. Endocr Pract. 2011;17:441–7. doi: 10.4158/EP10340.RA. [DOI] [PubMed] [Google Scholar]


