Abstract
Introduction:
The IMPROVE Control Training program was designed by Indian Academy of Diabetes (IAD), and a non-intervention study was conducted to evaluate the effectiveness of this standardized healthcare professionals (HCPs) training program on achieving treatment goals in patients with diabetes mellitus and its impact on standard of care.
Materials and Methods:
This multi-center, parallel group, open-label, non-randomized, non-intervention study included patients with type 2 diabetes who had an HbA1c >9 at time of diagnosis or an HbA1c >7% even after 6 months of initiation of therapy with anti-diabetic agents (Oral anti diabetic agents (OADs) and/or insulin). The data recorded at baseline included demographic characteristics, medical history, and the treatment regimens.
Results:
The study included 20,493 patients with diabetes, of which 13,295 (64.9%) were men. The mean [standard deviation (SD)] duration of diabetes was 6.4 (4.2) years and 6608 (32.2%) reported complications of diabetes. Poor glycemic control [HbA1c = 9.4 (1.3), FPG (mg/dl) = 181.2 (45.7); mean (SD)] was observed. The postprandial glucose was also high [post-breakfast, lunch, and dinner values in mg/dl were 263.6 (68.5), 278.1 (69.6), and 250.2 (63.7), respectively] in these patients. Failure of OADs was the most common reason cited for initiation of insulin. Premixed insulin was rated the regimen of choice for initiating therapy by the physicians (62.2% vs. 34.5% who preferred basal insulin).
Conclusion:
The baseline results confirm the poor glycemic control and the delayed initiation and/or inadequacy of treatment in subjects with type 2 diabetes. These results also highlight the need for early and optimal insulin-based therapy.
Keywords: baseline characteristics, oral anti diabetic agents failure, insulin initiation, IMPROVE
In India, the value of early intervention to achieve optimal glycemic control is not yet realized to its capacity due to lack of a formal training in insulin therapy and widespread clinical inertia.[1] In this background, the IMPROVE Control Program, 2011 intended to propagate the need to aim for a well-defined glycemic target (HbA1c <7% within 180 days of intervention). As a part of this healthcare professional (HCP) training, the series of workshops were held in the early part of 2011. A need to evaluate the impact of this kind of educational intervention on treatment outcomes, standards of care, and subsequent clinical outcomes of diabetes was also realized. Subsequently, a non-intervention study was conducted to evaluate the effectiveness of this standardized HCPs training program on achieving treatment goals in patients with diabetes mellitus and its impact on standards of care. It was hypothesized that a structured, evidence-based HCPs training program would help more patients achieve treatment goals and would improve physicians’ standard of care.
This multi-center, parallel group, open-label, non-randomized, non-intervention study included patients with type 2 diabetes who had an HbA1c >9% at time of diagnosis or an HbA1c >7% even after 6 months of initiation of therapy with anti-diabetic agents (OADs and/ or insulin). The principal arm included physicians who had attended the standardized training program(s) developed by the steering committee. These physicians collected data of their first 20 patients for whom they initiated treatment after attending the structured HCPs training program. The comparator group had physicians who were not a part of these training program(s). These physicians also collected data of their 20 patients whom they treated as per their routine clinical practice. Considering the non-interventional study design, there would be no study drug or specified treatment flow. The inclusion of patients was at discretion of the treating physician. The physician also determined the treatment for the diabetes, the starting dose and administration frequency, as well as later changes to either dose or frequency, if any. The data recorded at baseline included demographic characteristics, medical history, and the treatment regimens. A pre-study physician perceptions questionnaire on diabetes, and clinical practice was also filled up by the participating physicians. Here, we report the baseline characteristics and the glycemic parameters of the patients who were evaluated in this study.
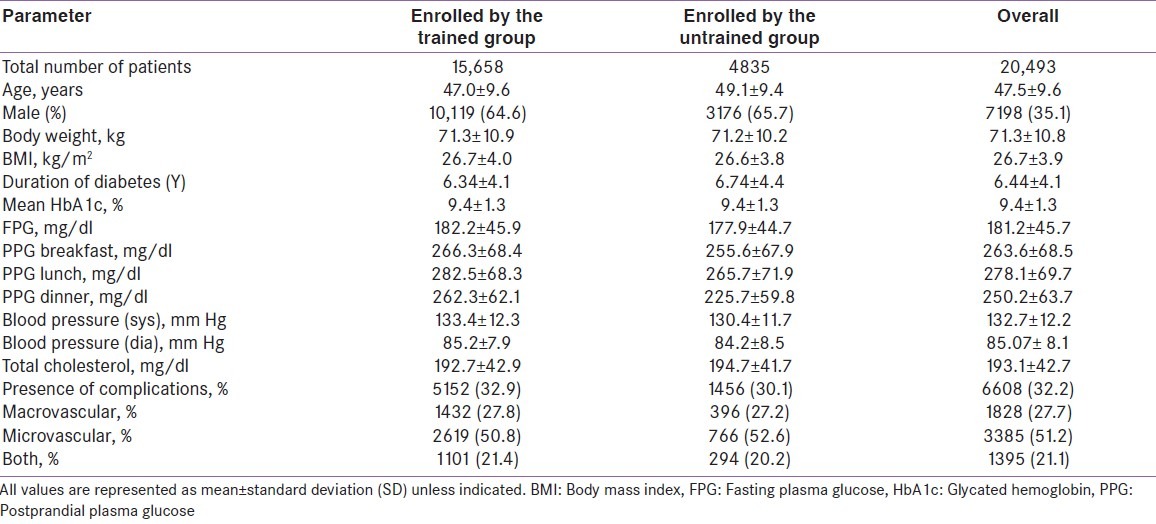
The study included 20,493 patients with diabetes, of which 13,295 (64.9%) were males. The mean (SD) duration of diabetes was 6.4 (4.2) years and 6608 (32.2%) reported complications of diabetes. Poor glycemic control [HbA1c (%) = 9.4 (1.3), FPG (mg/dl) = 181.2 (45.7); mean (SD)] was observed. The postprandial glucose was also high [post-breakfast, lunch, and dinner values in mg/dl were 263.6 (68.5), 278.1 (69.6), and 250.2 (63.7), respectively] in these patients. Failure of OADs was the most common reason cited for initiation of insulin. Premixed insulin was rated the regimen of choice for initiating therapy by the physicians (62.2% vs. 34.5% who preferred basal insulin). The baseline characteristics and glycemic parameters are described in Table 1.
Table 1.
Baseline characteristics of the patients in the IMPROVE Control program
The baseline results confirm the poor glycemic control and the delayed initiation and/or inadequacy of treatment in subjects with type 2 diabetes. These results also highlight the need for early and optimal insulin-based therapy. Similar results from the A1chieve®, DiabCare India, and IMPROVE™ studies (including the Indian cohort) confirm poor glycemic control and the delayed initiation and/or inadequacy of treatment in subjects with type 2 diabetes.[2–4] These results also highlight the need for timely and appropriately intensive insulin-based therapy. The data also represent a severe and serious indictment of current treatment approaches. Landmark studies have emphasized on the need for achieving glycemic control as early as possible to reap the long-term beneficial effects of reduction in cardiovascular and microvascular complications.[5] Besides, optimal management of co-morbidities such as hypertension and dyslipidemia would further improve the therapeutic outcomes. Results from the IMPROVE Control Program will further assist to design a structured accredited uniform education program for HCPs to highlight the benefits of an early intervention strategy and provide a guidance for implementing it.
Footnotes
Source of Support: Unrestricted educational grant from novonordisk India Limited
Conflict of Interest: None declared
REFERENCES
- 1.Indian National Consensus Group. Premix insulin: Initiation and continuation guidelines for management of diabetes in primary care. J Assoc Physicians India. 2009;57:S42–6. [Google Scholar]
- 2.Home P, Naggar NE, Khamseh M, Gonzalez-Galvez G, Shen C, Chakkarwar P, et al. An observational non-interventional study of people with diabetes beginning or changed to insulin analogue therapy in non-Western countries: The A1chieve study. Diabetes Res Clin Pract. 2011;94:352–63. doi: 10.1016/j.diabres.2011.10.021. [DOI] [PubMed] [Google Scholar]
- 3.Mohan V, Seshiah V, Sahay BK, Shah SN, Rao PV, Banerjee S, et al. Current status of management of diabetes and glycaemic control in India: Preliminary results from the DiabCare India 2011 study. Diabetes. 2012;61:A645–77. [Google Scholar]
- 4.Valensi P, Benroubi M, Borzi V, Gumprecht J, Kawamori R, Shaban J, et al. Initiating insulin therapy with, or switching existing insulin therapy to, biphasic insulin aspart 30/70 (NovoMix 30) in routine care: Safety and effectiveness in patients with type 2 diabetes in the IMPROVE observational study. Int J Clin Pract. 2009;63:522–31. doi: 10.1111/j.1742-1241.2009.02002.x. [DOI] [PubMed] [Google Scholar]
- 5.Gaede P, Lund-Andersen H, Parving HH, Pedersen O. Effect of a multifactorial intervention on mortality in type 2 diabetes. N Engl J Med. 2008;358:580–91. doi: 10.1056/NEJMoa0706245. [DOI] [PubMed] [Google Scholar]


