Abstract
Objectives
We sought to determine how delirium and dementia affect 1) the accuracy of the presenting illness and 2) discharge instruction comprehension in older ED patients.
Methods
This cross-sectional study was conducted at an academic ED from 5/2008 to 7/2008 and included non-nursing home patients who were 65 years old and older. Two open-ended interviews were performed to assess patients’ ability to accurately provide their presenting illness and comprehension of their ED discharge instructions (discharge diagnosis, return to ED instructions, and follow-up instructions). The surrogates’ version of the presenting illness and printed discharge instructions were the reference standards, respectively. Concordance between the patient and the reference standards were determined by two reviewers using a 5-point scale ranging from 1 (no concordance) to 5 (complete concordance). Proportional odds logistic regression was performed to determine if cognitive impairment was associated with presenting complaint accuracy and discharge instruction comprehension. All models were adjusted for age, health literacy, education, non-white race, and hearing impairment.
Results
For the presenting illness analysis, 202 patients participated. Compared with patients without cognitive impairment, those with delirium superimposed on dementia (DSD) had lower odds of agreeing with their surrogates with regard to why they were in the ED (adjusted POR = 0.20; 95%CI: 0.09 – 0.43). For the discharge instruction comprehension analysis, 115 patients participated. Patients with DSD had significantly lower odds of comprehending their discharge diagnosis (adjusted POR = 0.13; 95%CI: 0.04 – 0.47), return to the ED instructions (adjusted POR = 0.18; 95%CI: 0.04 – 0.82), and follow-up instructions (adjusted POR = 0.09; 95%CI: 0.02 – 0.35) compared with patients without cognitive impairment.
Conclusions
DSD is associated with decreased accuracy of the older patient’s presenting illness and decreased comprehension of ED discharge instructions.
Introduction
Background
For older patients (≥65 years old), an emergency department (ED) visit can be a life altering event. Many of these patients experience subsequent loss of independence and decreased health-related quality of life after their ED care.1–4 Furthermore, approximately one third of older patients who are discharged from the ED will return to the ED or die within 90 days.5 Multiple studies have shown that higher comorbidity burden and recent ED or hospital use are associated with these adverse outcomes.5, 6 To our knowledge, however, no study has considered the effect of patients’ cognitive impairment on ED communication, comprehension of discharge instructions, and subsequent adverse outcomes. Delirium and dementia are two forms of cognitive impairment that occur in 25% of older ED patients,7 yet they go unrecognized by emergency physicians in the majority of cases.7–9 According to the Diagnostic and Statistical Manual of Mental Disorders Fourth Edition, delirium is characterized by an acute and transient decline in cognition, whereas dementia is characterized by a gradual and irreversible decline in cognition.10
Importance
Recently, Hogan et al. published a consensus document advocating that emergency medicine residents be adequately trained in the detection of cognitive impairment.11 Similarly, the Society of Academic Emergency Medicine Geriatric Task Force recommended that routine cognitive assessments in the ED be a quality indicator.12 The reason is because missing cognitive impairment could be a patient safety issue. Patients with cognitive impairment may not be able to provide an accurate medical history or even know why they are being brought in for care.11, 12 If discharged from the ED, their ability to understand and carry out discharge instructions may be jeopardized. Discharge instruction comprehension has been shown to be inadequate in younger and cognitively intact patients;13, 14 we hypothesize that this problem is magnified in older and cognitively impaired ED patients. Though intuitive, the effect of presenting illness accuracy and discharge instruction comprehension has never been substantiated or quantified in the medical literature, and it is not yet routine to screen for delirium or dementia in the ED despite recent studies indicating a heightened risk of death.15–18
Elderly patients are frequent users of the ED, accounting for 17 million visits in the U.S. annually.19 The U.S. aging population is growing exponentially and by 2030, one out of five Americans will be 65 years and older.20 Consequently, the burden of delirium and dementia will also grow and will have a greater effect on our ability to adequately care for these vulnerable patients. Improving our understanding of how these forms of cognitive impairment affect patient care and contribute to adverse outcomes is crucial to improving the quality of geriatric emergency care. For these reasons, the American Geriatric Society has made this particular line of investigation of high priority.21
Goals for this Investigation
We sought to determine how delirium, dementia, and delirium superimposed on dementia affect: (1) the accuracy of the presenting complaint and (2) discharge instruction comprehension in older ED patients.
Methods
Study Design and Setting
This was a cross-sectional study conducted in a tertiary care, academic ED with 55,000 patient visits annually. The local institutional review board approved this study using verbal consent.
Study Population
A convenience sample of patients was enrolled from May 2008 to July 2008 from 8AM to 10PM. Not every eligible patient was approached during the enrollment window especially during periods of high ED volume. ED patients aged 65 years and older were included. Patients were excluded if they were present in the ED for greater than 12 hours at enrollment, non-English speaking, were previously enrolled, did not complete the CAM-ICU, were non-verbal or unable to follow simple commands at baseline, were unarousable to verbal stimuli, or were from a nursing home. The latter groups were excluded because these patients most likely have severe dementia and are not likely to be responsible for their own self care after the ED discharge. For the presenting complaint analysis, only patients with adult (≥18 years old) surrogates who were readily present in the ED and had some knowledge of why the patient was in the ED were included. For the discharge instruction comprehension analysis, only those who were discharged from the ED were included.
Study Protocol
All prospective data collection was performed by a research assistant (SNB). Prior to the start of the study, the research assistant participated in a one-week training period and received didactic lectures, studied training manuals, watched live patient demonstrations, and practiced administering the research assessments and surveys using simulated patient scenarios. At the end of the training period, the principal investigator (JHH) observed the research assistant perform these assessments and surveys in actual ED patients.
During the study period, the research assistant approached eligible patients and obtained verbal consent. Patients were deemed capable of providing consent if: 1) they were able to carry a normal adult conversation, and 2) they were able to recall aspects of the consent process such as the study’s purpose and risk. Otherwise, consent was obtained from an authorized surrogate. If the patient was not consentable in the ED, and no authorized surrogate was available, then the patient was excluded from the study.
After consent was obtained, patient demographics, place of residence, and highest level of education completed, and hearing impairment were collected prospectively. Highest level of education was recorded as an ordinal variable (elementary, middle or high school, college, or graduate school). During the ED visit, the research assistant assessed the patient for delirium, dementia, and health literacy status using standardized instruments, and also performed open-ended interviews to determine presenting illness accuracy and discharge instruction comprehension. These instruments and interviews are described in subsequent paragraphs. All prospective data collection took approximately 15 to 20 minutes to complete for each patient.
Methods of Measurements
Delirium was assessed at the time of enrollment using the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU).22 The CAM-ICU is a modification of the Confusion Assessment Method (CAM) and uses the same construct with adaptations that standardize the inattention and disorganized thinking assessments.23 The CAM-ICU is brief (less than two minutes) compared with the CAM (up to 10 minutes) making it ideal for the busy ED environment where interruptions frequently occur. Because the CAM-ICU uses objective assessments, it is easy to use and non-physicians can administer it reliably. It has been validated in a broad spectrum of patients who were sick and not sick, older and younger, intubated and non-intubated, and patients with and without dementia.22, 24 The CAM-ICU is highly sensitive (93% – 100%) and specific (89% – 100%) compared with a psychiatrist’s assessment, and has excellent interrater reliability between physicians and nurses (kappa = 0.84 – 0.96).22, 24 As part of the CAM-ICU, the Richmond Agitation and Sedation Scale (RASS) was also recorded to quantify level of consciousness.25, 26 The RASS ranges from −5 (coma) to +4 (combative).
Patients were classified as having dementia if they had one of the following: Mini-Mental State Examination (MMSE) less than 24,27 short form of the Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE) greater than 3.38,28 or dementia documented in the medical record. A combination of assessments was used to be conservative and because there was no single dementia assessment that was valid for the entire cohort. The MMSE is a widely used cognitive assessment; a cutoff of less than 24 out of a possible 30 points is 85% sensitive and 98% specific for dementia using a psychiatrist evaluation as the reference standard.29 Because patients experiencing an episode of delirium have acute changes in their cognition (most notably related to inattention and disorganized thinking), the MMSE does not accurately reflect their true pre-morbid cognitive status. Hence, scores obtained by the MMSE in delirious patients cannot be used to identify patients with potential dementia. For this reason, the MMSE was not performed in CAM-ICU positive patients. For this reason, the MMSE was not performed in CAM-ICU positive patients and instead, baseline cognitive status was determined using the short form IQCODE. The short form IQCODE is an informant questionnaire with 16-items; a cut-off of 3.38 out of 5.00 is 79% sensitive and 82% specific using Diagnostic and Statistical Manual of Mental Disorders Third Edition Revised criteria as the reference standard.28 The IQCODE was only performed in patients with an adult surrogate (≥ 18 years old) present in the ED who knew the patient for greater than 10 years. Dementia was also identified through the medical record. The research assistant searched for the word “dementia” in prior ED visits, clinic visits, or hospitalizations, and the data were verified by the principal investigator. For these analyses, delirium and dementia were combined into a 4-level categorical variable: (1) no cognitive impairment, (2) delirium only, (3) dementia only, or (4) delirium superimposed on dementia.
Health literacy was assessed through a screening question: "How often do you have someone (like a family member, friend, hospital / clinic worker, caregiver) help you read hospital materials?" This question has 5 ordinal responses ranging from 0 (never, excellent health literacy) to 4 (all the time, poor health literacy) and has an area under the receiver operating characteristic curve of 0.87 indicating very good diagnostic performance.30 If the patient did not know the answer to this question, then the surrogate was allowed to answer it. This occurred less than 5% of the time.
To assess the accuracy of the patient's presenting complaint, the research assistant performed an open-ended interview (Appendix A) asking the patient about the primary reason for the ED visit; this interview occurred at the time of enrollment. The surrogate, if present in the ED, also provided a written response of the same question and was considered to be the reference standard. This written response was obtained at the beginning of the patient interaction and prior to the patient survey in order to minimize bias. The patient and research assistant were also blinded to the surrogate’s response.
To assess patient discharge instruction comprehension, an open-ended survey (Appendix B) was performed, which was designed to test the patient’s comprehension of the following domains: discharge diagnosis, return to the ED instructions, and follow-up instructions. The interview was performed after the ED nurse reviewed these domains with the patient using the printed discharge instructions as part of the standard ED discharge process. These printed instructions were provided by the emergency physicians using Discharge 1-2-3 (Callibra Incorporated, Schaumburg, IL) and were usually standardized by diagnosis or complaint. Patients were allowed to look at their printed discharge instructions, but the research assistant was blinded to them during the interview.
The printed discharge instructions were automatically imported into the medical record. Patient responses for both surveys were recorded verbatim on to a paper-based case report form by the research assistant and all responses were immediately transferred into a Microsoft Access 2003 database (Microsoft Inc, Seattle, WA). All surveys were pretested in five patients prior to the start of the study and no modifications were required.
Dependent Variables
Approximately 6 months after enrollment was completed, two independent reviewers blinded to the patient’s cognitive status rated the patient’s responses to the presenting illness and discharge instruction comprehension surveys using a 5-point scale: 1 - no concordance / understanding, 2 - minimal concordance / understanding, 3 - partial concordance / understanding, and 4 - very good concordance / understanding, and 5 - complete concordance / understanding. For the presenting illness analysis, the surrogate’s written response was used as the reference standard. For the discharge instruction comprehension analysis, the printed discharge instructions were considered the reference standard. The two reviewers’ ratings were averaged for analysis.
Data Analysis
Patients’ baseline characteristics and outcome measures were presented using proportions for categorical variables and medians and interquartile ranges for continuous variables. Weighted kappa scores were calculated to test inter-rater reliability between the two reviewers using linear weighting for the magnitude of discordances. Because of the non-parametric distribution of our dependent variables, multiple linear regression was not used. Instead, proportional odds logistic regression was used to determine if cognitive impairment was associated with the inability to provide an accurate presenting complaint and poor patient comprehension of the discharge diagnosis, return to the ED instructions, and follow-up instructions. All four multivariable models were adjusted for age, health literacy, education, hearing impairment, and non-white race. These covariates were selected a priori and were limited to 8 degrees of freedom for each model to avoid overfitting.31 No interactions were considered. Condition indices were calculated to assess for collinearity, and Pearson Chi-square was used to determine goodness of fit for all multivariable models. Proportional odds ratios (PORs) and their 95% confidence intervals (95%CIs) were reported. All statistical analyses were performed using SAS 9.1.3 (SAS Institute, Carey, NC).
Results
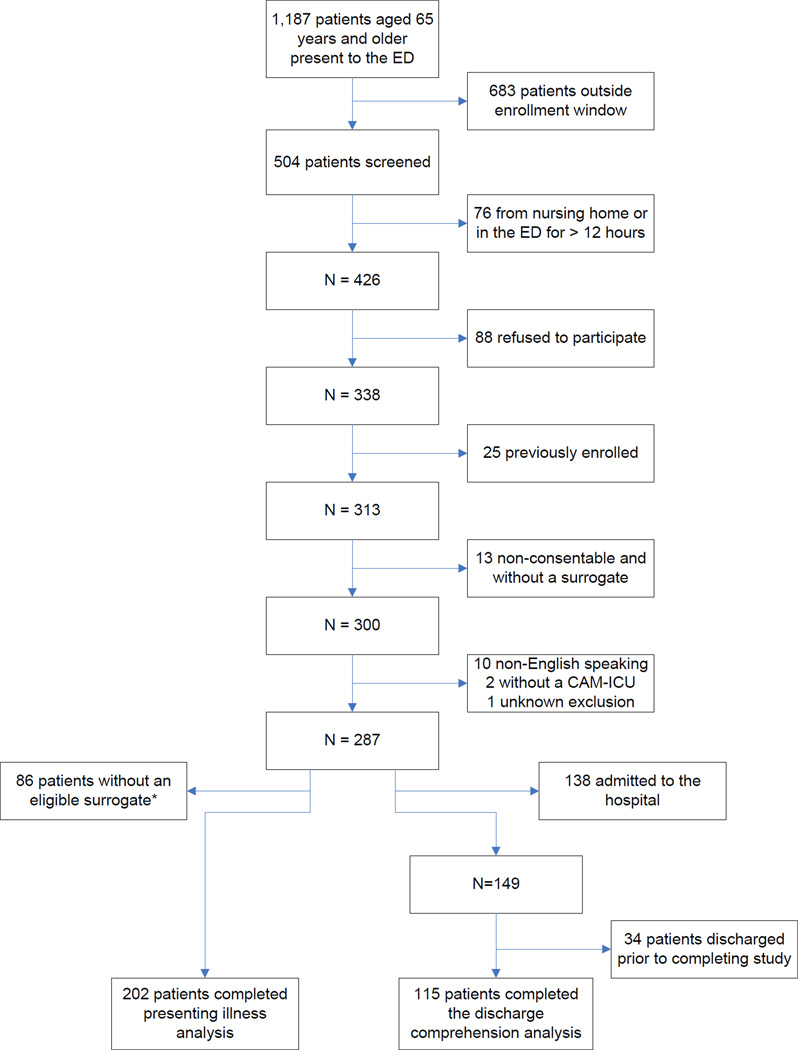
During the study period, 1,187 potentially eligible patients aged 65 years and older presented to the ED, 504 were screened, and 287 were enrolled and participated in either the presenting illness or discharge instruction comprehension surveys (Figure). The median age was similar between enrolled and all potentially eligible older patients (Table 1). Enrolled patients were more likely to be female and have an Emergency Severity Index of 3, and were less likely to be admitted to the hospital compared with all potentially eligible older patients (Table 1). Of the 287 patients who were enrolled, 74 (25.8%) patients met criteria for delirium, and of these 73 (98.6%) had a RASS of −1 (drowsy) or +1 (anxious) indicating that these patients had subtle symptomatology. In addition, 134 (46.7%) met criteria for dementia, but only 18 (13.4%) patients had a previous diagnosis of dementia documented in the medical record.
Figure 1.
Patient flow according to inclusion and exclusion criteria. The combined total of patients who participated in the presenting illness and discharge instruction comprehension components of the study did not equal 287 because some participated in both studies. *Eligible surrogates are those who were present in the emergency department and knew the reason why patient was in the emergency department. ED, Emergency department; CAM-ICU, Confusion Assessment Method for the Intensive Care Unit.
Table 1.
Comparison of patient demographics, emergency severity index and disposition of enrolled patients and all older patients who presented to the emergency department during the study period. Continuous variables are represented as median (interquartile range), and categorical variables are represented as absolute number (proportion). IQR, interquartile range.
| Variable | Enrolled Patients N=287 |
All Older Patients Seen in the ED N=1,187 |
|---|---|---|
| Age, median (IQR) | 74 (69, 81) | 75 (69, 82) |
| Female | 170 (59.2) | 660 (55.6) |
| Emergency Severity Index | ||
| 1 | 0 (0.0) | 59 (5.0) |
| 2 | 165 (57.5) | 704 (59.3) |
| 3 | 110 (39.0) | 368 (31.0) |
| 4 | 10 (3.5) | 46 (3.9) |
| 5 | 0 (0.0) | 5 (0.42) |
| Unknown | 0 (0.0) | 5 (0.42) |
| Admitted to hospital | 138 (48.1) | 672 (56.6) |
For the accuracy of the presenting complaint analysis, 85 patients did not have an eligible surrogate present in the ED, and 202 patients completed this portion of the study. Patients who completed the presenting illness survey were more likely to have delirium, dementia, be hearing impaired, live with others, and be admitted to the hospital compared with those who did not complete the survey (Table 2). Patients who completed the presenting illness analysis were also less likely to have adequate health literacy and less likely to have a college or graduate degree (Table 2). Of those who completed the presenting illness analysis, 66 (32.7%) had no cognitive impairment, 31 (15.4%) had delirium only, 64 (31.7%) had dementia only, and 41 (20.3%) had delirium superimposed on dementia. The weighted kappa between the raters was 0.71 indicating good agreement (Appendix Table C1). The median (IQR) presenting illness concordance scores were 4.5 (4.0, 5.0) for the no cognitive impairment group, 4.0 (2.5, 4.5) for the delirium only group, 4.5 (4.0, 5.0) for the dementia only group, and 3.0 (1.0, 4.5) for the delirium superimposed on dementia group. Sixty (90.9%) patients without cognitive impairment, 23 (74.2%) with delirium only, 58 (90.6%) with dementia only, and 21 (51.2%) with delirium superimposed on dementia had a presenting illness concordance score greater than or equal to 3 (partial concordance). After adjusting for age, health literacy, education, non-white race, and hearing impairment (Table 3), patients with delirium only and delirium superimposed on dementia were less likely to agree with their surrogates with regard to why they were in the ED.
Table 2.
Patient demographics and characteristics between patients who completed and did not complete presenting illness (PI) analysis. Patients who did not complete the PI survey did not have an adult surrogate who was knowledgeable of the patient’s condition in the ED. Continuous variables are represented as median (interquartile range), and categorical variables are represented as absolute number (proportion).
| Variable | PI Completed N=202 |
PI not completed N = 85 |
|---|---|---|
| Median Age (IQR) | 75 (70, 81) | 74 (68, 80) |
| Female | 118 (58.4) | 52 (61.2) |
| Non-white | 33 (16.3) | 21 (24.7) |
| Delirium | 72 (35.6) | 2 (2.4) |
| Dementia | 105 (52.0) | 29 (34.1) |
| Hearing impaired | 97 (48.0) | 33 (38.8) |
| Place of residence | ||
| Home alone | 36 (17.8) | 29 (34.1) |
| Home with others | 156 (77.2) | 48 (56.5) |
| Assisted living | 7 (3.5) | 5 (5.9) |
| Rehabilitation | 3 (1.5) | 3 (3.5) |
| Health Literacy Question* | ||
| 0 – Never | 56 (27.7) | 49 (57.7) |
| 1 – A little of the time | 4 (2.0) | 0 (0.00) |
| 2 – Some of the time | 2 (1.0) | 1 (1.2) |
| 3 – Most of the time | 8 (4.0) | 5 (5.9) |
| 4 – All the time | 132 (65.4) | 30 (35.3) |
| Education | ||
| Elementary | 12 (5.9) | 3 (3.5) |
| Middle School | 17 (8.4) | 7 (8.2) |
| High School | 105 (52.0) | 25 (29.4) |
| College | 52 (25.7) | 37 (43.5) |
| Graduate School and higher | 16 (7.9) | 13 (15.3) |
| Admitted | 108 (53.5) | 30 (35.3) |
Health literacy was determined by "How often do you have someone (like a family member, friend, hospital / clinic worker, caregiver) help you read hospital materials? "; IQR, interquartile range.
Table 3.
Proportional odds logistic regression model for the analysis of the accuracy of the patient’s presenting complaint. Proportion odds ratios and their 95% confidence intervals for each delirium-dementia category are reported. Patients with no cognitive impairment were the reference group. A proportional odds ratio less than 1 indicates that patients were less likely to agree with their surrogate with regards to why they were in the ED.
| Variables | Proportion Odds Ratio (95% Confidence interval) |
|---|---|
| Cognitive impairment | |
| No cognitive impairment | Reference |
| Delirium only | 0.42 (0.19 – 0.93) |
| Dementia only | 1.40 (0.72 – 2.70) |
| Delirium superimposed on dementia | 0.20 (0.09 – 0.43) |
| Age | 0.95 (0.92 – 0.99) |
| Health Literacy | 0.93 (0.81 – 1.08) |
| Education | 0.81 (0.61 – 1.08) |
| Non-white race | 0.75 (0.38 – 1.50) |
| Hearing impairment | 1.13 (0.66 – 1.92) |
One hundred forty nine patients were discharged from the ED, but 34 patients were discharged prior to completing the discharge instruction comprehension interview. As a result, 115 patients participated in this analysis. Patients who completed the discharge instruction comprehension survey were more likely to be hearing impaired and less likely to have adequate health literacy (Table 4) compared with those who did not complete the survey. The weighted kappa between the two raters ranged from 0.51 – 0.71 for all the domains tested, indicating moderate to good agreement (Appendix Tables C2 – C4). Patients with delirium superimposed on dementia had consistently poorer comprehension their discharge diagnosis, return to the ED instructions, and follow-up instructions compared with patients without any cognitive impairment (Table 5). After adjusting for age, health literacy, education, non-white race, and hearing impairment, delirium superimposed on dementia remained associated with poor comprehension of all three discharge domains (Table 6).
Table 4.
Patient demographics and characteristics between patients who completed and did not complete discharge instruction comprehension interview (DCI). Patients who did not complete the DCI were discharged prior to the interview. Continuous variables are represented as median (interquartile range), and categorical variables are represented as absolute number (proportion).
| Variable | DCI Completed N=115 |
DCI Not Completed N = 34 |
|---|---|---|
| Median Age (IQR) | 73 (69, 81) | 75 (69, 77) |
| Female | 68 (59.1) | 23 (67.7) |
| Non-white | 28 (24.4) | 7 (20.6) |
| Delirium | 21 (18.3) | 5 (14.7) |
| Dementia | 51 (44.4) | 13 (38.2) |
| Hearing impaired | 49 (42.6) | 8 (23.5) |
| Place of residence | ||
| Home alone | 27 (23.5) | 12 (35.3) |
| Home with others | 82 (71.3) | 20 (58.8) |
| Assisted living | 5 (4.4) | 1 (2.9) |
| Rehabilitation | 1 (0.9) | 1 (2.9) |
| Health Literacy Question* | ||
| 0 – Never | 46 (40.0) | 18 (52.9) |
| 1 – A little of the time | 2 (1.7) | 0 (0.0) |
| 2 – Some of the time | 1 (0.9) | 0 (0.0) |
| 3 – Most of the time | 4 (3.5) | 2 (5.9) |
| 4 – All the time | 62 (53.9) | 14 (41.2) |
| Education | ||
| Elementary | 6 (5.2) | 0 (0.0) |
| Middle School | 7 (6.1) | 3 (8.8) |
| High School | 51 (44.4) | 17 (50.0) |
| College | 35 (30.4) | 10 (29.4) |
| Graduate School and higher | 16 (13.9) | 4 (11.8) |
Health literacy was determined by "How often do you have someone (like a family member, friend, hospital / clinic worker, caregiver) help you read hospital materials?”; IQR, interquartile range.
Table 5.
Patient’s level of understanding ratings are expressed in median (interquartile ranges) and the total number (%) of patients with a concordance score greater than and equal to 3 for each discharge instruction domain. The ratings were determined by two reviewers using the printed discharge instructions as the reference standard. A five-point (1 – 5) scale was used with a lower score indicating decreased understanding of discharge instructions. The two reviewer’s score was averaged for this analysis.
| No cognitive impairment N=53 |
Delirium only N=11 |
Dementia only N=41 |
Delirium superimposed on dementia N=10 |
|
|---|---|---|---|---|
| Discharge diagnosis | ||||
| Median (IQR) | 4.5 (4.0, 5.0) | 4.5 (3.5, 5.0) | 4.5 (3.0, 5.0) | 2.8 (1.0, 4.0) |
| N (%) Concordance Score ≥ 3 | 46 (86.8) | 9 (81.8) | 33 (80.5) | 5 (50.0) |
| Return instructions to the ED | ||||
| Median (IQR) | 2.5 (1.0, 3.5) | 1.0 (1.0, 2.5) | 1.0 (1.0, 3.0) | 1.0 (1.0, 1.5) |
| N (%) Concordance Score ≥ 3 | 26 (49.1) | 1 (9.1) | 2.0 11 (26.8) | 1 (10.0) |
| Follow-up instructions | ||||
| Median (IQR) | 3.5 (3.0, 4.5) | 4.0 (2.5 – 5.0) | 3.0 (2.5, 3.5) | 1.5 (1.0, 3.0) |
| N (%) Concordance Score ≥ 3 | 43 (81.1) | 9 (81.8) | 30 (73.2) | 3 (30.0) |
Table 6.
Multivariable proportional logistic regression models to determine if cognitive impairment is associated with decreased comprehension of emergency department discharge instructions adjusted for health literacy, education, non-white race, and hearing impairment. Proportional odds ratios with their 95% confidence intervals are reported. A proportional odds ratio less than 1.00 is indicative of decreased comprehension.
| Variables | Proportion Odds Ratio (95% Confidence interval) |
|
|---|---|---|
| Discharge Diagnosis | Cognitive impairment | |
| No cognitive impairment | Reference | |
| Delirium only | 0.94 (0.27 – 3.28) | |
| Dementia only | 0.72 (0.33 – 1.60) | |
| Delirium superimposed on dementia | 0.13 (0.04 – 0.47) | |
| Age | 1.00 (0.95 – 1.05) | |
| Health Literacy | 0.95 (0.79 – 1.13) | |
| Education | 1.20 (0.84 – 1.73). | |
| Non-white race | 0.37 (0.17 – 0.83) | |
| Hearing impairment | 1.15 (0.55 – 2.40) | |
| Return to ED Instructions | Cognitive impairment | |
| No cognitive impairment | Reference | |
| Delirium only | 0.39 (0.10 – 1.57) | |
| Dementia only | 0.58 (0.26 – 1.32) | |
| Delirium superimposed on dementia | 0.18 (0.04 – 0.82) | |
| Age | 0.94 (0.89 – 0.99) | |
| Health Literacy | 1.01 (0.84 – 1.22) | |
| Education | 1.34 (0.91 – 1.98) | |
| Non-white race | 0.65 (0.27 – 1.57) | |
| Hearing impairment | 2.03 (0.91 – 4.51) | |
| Follow-up Instructions | Cognitive impairment | |
| No cognitive impairment | Reference | |
| Delirium only | 2.23 (0.65 – 7.64) | |
| Dementia only | 0.56 (0.26 – 1.21) | |
| Delirium superimposed on dementia | 0.09 (0.02 – 0.35) | |
| Age | 1.02 (0.98 – 1.08) | |
| Health Literacy | 0.74 (0.62 – 0.89) | |
| Education | 0.89 (0.63 – 1.27) | |
| Non-white race | 0.50 (0.23 – 1.10) | |
| Hearing impairment | 1.00 (0.49 – 2.06) | |
For all multivariable models, the Pearson Chi-squared test provided p-values ranging from 0.632 to 0.975 indicating that there was no proof of any lack-of-fit. The condition indices were less than 10 for all multivariable models, indicating no evidence of substantial collinearity among the covariates.
Limitations
We used the surrogate as the reference standard to determine the accuracy of the presenting complaint. We did not measure surrogates’ cognitive function or assess cohabitation status, and may have contributed to discordance between the patient and surrogate. However, 95% of the surrogates knew the patient for more than 10 years as this is a requirement to complete the IQCODE. Based on clinical experience, most surrogates were patients’ adult offspring. These factors likely mitigated this source of bias. Future studies will measure the surrogate's cognitive status, relationship to patient, and cohabitation status to assess the effect of these potential confounders.
Misclassification bias may have occurred. Though widely used, the MMSE, IQCODE, and CAM-ICU have not been formally validated in the ED setting. Formal neuropsychiatric testing, which is considered the gold standard for delirium and dementia diagnosis, was not performed because it would have not have been feasible for this study. Such assessments are time consuming and even for neuropsychiatrists, the diagnosis of dementia can be difficult in the presence of delirium. Additionally, delirium was measured at enrollment, and the discharge instruction comprehension interview occurred prior to discharge. It is possible that the patient who was initially non-delirious could have developed delirium later in the ED course prior to discharge. Conversely, a patient who was delirious at enrollment may not have been delirious at discharge. However, these potential circumstances would have likely biased our findings towards the null.
There are several sources of selection bias. This was a convenience sample and there were slight differences between our enrolled patients and all older ED patients who presented during the study period. Our delirium and dementia rate was higher than previously reported, and it is possible that patients with cognitive impairment may have been inadvertently oversampled. Additionally, eligible patients who completed and did not complete the presenting illness or discharge instruction comprehension surveys were slightly different; we attempted to mitigate these differences using multivariable modeling.
It is also possible that emergency physicians and nurses may have preferentially avoided giving discharge instructions to patients with cognitive impairment. However, this is unlikely to be the case since delirium and dementia are unrecognized by emergency physicians in over 75% of the cases7, 32 particularly when symptoms are subtle as was the case in this study.
Our sample was relatively small and limited the number of covariates we could account for in the model. Potentially important confounders such as home medications, comorbidity burden, severity of illness, and psychoactive medications given in the ED were excluded from the multivariable models. We also used a screening question to assess for health literacy to maintain study feasibility and may not have adequately adjusted for health literacy in the multivariable model. Future trials should utilize a more formal measure of health literacy such as the Test of Functional Health Literacy in Adults (TOFHLA) or Rapid Estimate of Adult Literacy in Medicine (REALM).33,34 Lastly, our study was conducted at a single center and may have limited generalizability in rural and non-academic centers.
Discussion
To our knowledge, this study is the first to investigate the effects of delirium and dementia on patients’ ability to accurately provide the primary reasons why they are in the ED and their ability to comprehend their ED discharge instructions. We observed that patients with delirium only and those with delirium superimposed on dementia were more likely to have difficulty in accurately stating their presenting complaint. In addition, patients with delirium superimposed on dementia were less likely to understand their discharge diagnosis, return to ED instructions, and follow-up instructions. These findings pose a significant patient safety concern, which will be magnified as the elderly population grows exponentially over the next several decades.20 Emergency physicians should be aware of this and potentially take steps to address cognition more routinely among the elderly seeking care.
Having an accurate understanding of why the patient is in the ED is fundamental to delivering appropriate and timely care. An inaccurate history may lead to inadequate diagnostic workups and delayed or even missed diagnoses, which can lead to adverse events and malpractice claims.35 Similarly, such communication breakdowns may result in unnecessary or even dangerous diagnostic testing and inappropriate disposition decisions.36 Indeed, if the patient is cognitively impaired, emergency physicians should attempt to corroborate the presenting complaint from other sources such as a family member. If a cognitively impaired patient is alone in the ED, an attempt to contact a surrogate by phone should be made.
Perhaps the most vital and novel piece of this investigation was the assessment of the role of cognitive impairment on ED discharge instruction comprehension in older patients. Previous studies investigating ED discharge instruction comprehension have enrolled a general ED cohort and have not examined the effect of delirium or dementia in particular.13, 14, 37 Poor comprehension of discharge instructions may contribute to non-compliance,13 potentially avoidable return ED visits, and a heightened mortality risk.7, 38 In this study, only patients with delirium superimposed on dementia demonstrated poorer comprehension of ED discharge instructions. However, most of the adjusted PORs for the delirium only and dementia only subgroups were less than 1.00. For many point estimates, the upper limits of their 95%CIs were slightly above 1.00 and the lack of precision may have been secondary to a type II error. Larger studies are needed not only to confirm these findings, but to investigate how the presence of delirium or dementia alone can contribute to poor discharge instruction comprehension.
Our results suggest that missing delirium and dementia in the ED may be a safety hazard. Based upon recent a study, emergency physicians miss 75% of patients with delirium.32 Similarly, dementia is also frequently missed especially if it is not previously documented in the medical record.7 In our study, dementia was only documented in 13.4% of the cases. Similar findings have been observed in the inpatient and primary care settings.39, 40 Such high “miss” rates occur because delirium and dementia are not routinely screened for in any clinical setting, especially in the ED. The Confusion Assessment Method and MMSE are commonly used assessments to detect delirium and dementia, respectively.23, 27, 41–44 However, these assessments can take up to 10 minutes to perform, limiting their feasibility in the demanding ED environment. The Six-Item Screener and Mini-Cog are brief cognitive impairment screens that have been validated in the ED setting.45–47 Though these screening tests do not differentiate between delirium and dementia, they may be sufficient to identify older ED patients at high risk for providing unreliable histories and having poor discharge instruction comprehension. However, optimal strategies for delirium and dementia surveillance in the ED setting must continue to be developed.21 Fortunately, such strategies are currently being investigated through NIH-sponsored investigations.
Several additional uncertainties remain with regard to the effects of cognitive impairment in the ED. Future studies are needed to determine if providing an inaccurate presenting complaint and poor ED discharge instruction comprehension alter the trajectory of care and lead to subsequent adverse patient outcomes in the ED and long-term. In addition, we did not assess the ability of caregivers to comprehend the patients’ discharge instructions. Because they most likely play a significant role in the older patient's home medical care, measuring their ability to understand ED discharge instructions and how it affects outcomes must also be elucidated in future studies. Lastly, interventions that are designed to improve discharge instruction comprehension in cognitively impaired older ED patients must also be developed. These interventions may be as simple as increasing the involvement of a cognitively intact family member or other caregiver in the home medical care. It is possible, however, that more intense interventions such as social worker, case manager or nurse involvement and home visitations may be required. Such interventions should be tested by randomized control trials and designed to help determine if they are cost-effective in improving the quality of emergency geriatric care and patient outcomes.
Conclusion
Older patients with delirium superimposed on dementia were less likely to accurately provide the reason of why they were in the ED and had decreased comprehension of ED discharge instructions. Cognitive impairment thus poses a heightened risk for important types of communication breakdown that may lead to very relevant patient safety hazards. Future studies with larger sample sizes are needed to confirm these findings and to determine how they affect patient care and outcomes. The potential to screen patients in the ED for the presence of cognitive impairment offers a viable and modifiable solution to this currently “invisible” hazard for both patients and ED healthcare professionals.
Acknowledgments
Dr. Han received support from the Vanderbilt Physicians Scientist Development grant. Dr. Bryce received support from the Emergency Medicine Foundation Medical Student Grant. Dr. Ely was supported in part by the National Institutes of Health AG27472 and the Veteran Affairs MERIT grant. Dr. Kripalani receives support from a K23 Mentored Patient Oriented Career Development Award (K23 HL077597).
APPENDICES
Appendix A. History of present illness survey
Patient Question: What is the main reason you are here in the emergency room today?
Surrogate Question: What is the main reason your [relationship to the patient] is here in the emergency room today?
Appendix B. Discharge Instruction Comprehension Interview
Did the emergency physician say what was wrong with you? Did they tell you why you having your symptoms? If yes, what did they say?
Did they tell you return to the ED for any reasons? If so, what reasons?
Did they ask you to follow-up with another doctor? If yes, what kind of doctor and how soon?
Appendix C. The four multivariable regression models with the degrees of freedoms used
| Presenting illness concordance = | Cognitive Impairment + Age + Delirium + Dementia + Education + Health Literacy + Non-white + Hearing Impairment |
| Discharge diagnosis comprehension = | Cognitive Impairment + Age + Delirium + Dementia + Education + Health Literacy + Non-white + Hearing Impairment |
| Return to ED instruction comprehension = | Cognitive Impairment + Age + Delirium + Dementia + Education + Health Literacy + Non-white + Hearing Impairment |
| Follow-up instruction comprehension = | Cognitive Impairment + Age + Delirium + Dementia + Education + Health Literacy + Non-white + Hearing Impairment |
Because the dependent variables were non-normally distributed, proportional odds logistic regression was used. The covariates were selected a priori based upon expert opinion. No interactions terms were incorporated. Cognitive impairment was categorized as: (1) no cognitive impairment, (2) delirium only, (3) dementia only, or (4) delirium superimposed on dementia. No cognitive impairment was the reference standard. Each multivariable model used 8 degrees of freedom.
Appendix C. Level of Agreement of concordance scores between two reviewers
Table C1.
Level of agreement in presenting illness concordance ratings between two reviewers represented as count data. Concordance ratings were the following: 1 - no concordance / understanding, 2 - minimal concordance / understanding, 3 - partial concordance / understanding, and 4 - very good concordance / understanding, and 5 - complete concordance / understanding.
| Reviewer 2 Concordance Ratings |
||||||
|---|---|---|---|---|---|---|
| Reviewer 1 Concordance Ratings | 1 | 2 | 3 | 4 | 5 | |
| 1 | 19 | 5 | 0 | 0 | 0 | |
| 2 | 0 | 8 | 4 | 1 | 0 | |
| 3 | 1 | 3 | 9 | 10 | 5 | |
| 4 | 0 | 2 | 6 | 29 | 16 | |
| 5 | 0 | 2 | 2 | 10 | 70 | |
| Weighted Kappa = 0.71 | ||||||
Table C2.
Level of agreement in discharge diagnosis comprehension concordance ratings between two reviewers represented as count data. Concordance ratings were the following: 1 - no concordance / understanding, 2 - minimal concordance / understanding, 3 - partial concordance / understanding, and 4 - very good concordance / understanding, and 5 - complete concordance / understanding.
| Reviewer 2 Concordance Ratings |
||||||
|---|---|---|---|---|---|---|
| Reviewer 1 Concordance Ratings | 1 | 2 | 3 | 4 | 5 | |
| 1 | 6 | 4 | 0 | 2 | 0 | |
| 2 | 0 | 9 | 1 | 0 | 0 | |
| 3 | 0 | 0 | 2 | 3 | 0 | |
| 4 | 0 | 0 | 6 | 9 | 4 | |
| 5 | 2 | 0 | 4 | 22 | 41 | |
| Weighted Kappa = 0.61 | ||||||
Table C3.
Level of agreement in discharge diagnosis comprehension concordance ratings between two reviewers represented as count data. Concordance ratings were the following: 1 - no concordance / understanding, 2 - minimal concordance / understanding, 3 - partial concordance / understanding, and 4 - very good concordance / understanding, and 5 - complete concordance / understanding.
| Reviewer 2 Concordance Ratings |
||||||
|---|---|---|---|---|---|---|
| Reviewer 1 Concordance Ratings | 1 | 2 | 3 | 4 | 5 | |
| 1 | 56 | 2 | 2 | 0 | 0 | |
| 2 | 3 | 1 | 7 | 1 | 1 | |
| 3 | 0 | 3 | 17 | 6 | 2 | |
| 4 | 2 | 0 | 0 | 7 | 2 | |
| 5 | 0 | 0 | 0 | 2 | 1 | |
| Weighed Kappa = 0.71 | ||||||
Table C4.
Level of agreement in discharge diagnosis comprehension concordance ratings between two reviewers represented as count data. Concordance ratings were the following: 1 - no concordance / understanding, 2 - minimal concordance / understanding, 3 - partial concordance / understanding, and 4 - very good concordance / understanding, and 5 - complete concordance / understanding.
| Reviewer 2 Concordance Ratings |
||||||
|---|---|---|---|---|---|---|
| Reviewer 1 Concordance Ratings | 1 | 2 | 3 | 4 | 5 | |
| 1 | 7 | 5 | 3 | 0 | 0 | |
| 2 | 4 | 4 | 5 | 2 | 3 | |
| 3 | 1 | 8 | 19 | 11 | 2 | |
| 4 | 0 | 2 | 0 | 6 | 0 | |
| 5 | 0 | 0 | 5 | 11 | 17 | |
| Weighed Kappa = 0.51 | ||||||
Footnotes
These were poster presentations at the American College of Emergency Physicians Research Forum on 10/2009 (Boston, MA) and the Society of Academic Emergency Medicine National Meeting on 6/2010 (Phoenix, AZ).
References
- 1.Rowland K, Maitra AK, Richardson DA, et al. The discharge of elderly patients from an accident and emergency department: functional changes and risk of readmission. Age Ageing. 1990;19:415–418. doi: 10.1093/ageing/19.6.415. [DOI] [PubMed] [Google Scholar]
- 2.Rosenfeld T, Fahey P, Price M, et al. The fate of elderly patients discharged from the accident and emergency department of a general teaching hospital. Community Health Stud. 1990;14:365–372. doi: 10.1111/j.1753-6405.1990.tb00047.x. [DOI] [PubMed] [Google Scholar]
- 3.Richardson DB. Elderly patients in the emergency department: a prospective study of characteristics and outcome. Med J Aust. 1992;157:234–239. doi: 10.5694/j.1326-5377.1992.tb137125.x. [DOI] [PubMed] [Google Scholar]
- 4.Chin MH, Jin L, Karrison TG, et al. Older patients' health-related quality of life around an episode of emergency illness. Ann Emerg Med. 1999;34:595–603. doi: 10.1016/s0196-0644(99)70161-7. [DOI] [PubMed] [Google Scholar]
- 5.Hastings SN, Schmader KE, Sloane RJ, et al. Adverse health outcomes after discharge from the emergency department--incidence and risk factors in a veteran population. J Gen Intern Med. 2007;22:1527–1531. doi: 10.1007/s11606-007-0343-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hastings SN, Oddone EZ, Fillenbaum G, et al. Frequency and predictors of adverse health outcomes in older Medicare beneficiaries discharged from the emergency department. Med Care. 2008;46:771–777. doi: 10.1097/MLR.0b013e3181791a2d. [DOI] [PubMed] [Google Scholar]
- 7.Hustey FM, Meldon SW, Smith MD, et al. The effect of mental status screening on the care of elderly emergency department patients. Ann Emerg Med. 2003;41:678–684. doi: 10.1067/mem.2003.152. [DOI] [PubMed] [Google Scholar]
- 8.Liptzin B, Levkoff SE. An empirical study of delirium subtypes. Br J Psychiatry. 1992;161:843–845. doi: 10.1192/bjp.161.6.843. [DOI] [PubMed] [Google Scholar]
- 9.Naughton BJ, Moran MB, Kadah H, et al. Delirium and other cognitive impairment in older adults in an emergency department. Ann Emerg Med. 1995;25:751–755. doi: 10.1016/s0196-0644(95)70202-4. [DOI] [PubMed] [Google Scholar]
- 10.American Psychiatric Association., American Psychiatric Association. Diagnostic and statistical manual of mental disorders : DSM-IV. 4th ed. Washington, DC: American Psychiatric Association; 1994. Task Force on DSM-IV. [Google Scholar]
- 11.Hogan TM, Losman ED, Carpenter CR, et al. Development of geriatric competencies for emergency medicine residents using an expert consensus process. Acad Emerg Med. 2010;17:316–324. doi: 10.1111/j.1553-2712.2010.00684.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Terrell KM, Hustey FM, Hwang U, et al. Quality indicators for geriatric emergency care. Acad Emerg Med. 2009;16:441–449. doi: 10.1111/j.1553-2712.2009.00382.x. [DOI] [PubMed] [Google Scholar]
- 13.Clarke C, Friedman SM, Shi K, et al. Emergency department discharge instructions comprehension and compliance study. CJEM. 2005;7:5–11. doi: 10.1017/s1481803500012860. [DOI] [PubMed] [Google Scholar]
- 14.Spandorfer JM, Karras DJ, Hughes LA, et al. Comprehension of discharge instructions by patients in an urban emergency department. Ann Emerg Med. 1995;25:71–74. doi: 10.1016/s0196-0644(95)70358-6. [DOI] [PubMed] [Google Scholar]
- 15.Han JH, Shintani A, Eden S, et al. Delirium in the emergency department: an Independent predictor of death within 6 months. Ann Emerg Med. 2010 doi: 10.1016/j.annemergmed.2010.03.003. (In Press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ely EW, Shintani A, Truman B, et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA. 2004;291:1753–1762. doi: 10.1001/jama.291.14.1753. [DOI] [PubMed] [Google Scholar]
- 17.McCusker J, Cole M, Abrahamowicz M, et al. Delirium predicts 12-month mortality. Arch Intern Med. 2002;162:457–463. doi: 10.1001/archinte.162.4.457. [DOI] [PubMed] [Google Scholar]
- 18.Tschanz JT, Corcoran C, Skoog I, et al. Dementia: the leading predictor of death in a defined elderly population: the Cache County Study. Neurology. 2004;62:1156–1162. doi: 10.1212/01.wnl.0000118210.12660.c2. [DOI] [PubMed] [Google Scholar]
- 19.Pitts SR, Niska RW, Xu J, et al. National Hospital Ambulatory Medical Care Survey: 2006 emergency department summary. National Health Statistics Reports; No. 7. Hyattsville, MD: National Center for Health Statistics; 2008. [PubMed] [Google Scholar]
- 20.He W, Sengupta M, Velkoff VA, et al. U.S Census Bureau, Current Population Reports, P23-209, 65+ in the United States: 2005. U.S. Government Printing Office; 2005. [Google Scholar]
- 21.Carpenter CR, Gerson LW. Geriatric emergency medicine. In: LoCicero J III, Rosenthal RA, Katlic MR, et al., editors. A supplement to new frontiers in geriatrics research: an agenda for surgical and related medical specialties. New York: American Geriatrics Society; 2007. pp. 45–72. [Google Scholar]
- 22.Ely EW, Inouye SK, Bernard GR, et al. Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU) JAMA. 2001;286:2703–2710. doi: 10.1001/jama.286.21.2703. [DOI] [PubMed] [Google Scholar]
- 23.Inouye SK, van Dyck CH, Alessi CA, et al. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113:941–948. doi: 10.7326/0003-4819-113-12-941. [DOI] [PubMed] [Google Scholar]
- 24.Ely EW, Margolin R, Francis J, et al. Evaluation of delirium in critically ill patients: validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) Crit Care Med. 2001;29:1370–1379. doi: 10.1097/00003246-200107000-00012. [DOI] [PubMed] [Google Scholar]
- 25.Pandharipande P, Cotton BA, Shintani A, et al. Motoric subtypes of delirium in mechanically ventilated surgical and trauma intensive care unit patients. Intensive Care Med. 2007;33:1726–1731. doi: 10.1007/s00134-007-0687-y. [DOI] [PubMed] [Google Scholar]
- 26.Peterson JF, Pun BT, Dittus RS, et al. Delirium and its motoric subtypes: a study of 614 critically ill patients. J Am Geriatr Soc. 2006;54:479–484. doi: 10.1111/j.1532-5415.2005.00621.x. [DOI] [PubMed] [Google Scholar]
- 27.Folstein MF, Folstein SE, McHugh PR. "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 28.Jorm AF. A short form of the Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE): development and cross-validation. Psychol Med. 1994;24:145–153. doi: 10.1017/s003329170002691x. [DOI] [PubMed] [Google Scholar]
- 29.Hogervorst E, Combrinck M, Lapuerta P, et al. The Hopkins Verbal Learning Test and screening for dementia. Dement Geriatr Cogn Disord. 2002;13:13–20. doi: 10.1159/000048628. [DOI] [PubMed] [Google Scholar]
- 30.Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med. 2004;36:588–594. [PubMed] [Google Scholar]
- 31.Harrell FE. Regression modeling strategies : with applications to linear models, logistic regression, and survival analysis. New York: Springer; 2001. [Google Scholar]
- 32.Han JH, Zimmerman EE, Cutler N, et al. Delirium in older emergency department patients: recognition, risk factors, and psychomotor subtypes. Acad Emerg Med. 2009;16:193–200. doi: 10.1111/j.1553-2712.2008.00339.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Davis TC, Long SW, Jackson RH, et al. Rapid estimate of adult literacy in medicine: a shortened screening instrument. Fam Med. 1993;25:391–395. [PubMed] [Google Scholar]
- 34.Parker RM, Baker DW, Williams MV, et al. The test of functional health literacy in adults: a new instrument for measuring patients' literacy skills. J Gen Intern Med. 1995;10:537–541. doi: 10.1007/BF02640361. [DOI] [PubMed] [Google Scholar]
- 35.Kachalia A, Gandhi TK, Puopolo AL, et al. Missed and delayed diagnoses in the emergency department: a study of closed malpractice claims from 4 liability insurers. Ann Emerg Med. 2007;49:196–205. doi: 10.1016/j.annemergmed.2006.06.035. [DOI] [PubMed] [Google Scholar]
- 36.Sanders AB. Missed delirium in older emergency department patients: a quality-of-care problem. Ann Emerg Med. 2002;39:338–341. doi: 10.1067/mem.2002.122273. [DOI] [PubMed] [Google Scholar]
- 37.Engel KG, Heisler M, Smith DM, et al. Patient comprehension of emergency department care and instructions: are patients aware of when they do not understand? Ann Emerg Med. 2009;53:454–461. e415. doi: 10.1016/j.annemergmed.2008.05.016. [DOI] [PubMed] [Google Scholar]
- 38.Kakuma R, du Fort GG, Arsenault L, et al. Delirium in older emergency department patients discharged home: effect on survival. J Am Geriatr Soc. 2003;51:443–450. doi: 10.1046/j.1532-5415.2003.51151.x. [DOI] [PubMed] [Google Scholar]
- 39.Mackin RS, Arean PA. Incidence and documentation of cognitive impairment among older adults with severe mental illness in a community mental health setting. Am J Geriatr Psychiatry. 2009;17:75–82. doi: 10.1097/JGP.0b013e31818cd3e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Boustani M, Callahan CM, Unverzagt FW, et al. Implementing a screening and diagnosis program for dementia in primary care. J Gen Intern Med. 2005;20:572–577. doi: 10.1111/j.1525-1497.2005.0126.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Iracleous P, Nie JX, Tracy CS, et al. Primary care physicians' attitudes towards cognitive screening: findings from a national postal survey. Int J Geriatr Psychiatry. 2010;25:23–29. doi: 10.1002/gps.2293. [DOI] [PubMed] [Google Scholar]
- 42.Hatfield CF, Dudas RB, Dening T. Diagnostic tools for dementia. Maturitas. 2009;63:181–185. doi: 10.1016/j.maturitas.2009.03.005. [DOI] [PubMed] [Google Scholar]
- 43.Ismail Z, Rajji TK, Shulman KI. Brief cognitive screening instruments: an update. Int J Geriatr Psychiatry. 2010;25:111–120. doi: 10.1002/gps.2306. [DOI] [PubMed] [Google Scholar]
- 44.Milne A, Culverwell A, Guss R, et al. Screening for dementia in primary care: a review of the use, efficacy and quality of measures. Int Psychogeriatr. 2008;20:911–926. doi: 10.1017/S1041610208007394. [DOI] [PubMed] [Google Scholar]
- 45.Wilber ST, Lofgren SD, Mager TG, et al. An evaluation of two screening tools for cognitive impairment in older emergency department patients. Acad Emerg Med. 2005;12:612–616. doi: 10.1197/j.aem.2005.01.017. [DOI] [PubMed] [Google Scholar]
- 46.Carpenter CR, DesPain B, Keeling TN, et al. The six item screener and AD8 for the detection of cognitive impairment in geriatric emergency department patients. Ann Emerg Med. 2011;57:653–661. doi: 10.1016/j.annemergmed.2010.06.560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wilber ST, Carpenter CR, Hustey FM. The Six-Item Screener to detect cognitive impairment in older emergency department patients. Acad Emerg Med. 2008;15:613–616. doi: 10.1111/j.1553-2712.2008.00158.x. [DOI] [PubMed] [Google Scholar]