Abstract
Background:
Celiac disease can have extra gastrointestinal tract (GIT) presentations, most of which are endocrine. The aim of this study was to present patients diagnosed to have celiac disease from an endocrine department and to study the prevalence of endocrinopathies in celiac disease.
Materials and Methods:
A total of 36 patients from the endocrinology department (LLRM Medical College, Meerut) between January 2011 and July 2012 and who were diagnosed to have celiac disease were included in the study.
Results:
Short stature was the commonest presentation (25%), other presentations included short stature and delayed puberty (20%), delayed puberty (11%), screening for celiac disease in type-1 DM patients (17%), rickets (6%), anemia not responding to oral therapy (6%), type-1 DM with recurrent hypoglycaemia (6%), and osteomalacia (3%). The endocrine manifestations include (after complete evaluation) short stature (58%), delayed puberty (31%), elevated alkaline phospahatase (67%), low calcium (22%), X-rays suggestive of osteomalacia or rickets (8%), capopedal spasm (6%), and night blindness (6%). Anti-TPO antibody positivity was found in 53%, hypothyroidism in 28%, subclinical hypothyroidism in 17%, and type-1 DM in 25% of the patients. A total of 14% patients had no GI symptoms.
Conclusion:
Celiac disease is an endocrine disrupter as well as the great masquerader having varied presentations including short stature, delayed puberty, and rickets. Some patients who have celiac disease may not have any GI symptoms, making the diagnosis all the more difficult. Also, there is significant incidence of celiac disease with hypothyroidism and type-1 DM, making screening for it important in these diseases.
Keywords: Celiac disease, short stature, delayed puberty
INTRODUCTION
Celiac disease, or gluten-sensitive enteropathy, is an autoimmune disorder characterized by inflammation, villous atrophy, and crypt hyperplasia of the small bowel mucosa after ingestion of dietary gluten and recovers when gluten-containing cereals are withdrawn from the diet. It has an incidence of 1 in 96 in north India.[1] Although this disease primarily affects the GIT, many patients may present with only subtle, if any, GI symptoms, which makes the disease difficult to diagnose. Also, celiac disease being an autoimmune disease, causes other endocrine dysfunctions, beyond its action on the GIT. This disease, due to its varied presentations, can baffle an endocrinologist. The aim of this study was to study the initial presentation in patients diagnosed to have celiac disease from an endocrine department,to study the prevalence of other endocrinopathies in patients diagnosed to have celiac disease, and to study the clinical profile of celiac disease with non-GIT presentation.
MATERIALS AND METHODS
Total 36 patients who were diagnosed to have celiac disease from the endocrinology department (LLRM Medical College, Meerut) between January 2011 and July 2012 were included in the study. Presenting complaint was defined as the complaint for which the patient sought endocrinology services. The diagnosis of celiac disease was made as per the ESPGHAN diagnostic criteria. Clinical and laboratory profiling was performed for these patients and the prevalence of other endocrinopathies (thyroid, diabetes, adrenal, and hypogonadism/delayed puberty) were screened in these patients.
RESULTS
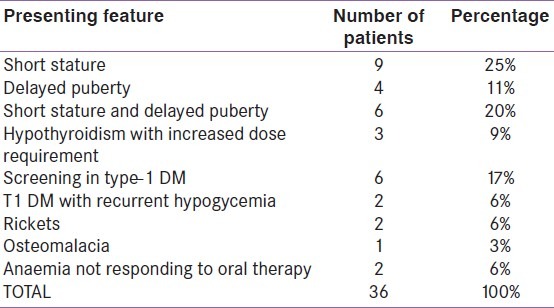
Short stature was the commonest presentation (25%), and 11% of patients had delayed puberty as the presenting complaint. A total of 20% patients had both short stature and delayed puberty as the main presentation. Other presenting complaints included hypothyroidism with increase dose requirement (9%), rickets (6%), anemia not responding to oral therapy (6%), type- and osteomalacia (3%), and 17% patients were diagnosed during screening for celiac disease in type-1 diabetes patients [Table 1].
Table 1.
Presenting feature of patients diagnosed to have celiac disease
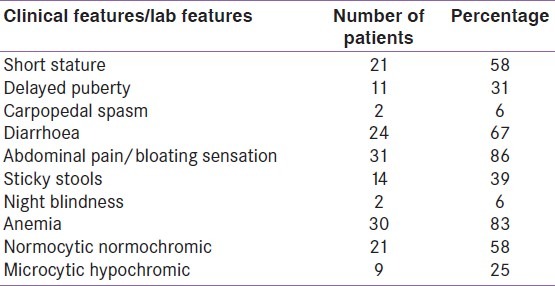
The clinical profile of celiac disease presented in our department (after complete evaluation) is as follows:
short stature in 58% patients, delayed puberty in 31%, carpopedal spasm in 6%, and night blindness in 6%. History of GI symptoms elicited included abdominal pain or bloating sensation in 86%, chronic diarrhoea in 67%, and sticky stools in 39% patients [Table 2].
Table 2.
Clinical profile of patients with celiac disease
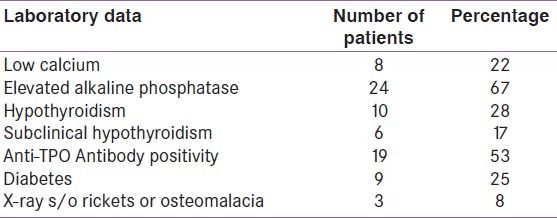
Presence of other endocrine dysfunctions included (repetitive) low calcium in 22%, elevated alkaline phosphatase in 67%, hypothyroidism in 28%, subclinical hypothyroidism in 17%, Anti-TPO antibody positivity in 53%, type-1 DM in 25%, X-rays suggestive of osteomalacia or rickets in 8% patients [Table 3].
Table 3.
Endocrine manifestations of celiac disease
DISCUSSION
Celiac disease has the classical well-recognised presentation of steatorrhea and abdominal distension in children and in adults, celiac disease typically produces diarrhoea or steatorrhea, malaise, and weight loss.[2] But celiac disease has atypical extra intestinal presentations, many of which are endocrine, making it mandatory for the endocrinologist to recognise and diagnose the disease.
Endocrinological conditions associated with celiac disease
Type-1 DM:
The incidence of celiac disease in type-1 DM is 5.4–7.4% and the patients usually have the classical symptoms of steatorrhoea, malabsorption syndrome, diarrhoea, and failure to thrive.[3] The metabolic control is usually poor with frequent episodes of hypoglycaemias. ADA recommends screening for celiac disease in patients with type-1 DM.
Thyroid disorders:
Celiac disease has an approximate incidence of 6% in patients having autoimmune thyroid disease. Patients usually have the classical presentation of diarrhoea and steatorrhoea,[4] but hypothyroidism with weight loss and increased dose requirement of L Thyroxine are two well recognised presentations of celiac disease in hypothyroidism.
Other endocrine diseases:
In a recent study, 12.5% patients with celiac disease had adrenal insufficiency, and 0.3% had primary hyperparathyroidism.[5] Celiac disease is associated with autoimmune hypophysitis, and alopecia areata has been found in 2% patients. Celiac disease has been found in 4–8% of women with unexplained infertility, and successful treatment of infertility has occurred after the diagnosis and dietary treatment of celiac disease. Celiac women have a shorter fertility period and suffer from spontaneous abortions and other complications of pregnancy more than the general population.
The coexistence of these diseases could be explained by molecular mimicry by which gliadin or tissue transglutaminase activates T cells that are cross-reactive with various self-antigens. Such inflammatory responses may have the capacity to persist in genetically susceptible hosts and lead to chronic organ-specific autoimmune disease via epitope spreading.[5]
CONCLUSION
Celiac disease is an endocrine disrupter as well as the great masquerader. It can have varied presentations including short stature, delayed puberty, rickets, or may be picked up during screening. Some patients who have celiac disease may not have any GI symptoms, making the diagnosis all the more difficult. Also, there is a significant incidence of celiac disease with hypothyroidism and type-1 DM, making screening for it important in these diseases.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Makharia GK, Verma AK, Amarchand R, Bhatnagar S, Das P, Goswami A, et al. Prevalence of celiac disease in the northern part of India: A community based study. J Gastroenterol Hepatol. 2011;26:894–900. doi: 10.1111/j.1440-1746.2010.06606.x. [DOI] [PubMed] [Google Scholar]
- 2.Visakorpi JK, Mäki M. Changing clinical features of celiac disease. Acta Paediatr Suppl. 1994;83:10–13. doi: 10.1111/j.1651-2227.1994.tb13221.x. [DOI] [PubMed] [Google Scholar]
- 3.Shanahan F, McKenna R, McCarthy CF, Drury MI. Coeliac disease and diabetes mellitus: a study of 24 patients with HLA typing. Q J Med. 1982;51:329–335. [PubMed] [Google Scholar]
- 4.Kuitunen P, Mäenpää J, Krohn K, Visakorpi JK. Gastrointestinal findings in autoimmune thyroiditis and non-goitrous juvenile hypothyroidism in children. Scand J Gastroenterol. 1971;6:335–41. [PubMed] [Google Scholar]
- 5.Schuppan D. Current concepts of celiac disease pathogenesis. Gastroenterology. 2000;119:234–42. doi: 10.1053/gast.2000.8521. [DOI] [PubMed] [Google Scholar]


