Abstract
Individuals with acute heart failure exacerbation often experience a deterioration in renal function. We sought to determine whether this deterioration is ischemic in nature and detectable by sensitive urine biomarkers neutrophil gelatinase-associated lipocalin (NGAL) and kidney injury molecule-1 (KIM-1). We measured serial biomarker levels and evaluated the associations of these biomarkers with renal recovery in a cohort of hospitalized patients with acute heart failure exacerbation.
Keywords: acute kidney injury, urine biomarkers, heart failure
Patients with acute heart failure (HF) exacerbation commonly experience a deterioration of renal function, manifested clinically as a rise in serum creatinine (SCr). This is often attributed to “pre-renal” physiology and is thought to be reversible. Whether this rise in SCr represents true kidney tubular injury is uncertain. Urine neutrophil gelatinase-associated lipocalin (NGAL) has been reported to be able to distinguish pre-renal azotemia from intrinsic kidney injury in hospitalized patients with established acute kidney injury (AKI).1 Kidney injury molecule- 1 (KIM-1) is elevated in pre-renal azotemia to a lesser extent than in more severe AKI (lasting more than 48 hours).2 Assessment of daily urine NGAL in patients with acute HF did not indicate significant tubular injury despite aggressive diuresis and clinical AKI in some.3 We evaluated the patterns of daily measurements of urine NGAL and KIM-1 in hospitalized individuals with HF exacerbation undergoing routine clinical care. We sought to determine whether elevations of these markers are associated with likelihood of recovery of kidney function in this population.
We recruited consecutive patients admitted for HF exacerbation from March 2–May 31, 2011 at one medical center, regardless of renal function. Our institution’s committee on human research gave approval for this study, and all participants gave informed consent. HF exacerbation was defined by clinical presentation as assessed by the admitting providers, and management of the patients including diuretic administration and other treatments was guided by the medical judgment of the hospital team. We collected daily urine samples (for 5 days) and measured urine NGAL (AntibodyShop) and KIM-1 (R&D Systems). Due to limited resources, the timing of urine collection relative to diuretic administration could not be standardized. AKI was defined by AKIN criteria.4 The primary outcome was recovery from AKI, defined as return to within 10% of the original SCr. Since it has been observed that the rise in SCr in individuals with HF often occurs due to decompensation of heart function and associated kidney dysfunction before the patient feels poorly enough to seek medical attention, we also assessed recovery in patients whose SCr rise had occurred prior to admission, ie, those admitted above baseline creatinine (ABL). We defined baseline creatinine as the most recent to the index hospitalization (excluding values within 7 days or older than 1 year).5
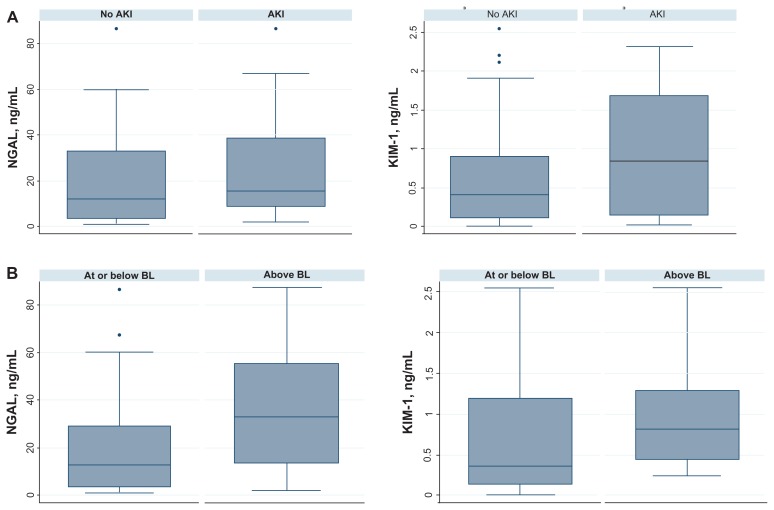
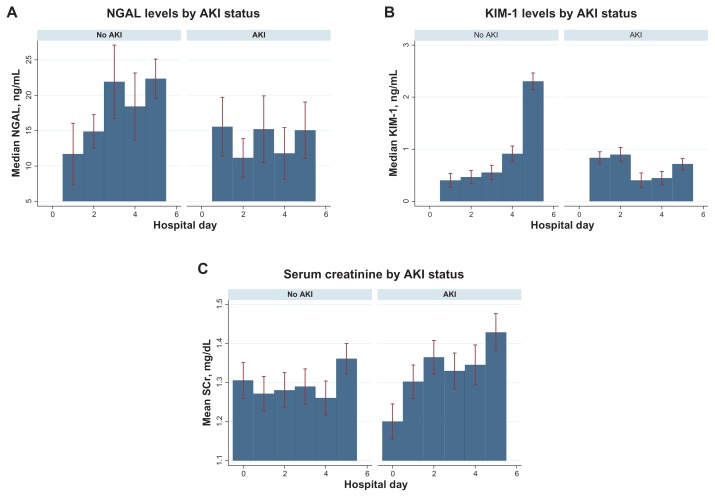
53 eligible patients were recruited. Mean age was 65; 30 were men; mean baseline creatinine was 1.2 mg/dL. 20 experienced AKI (9 recovered), 9 patients presented ABL (6 recovered), and 24 had no change in renal function. Mean NGAL and KIM-1 were similar in those without and with AKI (Fig. 1A) or who presented at or above baseline (Fig. 1B) (Table 1). In pooled logistic regression models, NGAL and KIM-1 were not associated with recovery from rise in SCr (odds ratio per standard deviation biomarker 0.72 (95% CI 0.21–2.5) and 0.78 (95% CI 0.36–1.69) respectively). NGAL and KIM-1 were correlated with each other (Spearman coefficient 0.53, P = 0.004). In contrast to NGAL, KIM-1 levels rose over the first 5 days of hospitalization in individuals with no AKI and stayed static in those who experienced AKI (Fig. 2A and B). This differed from the pattern of serum creatinine between groups (Fig. 2C). These patterns remained the same when both biomarkers were normalized to urine creatinine.
Figure 1.
(A) Box plots of day 1 biomarker levels by status of AKI during hospitalization. (B) Box plots of day 1 biomarker levels by status of creatinine at day of admission.
Table 1.
Mean (SE) level biomarker by absence v. presence of rise in creatinine during hospitalization and at admission.
| No AKI (N = 33) | AKI (N = 20) | P value | |
|---|---|---|---|
| NGAL/cr | 79.8 (26.3) | 91.0 (41.6) | 0.41 |
| NGAL | 43.4 (15.2) | 30.0 (8.4) | 0.74 |
| KIM-1/cr | 1.61 (0.13) | 1.41 (0.21) | 0.26 |
| KIM-1 | 0.82 (0.18) | 0.90 (0.17) | 0.39 |
| At baseline (N = 44) | ABL (N = 9) | Pvalue | |
|
| |||
| NGAL/cr | 76.2 (23.7) | 120.6 (64.1) | 0.23 |
| NGAL | 36.7 (10.7) | 66.3 (27.9) | 0.11 |
| KIM-1/cr | 1.34 (0.17) | 1.33 (0.25) | 0.51 |
| KIM-1 | 0.76 (0.13) | 1.27 (0.45) | 0.07 |
Notes: Units for NGAL and KIM-1 are ng/mL. Units for NGAL/cr and KIM-1/cr are ng/mg.
Abbreviations: AKI, acute kidney injury experienced during hospitalization; ABL, above baseline creatinine at admission.
Figure 2.
Levels of urine biomarkers and serum creatinine by status of AKI during hospitalization, by hospital day.
Note: Error bars represent 95% confidence intervals.
In this study, levels of urine NGAL and KIM-1 were not associated with recovery from rise in SCr in patients with HF exacerbation. A significant proportion of patients experienced deterioration of renal function before presentation to medical care (ABL), which may be attributable to venous congestion6 and may represent a different type of renal injury from that of the in-hospital AKI group. Limitations of our study include small sample size, lack of uniform administration of diuretics, and inability to evaluate tubular function.7 However, we found that patterns of NGAL and KIM-1 may differ with varying timing of HF exacerbation presentation. This may be due to differences in the type of kidney injury detectable by these biomarkers or in the responses of these markers to treatment. These differences should be evaluated in future studies.
Informed consent was granted by all involved patients and procedures were in accordance with the ethical standards of the responsible committee on human experimentation at our institution and with the Helsinki Declaration of 1975–2000.
Acknowledgements
The authors would like to thank Dr. Michael Bennett at Cincinnati Children’s Hospital, Brandon Imp, and the patients who participated in this study.
Footnotes
Author Contributions
Conceived and designed the experiments: MP, CYH. Analyzed the data: MP, EV. Wrote the first draft of the manuscript: MP. Contributed to the writing of the manuscript: EV, CYH, KDL, MGS. Agree with manuscript results and conclusions: MP, EV, KDL, MGS, CYH. Jointly developed the structure and arguments for the paper: MP, CYH, MGS. Made critical revisions and approved final version: MP, EV, KDL, MGS, CYH. All authors reviewed and approved of the final manuscript.
Competing Interests
KDL discloses consulting fees from Astute Biomedical, Cytopheryx, and Complexa, grants/ grants pending from NIH, donation of reagents from Abbott and CMIC, and holds shares in Amgen. Other authors disclose no competing interests.
Disclosures and Ethics
As a requirement of publication author(s) have provided to the publisher signed confirmation of compliance with legal and ethical obligations including but not limited to the following: authorship and contributorship, conflicts of interest, privacy and confidentiality and (where applicable) protection of human and animal research subjects. The authors have read and confirmed their agreement with the ICMJE authorship and conflict of interest criteria. The authors have also confirmed that this article is unique and not under consideration or published in any other publication, and that they have permission from rights holders to reproduce any copyrighted material. Any disclosures are made in this section. The external blind peer reviewers report no conflicts of interest.
Funding
This work was funded by Dr. Park’s University of California, San Francisco, Clinical and Translational Science Institute Clinical Research Services Young Investigators Pilot Award, NIH/NIDDK F32DK093231, and American Heart Association 11POST7230046 and Dr. Chi-yuan Hsu’s NIH/NIDDK K24 DK92291.
References
- 1.Singer E, Elger A, Elitok S, et al. Urinary neutrophil gelatinase-associated lipocalin distinguishes pre-renal from intrinsic renal failure and predicts outcomes. Kidney Int. 2011;80(4):405–14. doi: 10.1038/ki.2011.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nejat M, Pickering JW, Devarajan P, et al. Some biomarkers of acute kidney injury are increased in pre-renal acute injury. Kidney Int. 2012;81(12):1254–62. doi: 10.1038/ki.2012.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dupont M, Shrestha K, Singh D, et al. Lack of significant renal tubular injury despite acute kidney injury in acute decompensated heart failure. Eur J Heart Fail. 2012;14(6):597–604. doi: 10.1093/eurjhf/hfs039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mehta RL, Kellum JA, Shah SV, et al. Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit Care. 2007;11(2):R31. doi: 10.1186/cc5713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Siew ED, Matheny ME, Ikizler TA, et al. Commonly used surrogates for baseline renal function affect the classification and prognosis of acute kidney injury. Kidney Int. 2010;77(6):536–42. doi: 10.1038/ki.2009.479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tang WH, Mullens W. Cardiorenal syndrome in decompensated heart failure. Heart (British Cardiac Society) 2010;96(4):255–60. doi: 10.1136/hrt.2009.166256. [DOI] [PubMed] [Google Scholar]
- 7.Shrestha K, Shao Z, Singh D, Dupont M, Tang WH. Relation of systemic and urinary neutrophil gelatinase-associated lipocalin levels to different aspects of impaired renal function in patients with acute decompensated heart failure. Am J Cardiol. 2012;110(9):1329–35. doi: 10.1016/j.amjcard.2012.06.035. [DOI] [PMC free article] [PubMed] [Google Scholar]