Abstract
The virulence of Soromba-R, a Lassa virus strain recently isolated from southern Mali, was assessed in 2 animal models of Lassa fever: inbred strain 13 guinea pigs and cynomolgus macaques. In both models, the Malian isolate demonstrated tissue tropism and viral titers similar to those of historical Lassa virus isolates from Sierra Leone (Josiah) and Liberia (Z-132); however, the Soromba-R isolate was found to be less pathogenic, as determined by decreased mortality and prolonged time to euthanasia in macaques. Interestingly, in addition to the classic indicators of Lassa fever, Soromba-R infection presented with moderate to severe pulmonary manifestations in the macaque model. Analysis of host responses demonstrated increased immune activation in Soromba-R–infected macaques, particularly in neutrophil-activating or -potentiating proinflammatory cytokines or growth factors, including tumor necrosis factor α, macrophage inflammatory protein 1α, interleukin 1β, and granulocyte colony-stimulating factor, as well as interleukin 5, which may be responsible for the decreased lethality and uncharacteristic clinical presentation. These results suggest that the strain of Lassa virus circulating in Mali might be less pathogenic than strains circulating in the historical region of endemicity and may result in an atypical presentation for Lassa fever, which could complicate clinical diagnosis.
Keywords: Lassa fever, pathogenesis, disease modeling, guinea pigs, non-human primates, West Africa
Lassa fever (LF) is an acute viral illness associated with Lassa virus (LASV; family Arenaviridae, genus Arenavirus) infection. LF is endemic in the West African countries of Nigeria, Liberia, Guinea, and Sierra Leone, where it represents a major burden on healthcare systems, with up to 500 000 combined infections identified per annum [1–4]. Sporadic cases of LF have also been diagnosed from countries in close proximity to the LF-endemic regions, including a confirmed case suspected to have originated from Ghana, Cote d'Ivoire, or Burkina Faso and, more recently, a confirmed case from Mali, where LASV was shown to be enzootic [5–7].
In humans, exposure to LASV can result in a range of manifestations, from apparently asymptomatic infection to severe hemorrhagic fever disease with multiorgan failure [1]. In the LF-endemic region, LASV is associated with approximately 5000 deaths annually, representing an overall mortality rate of 1%–2% among infected individuals [4]. However, the mortality rate of LF among hospitalized cases increases to around 20%, and mortality rates exceeding 50% have been documented in outbreak scenarios [8, 9]. The remote locations where LASV is considered endemic, coupled with the risk of secondary transmission of LASV, has hindered clinical and pathological investigations into LF. As such, the pathogenesis of LF remains poorly understood [10].
Currently, 2 animal models have been described for studying LF: inbred (strain 13) guinea pigs and nonhuman primates (NHPs) [11]. While the inbred guinea pig model is useful as a screening model, the disease manifestations in this model do not recapitulate those seen in human cases; therefore, the preferred model for pathogenesis and vaccine or therapeutic studies is NHPs, most commonly rhesus or cynomolgus macaques. To date, the majority of studies conducted in NHPs have focused on infection with LASV strain Josiah [12–18]. The purpose of this study was to use the strain 13 guinea pig and cynomolgus macaque models of LF for infection with a recent LASV isolate from Mali and to compare potential differences in virulence with LASV strains from Liberia and Sierra Leone.
METHODS
Animal Work and Biosafety
Animal experiments were approved by the Institutional Animal Care and Use Committee of the Rocky Mountain Laboratories (RML) and were performed following the guidelines of the Association for Assessment and Accreditation of Laboratory Animal Care, International (AAALAC), by certified staff in an AAALAC-approved facility. Experiments were conducted in the biosafety level 4 (BSL-4) facility at the RML.
Viruses
Low-passage (defined as ≤4 passages) LASV isolates Josiah [19], Z-132 (which genetically is similar to LASV Z-148) [7, 20], and Soromba-R [7] were cultured in Vero cells and titered using standard median tissue culture infective dose (TCID50) methods.
In Vivo Infection (Strain 13 Guinea Pigs)
Twenty-one strain 13 guinea pigs (Cavia porcellus; age, 2–4 months) were infected with a TCID50 of 1 × 104 LASV Josiah, Z-132, or Soromba-R by intraperitoneal injection and were monitored daily for signs of illness (ie, abnormal activity, posture, and respiration; recumbency; and weight loss). Animals in the terminal stage of disease (weight loss of >15%, inability to move, and/or respiratory distress) were euthanized by exsanguination, and blood, liver, spleen, and lung samples were collected for pathological and virological analysis from 3 animals per group.
In Vivo Infection (Cynomolgus Macaques)
Nine cynomolgus macaques (Macaca fascicularis; age, 6–7 years; sex, 7 males and 2 females) were infected with 1 × 104 TCID50 of LASV Josiah, Z-132, or Soromba-R (3 animals per group) by intramuscular injection. Animals were monitored twice daily and assigned a numerical score based on clinical signs of disease (ie, fever; abnormal posture, respiration, feces/urine, food intake, attitude, and skin turgor; and recumbency), using an approved end point scoring sheet. On days −7, 0, 1, 3, 7, 10, and 14, animals were examined under anesthesia, at which point chest radiography was performed; pulse rate, blood pressure, temperature, and respiration rates were measured; and animals were bled for analysis of blood chemistry, coagulation parameters, differential blood count, virologic characteristics, and cytokine profiling. Animals were euthanized (by exsanguination while under deep anesthesia) when clinical signs indicated terminal disease (ie, a score of ≥30) [21], and a complete necropsy was performed, with collection of clinical specimens from nasal mucosa, oral mucosa, conjunctiva, tonsils, salivary gland, trachea, bronchi, right and left lung (upper, middle, and caudal lobes), lymph nodes (cervical, axillary, inguinal, and mesenteric) heart, liver, spleen, pancreas, jejunum, transverse colon, kidney, adrenal gland, testes/ovary, femoral bone marrow, urinary bladder, cervical spinal cord, and brain (stem, frontal, and cerebellum).
Hematological, Serum Biochemical, and Coagulation Parameters
Hematological, serum biochemical, and coagulation analyses were accomplished as previously described [18, 22, 23].
Serum Cytokine/Chemokine Analysis
Concentrations of granulocyte colony-stimulating factor (G-CSF), granulocyte macrophage colony-stimulating factor, interferon γ (IFN-γ), interleukin 1β (IL-1β), interleukin 1Rα, interleukin 2 (IL-2), interleukin 4, interleukin 5 (IL-5), interleukin 6 (IL-6), interleukin 8 (IL-8), interleukin 12/23 (IL-12/23), interleukin 13, interleukin 15, interleukin 17, interleukin 18, monocyte chemotactic protein 1 (MCP-1), macrophage inflammatory protein 1α (MIP-1α), macrophage inflammatory protein 1β, sCD-40L, tumor necrosis factor α (TNF-α), transforming growth factor α, and vascular endothelial growth factor were determined in serum samples, using a NHP cytokine kit (Millipore). Data were analyzed with 2-way analysis of variance (ANOVA) and a Bonferroni posttest comparing Soromba-R and Z-132 infection groups to Josiah.
Virus Detection/Titration
RNA was extracted from NHP blood samples by use of QIAamp viral RNA extraction kits (Qiagen) and was screened for the presence of LASV RNA as previously described [24]. Infectious LASV titers were determined in blood and tissue samples by a standard TCID50 assay on Vero cells (limit of detection, approximately 103 infectious particles/g). Viral titers were analyzed with 1-way ANOVA and the Tukey-Kramer posttest.
Histopathological and Immunohistochemical (IHC) Analysis
Tissues were inactivated and fixed with 10% formalin and processed according to standard methods and BSL-4 standard operating procedures. Thin sections were stained with hematoxylin and eosin or tested for viral antigen by IHC, using a monoclonal antibody against LASV GP2 (1:200 dilution, antibody L52-121-22; kindly provided by Dr Lisa Hensley, US Army Medical Research Institute of Infectious Diseases) [18] on a Discovery XT instrument (Ventana Medical Systems). Slides were blindly evaluated by a veterinary pathologist.
RESULTS AND DISCUSSION
LASV Infection in Inbred Guinea Pigs
LASV Josiah and Z-132 were uniformly lethal in inbred guinea pigs, with mean times to death of 20.7 days (range, 18–26 days) and 19.9 days (range, 17–23 days), respectively. In contrast, infection with LASV Soromba-R was lethal in 4 of 7 animals (57%), with a mean time to death of 20.8 days (range, 19–22 days; Figure 1A). The 3 survivors in the Soromba-R group were monitored until 55 days after infection, and although minor weight loss was noted, no other signs of disease were observed. Infection was confirmed in the survivors through identification of anti-LASV antibodies via recombinant nucleoprotein enzyme-linked immunosorbent assay [25].
Figure 1.
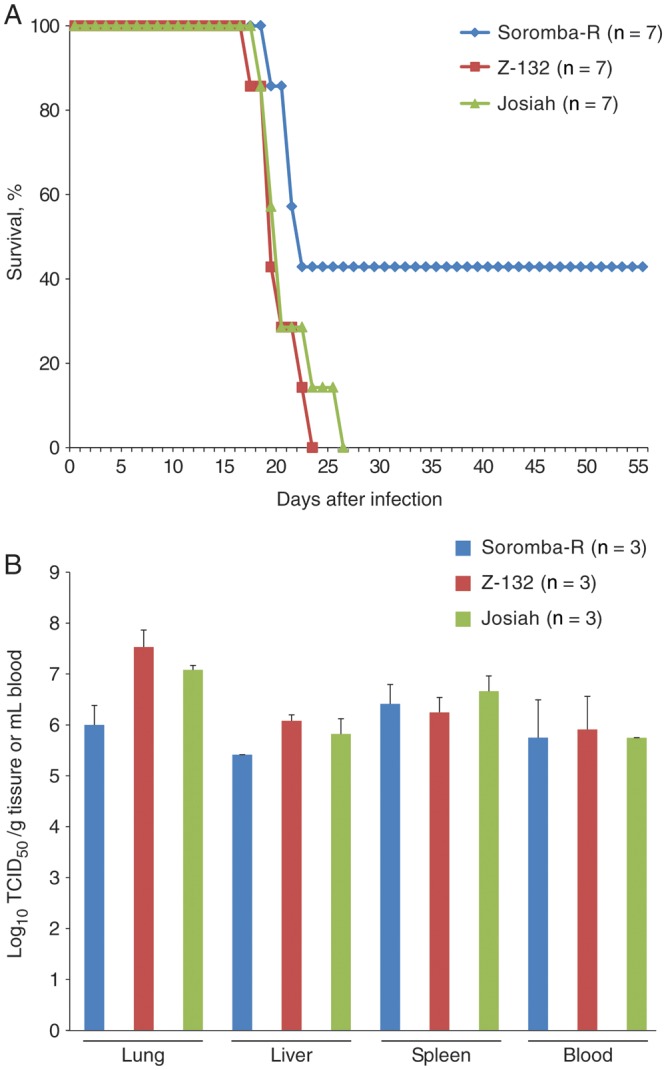
Lassa virus infection in strain 13 guinea pigs. Groups of 7 inbred guinea pigs were infected with a median tissue culture infective dose (TCID50) of 1 × 104 Lassa virus strain Josiah (green), Z-132 (red), or Soromba-R (blue). Soromba-R demonstrated decreased lethality in strain 13 guinea pigs (A), although disease progression and viral titers in organs of terminally ill animals (B) did not differ among the 3 groups. Error bars represent the standard error of the mean.
Viral titers in 3 organs (lung, liver, and spleen) and blood collected from terminally ill animals revealed similar, high levels of infectious LASV (Figure 1B), and IHC staining of tissues demonstrated little difference between the 3 infection groups. Macrophages and pneumocytes stained positive in lung samples, with minimal positivity noted in the endothelium. In the liver, the mesothelium frequently stained positive for LASV antigen and, to a lesser extent, periductal monocytes. Histological changes in lung, liver, and spleen samples were also similar and consistent across all 3 groups. Changes in the spleen were characterized by mild to moderate red pulp histiocytosis (hyperplasia of histiocytes/macrophages), with variable but fewer numbers of heterophils. Liver samples exhibited hepatocellular lipid degeneration, as well as mild to moderate lymphohistiocytic portal hepatitis, which appeared to be centered primarily on bile ductules. Moderate, multifocal, bronchointerstitial pneumonia, primarily histiocytic with fewer heterophils, was noted in lung samples. In addition, there was multifocal alveolar septae expanded by macrophages with abundant, vacuolated cytoplasms. Multifocal, mild, perivascular aggregates of lymphocytes were also noted, and the pleural mesothelium was hypertrophic. Representative lung and liver samples from a Soromba-R–infected guinea pig are shown in Supplementary Figure 1. To further analyze potential differences in virulence, disease progression was assessed in macaques, which are known to be the gold standard animal model for pathogenesis studies and for which more reagents are available.
Clinical Progression of LASV Infection in NHPs
Physical signs of infection were unremarkable in cynomolgus macaques until days 5–7 after infection, at which point animals demonstrated reduced food intake, decreased activity, mild depression, and piloerection (Figure 2A). Fever was noted in 5 animals infected with Josiah and Z-132 isolates and peaked between days 7 and 10 (peak temperature, 40.3°C; average, 39.75°C). A single animal infected with Z-132 and all 3 animals infected with Soromba-R had no detectable fever during infection. Facial edema was apparent in half of the terminally ill animals. Similar to the results of the guinea pig study, infections with Josiah and Z-132 were 100% lethal in macaques, with mean times to death of 11.3 and 11.7 days, respectively, whereas infection with Soromba-R was lethal in 2 animals, with a prolonged time to death (average time to death, 15.5 days; Figure 2B).
Figure 2.
Disease progression of Lassa virus (LASV)–infected cynomolgus macaques. Groups of 3 macaques were infected with a median tissue culture infective dose of 1 × 104 LASV strain Josiah (green), Z-132 (red), or Soromba-R (blue) and scored daily for clinical signs of disease, as outlined in Materials and Methods. Animals infected with the Malian isolate (Soromba-R) demonstrated prolonged time to death (A) and decreased lethality (B), compared with animals infected with traditional LASV strains from Sierra Leone (Josiah) or Liberia (Z-132). Euthanasia occurred when animals reached a clinical score of 30 (see Materials and Methods). The bar with the dot above it indicates the clinical score for the macaque that did not progress to the point of euthanasia.
Serum Biochemical Findings
A summary of the serum biochemical findings can be found in Table 1. Liver indices showed an overall trend toward increase levels of transaminases (alanine aminotransferase [ALT] and aspartate aminotransferase [AST]) during infection. On average, AST values in all groups were higher than ALT values. ALT levels began to spike at day 10 after infection, peaked around day 13 after infection, and, only in the Soromba-R group, began to normalize. Levels of albumin and total protein had a downward trend across all infection groups. This is likely a result of redistribution into the extravascular space, secondary to capillary leak syndrome, as can occur in sepsis. These decreases could also be a component of decreased hepatic synthesis; however, the slow trend downward is suggestive of inflammation-mediated capillary leakage rather than poor hepatic synthesis, because liver failure tends to occur more abruptly. Alkaline phosphatase (ALP) levels increased up to the time of euthanasia in all but 1 case of Soromba-R infection, also suggesting liver injury in most animals. Usually, the ALP level is elevated in cholestatic, infiltrative, and inflammatory liver diseases, and any or all of these processes can be occurring with arenavirus infection. The γ-glutamyltransferase values also increased, which signifies that the process was likely cholestatic (ie, due to intra- or extrahepatic bile duct blockage). Blood urea nitrogen values were increased in several animals in the terminal stage of disease, which, in the face of more normal creatinine values, is suggestive of a prerenal insult (ie, compromised blood flow to kidney probably due to decreased circulating volume, decreased cardiac output, or renal artery disruption). The remaining biochemical markers were relatively unchanged or demonstrated no trend during infection.
Table 1.
Summary of Coagulation, Biochemical, and Hematologic Findings for Lassa Virus (LASV)–Infected Cynomolgus Macaques
| Parameter | LASV Group |
||
|---|---|---|---|
| Josiah | Z-132 | Soromba-R | |
| Coagulation | |||
| Prothrombin time | 1.3 | 1.2 | NC |
| aPT time | 1.5 | 2 | 1.3 |
| Thrombin time | 1.1 | 1.5 | 1.2 |
| Fibrinogen levela | 2 | 2 | 1.75 |
| Protein C levelb | −2 | −1.5 | −1.6 |
| Protein S level | −2.4 | −2.1 | −1.6 |
| d-dimer level | Pos | Pos | Pos |
| Biochemical | |||
| ALT level | 8 | 13 | 8 |
| AST level | 9 | 11 | 9 |
| ALP level | 1.1 | 1.5 | 2.4 |
| Albumin level | −1.6 | −2.1 | −2.5 |
| Amylase level | −18 | −1.2 | −1.4 |
| Creatinine level | NC | NC | NC |
| GGT level | 1.2 | 1.3 | 1.2 |
| Glucose level | NC | NC | NC |
| Total protein level | −1.2 | −1.2 | −1.2 |
| Total bilirubin level | NC | NC | NC |
| Blood urea nitrogen level | NC | 1.4 | 1.9 |
| Ca level | NC | NC | NC |
| Uric acid level | NC | NC | NC |
| Hematologic | |||
| White blood cell count | 1.3 | 1.7 | 8.4 |
| Neutrophil count | 1.8 | 2.5 | 3.2 |
| Lymphocyte countb | −5.8 | −1.8 | −3.3 |
| Monocyte countb | −4.4 | −10.3 | −8.7 |
| Eosinophil countb | −3.6 | −8.6 | −2.6 |
| Basophil count | 20 | 49 | 59 |
| Red blood cell count | −1.3 | −1.2 | −1.2 |
| Platelet count | −1.7 | −2.4 | −1.9 |
| Hematocrit | −1.3 | −1.4 | −1.2 |
| Hemoglobin level | −1.4 | −1.2 | NC |
| Reticulocyte count | NC | NC | NC |
| Cell volume | NC | NC | NC |
| Corpuscular volume | NC | NC | NC |
| Corpuscular hemoglobin volume | NC | NC | NC |
Unless otherwise indicated, data are average fold-changes in values measured at the time of death, compared with values measure at baseline (prechallenge).
Abbreviations: ALT, alanine aminotransferase; ALP, alkaline phosphatase; aPT, activated partial thromboplastin; AST, aspartate aminotransferase; GGT, γ-glutamyltransferase; NC, no change; Pos, positive.
a Fibrinogen concentrations demonstrated general increases until days 7–10 after infection, after which a precipitous drop was noted in most animals. Values shown represent peak fold-changes.
b Protein C activity and lymphocyte, monocyte, and eosinophil counts demonstrated a transient decrease between days 7 and 10 after infection. Values shown represent maximum fold-decreases observed during this period.
Hematological Findings
Hematological findings (Table 1) demonstrated a transient lymphopenia, neutropenia, monocytopenia, and eosinopenia, as well as anemia, in all infected animals 4–10 days after infection. The trends in hematocrit and hemoglobin level were nearly identical, which implies that the animals were losing whole blood from bleeding as opposed to hemoconcentrating. This was followed by generalized leukocytosis on days 10–13 after infection, which was mainly due to neutrophilia. There was a superimposed trend of lymphopenia beginning around days 4–10 after infection, but this had little effect on overall white blood cell counts, as neutrophilia predominated. Platelets showed an overall downward trend during infection, although the lowest counts were rarely below the threshold of thrombocytopenia (defined as a platelet count of <150 000 platelets/µL) in most animals. The timing of the drop coincided with the coagulation disorders noted below. The trend of the mean platelet volume increased during infection, which implies that the bone marrow was able to produce new (larger) platelets, thereby confirming consumptive platelet loss as opposed to decreased production.
Coagulation Parameters
Coagulation profiles (Table 1) showed general increases in prothrombin time, activated partial thromboplastin time, and thrombin time, beginning 7–10 days after infection. Corresponding to this, an increase and precipitous fall in fibrinogen levels was observed, with the decline occurring in parallel with an increased detection of fibrinogen degradation products (ie, d-dimers). There was also a trend toward decreased protein S activity and a pronounced, transient decrease in protein C activity 7–10 days after infection. Disseminated intravascular coagulation (DIC) is often stated not to be a part of LF in humans; however, combined, our results suggest DIC involvement in the macaque model of LF. In general, the changes in coagulation profiles were slightly delayed in the Soromba-R group. Interestingly, despite similar trends in coagulation parameters, hemorrhage was exclusively noted in the 3 animals infected with LASV strain Z-132 and presented as mild to moderate multifocal petechiation of the epididymis and mucosal linings of the bladder and colon, as well as dermal petechia.
Serum Cytokine and Chemokine Analysis
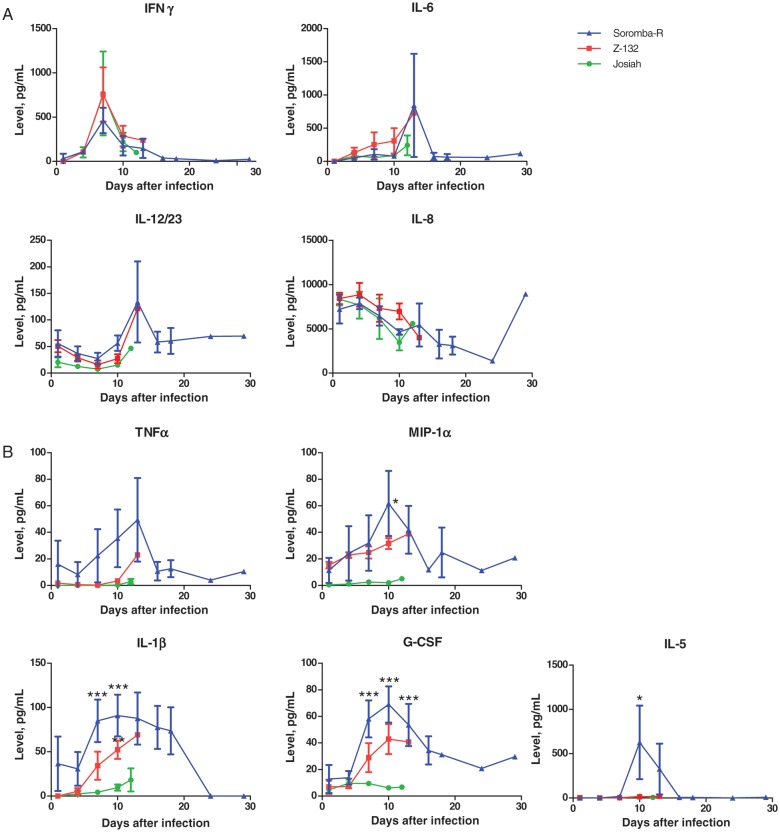
Analysis of serum cytokine/chemokine levels revealed interesting differences in immune activation between the 3 groups; however, several general trends were noted in our study that are consistent with previous work. A transient spike in IFN-γ levels 7–10 days after infection and moderate increases in IL-6 and IL-12/23 levels at the time of death were noted in all groups. These patterns have previously been associated with poor prognosis in humans [26] and NHPs [18, 27]. Similarly, a decrease in IL-8 levels, which has been suggested as an indicator of fatal infection in humans [26], was noted across all groups. Increases in IL-2, IL-18, and MCP-1 levels were also observed during the course of infection in all groups. Perhaps most interesting, infection with Soromba-R resulted in the most immune activation, specifically, neutrophil-activating or -potentiating proinflammatory cytokines or growth factors, including TNF-α, MIP 1α, IL-1β, and G-CSF, as well as IL-5 (Figure 3). This is in sharp contrast to the Josiah infection group, which, consistent with previous studies, demonstrated little to no activation of MIP-1α, IL-1β, or TNF-α [26, 28]. Importantly, increased IL-1β has previously been associated with nonfatal cases of LF and may play a role in the decreased lethality and increased time to death observed in Soromba-R–infected NHPs [26].
Figure 3.
Serum cytokine and chemokine responses in Lassa virus (LASV)–infected cynomolgus macaques. Serum cytokine/chemokine concentrations were determined in serial serum samples collected from macaques infected with LASV isolates Josiah (green), Z-132 (red), or Soromba-R (blue), using a nonhuman primate cytokine kit (Millipore) as described by the manufacturer. Several predictors of severe Lassa fever were confirmed in the 3 infection groups, including a transient spike in interferon γ (IFN-γ) level, moderate increases in interleukin 6 (IL-6) and interleukin 12/23 (IL-12/23) levels, and a decrease in interleukin 8 (IL-8) level (A). Interestingly, LASV strain Soromba-R and, to a lesser extent, strain Z-132 resulted in increased activation of several cytokines/chemokines, compared with LASV strain Josiah, including tumor necrosis factor α (TNF-α), macrophage inflammatory protein 1α (MIP-1α), interleukin 1β (IL-1β), granulocyte colony-stimulating factor (G-CSF), and interleukin 5 (IL-5; B). Data were analyzed with 2-way analysis of variance, using a Bonferroni posttest comparing Soromba-R and Z-132 infection groups to the Josiah group. Error bars represent the standard error of the mean. *P < .05, **P < .01, and ***P < .001.
Pathological and Histopathological Findings of LASV Infection
At necropsy, several gross pathological findings were common among the 3 LASV strains used in these studies. Mild to moderate hepatomegaly and splenomegaly were observed in all cynomolgus macaques at the time of death. All lymph nodes examined (inguinal, axillary, submandibular, mesenteric, and bronchial) were mildly to moderately enlarged and hyperplastic in all 3 groups. Radiography revealed an increased cardiothoracic size in the majority of animals, which could represent pericardial effusion, cardiomyopathy, or multichamber enlargement. However, to differentiate these would require a functional test (ie, echocardiography).
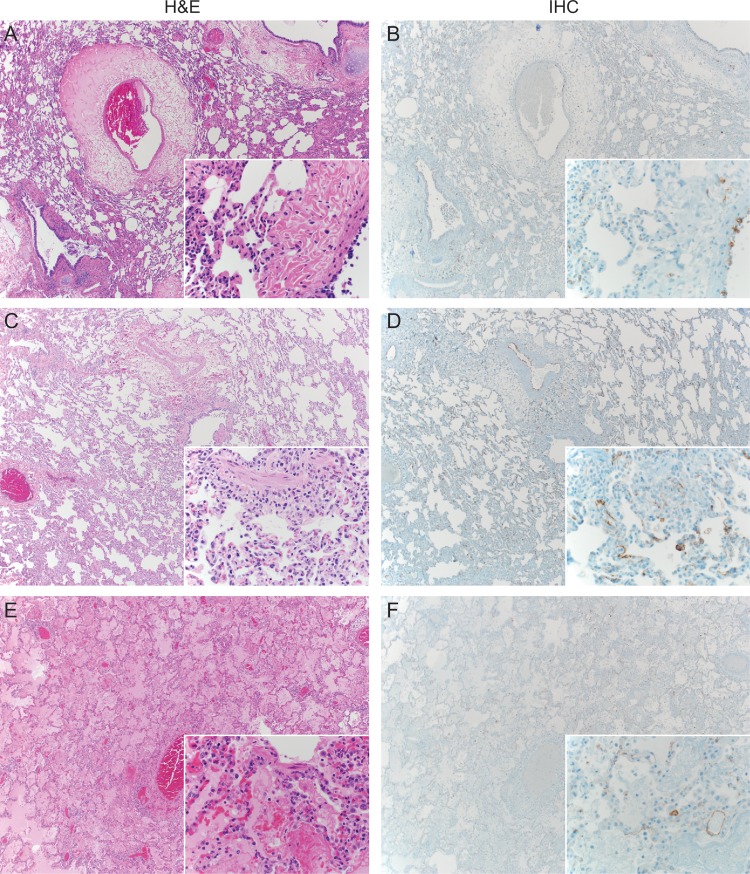
The most striking observation in these studies was the extent of lung pathology in the Soromba-R infection group (Figures 4 and 5). Radiographically, extensive pulmonary infiltrates were apparent in the 2 terminally ill NHPs infected with Soromba-R. At necropsy, pulmonary lesions were most pronounced in these animals. Specifically, the lungs were severely wet and heavy, with diffuse areas of reddening affecting 50%–100% of all lobes. In contrast, 1 of 3 animals infected with Z-132 and 2 of 3 animals infected with Josiah demonstrated multifocal areas of discoloration of varying degrees (on average affecting 25%–50% of individual lobes); however, only those from the single Z-132–infected animal were obviously edematous. Histologically, LASV infection resulted in mild to severe subacute interstitial pneumonia characterized by multifocal to coalescing thickening of alveolar septa by edema, fibrin deposition, and varying numbers of immune cells (plasma cells, lymphocytes, macrophages, and neutrophils) and multifocal type 2 pneumocyte hyperplasia. Consistent with the radiographic and gross pathological observations, LASV strain Soromba-R induced the most severe changes (average severity score, 4), with coalescing to diffuse interstitial pneumonia in every lung lobe (Figure 5). The pneumonia caused by LASV strains Josiah and Z-132 was considerably less diffuse, with decreased edema and fewer inflammatory cells (average severity score, 1.7 for both strains), which is in agreement with previous studies [18].
Figure 4.
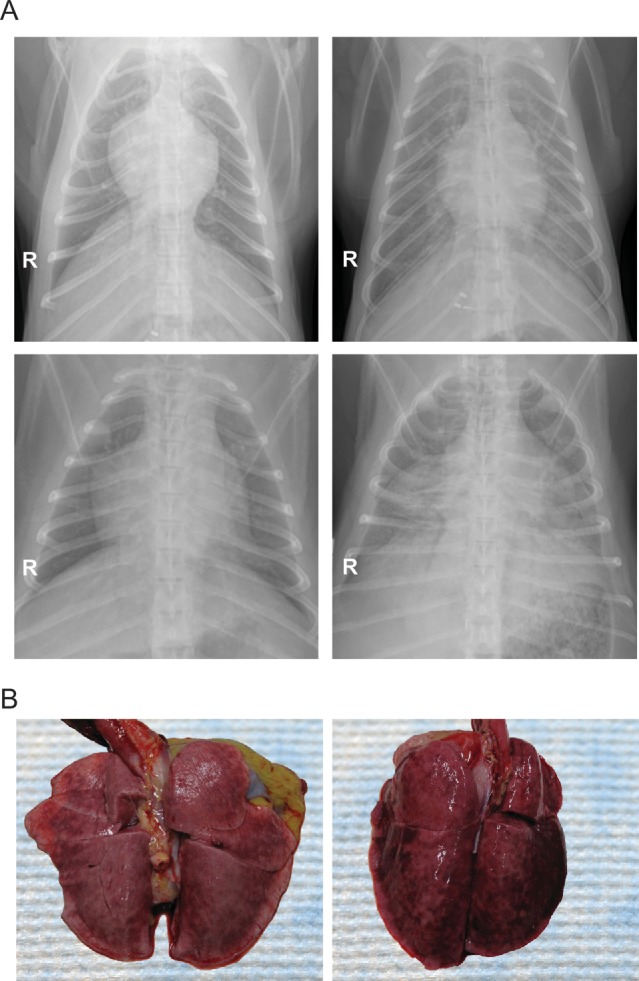
Radiological and gross pathological examination of the lungs of Lassa virus (LASV)–infected cynomolgus macaques. Macaques infected with the Malian LASV isolate (Soromba-R) demonstrated an atypical clinical presentation that consisted of increased pulmonary manifestations. A, Radiographs taken prior to infection on day 0 (baseline; left images) and at the time of death (right images) from a representative animal infected with LASV strains Josiah (top) and Soromba-R (bottom) are shown. Note the increased pulmonary infiltrates in the radiographs taken immediately prior to euthanasia in the Soromba-R–infected animal, which are suggestive of moderate to severe pneumonia. In contrast, radiographs taken at the time of euthanasia in animals infected with LASV Josiah revealed limited pulmonary infiltrates, primarily in the lower left quadrant in this image. B, Gross pathological examination revealed extensive areas of discoloration in the lungs from animals infected with Soromba-R (right), compared with those from animals infected with Josiah (left).
Figure 5.
Histological analysis of lungs from Lassa virus (LASV)–infected cynomolgus macaques. Infection with a median tissue culture infective dose of 1 × 104 LASV isolates Josiah (A and B), Z-132 (C and D), and Soromba-R (E and F) revealed a similar degree of viral antigen staining in the pulmonary endothelium across the 3 infection groups. Despite this, the severity of pathological changes was most prominent in the lungs of Soromba-R–infected macaques, with coalescing to diffuse interstitial pneumonia and pulmonary edema observed in every lung lobe. By comparison, the pneumonia caused by Josiah and Z-132 was considerably less diffuse, with decreased edema and fewer inflammatory cells. Images are at 40× magnification with a 400× inset. Abbreviations: H&E, hematoxylin-eosin stain; IHC, immunohistochemical analysis.
Histologically, the remaining organs analyzed showed no significant differences between the 3 infection groups and concurred with findings of other studies (Supplementary Figure 2) [18, 27]. Most animals demonstrated a mild, multifocal portal hepatitis with portal vessels bounded by small numbers of plasma cells, lymphocytes, and few macrophages and neutrophils. Several animals also had multifocal, random necrosis of hepatocytes, with loss of hepatocytes and replacement by karyorrhectic and cellular debris, along with small numbers of neutrophils, macrophages, and plasma cells. All 3 LASV strains induced meningoencephalitis in the frontal lobe, cerebellum, and brainstem, with lesions distinguished by small numbers of lymphocytes and plasma cells that multifocally expanded throughout Virchow-Robin spaces and by multifocal gliosis. Every animal had evidence of a normal immunologic response. All lymph nodes examined had follicular hyperplasia and thickening of medullary cords by abundant plasma cells. The spleen displayed similar changes, with minimal to mild follicular hyperplasia of the white pulp. Histological changes in the remaining tissues analyzed were largely unremarkable.
Results of IHC staining for LASV antigen did not vary significantly between the 3 groups. LASV antigen was detectable in endothelial cells in all tissues examined (lung, mediastinal lymph nodes, liver, spleen, kidney, and brain), as well as in hepatocytes, dendritic cells, and macrophages in spleen, bronchial epithelial cells, type II pneumocytes, lymph node follicular centers, and foci of gliosis.
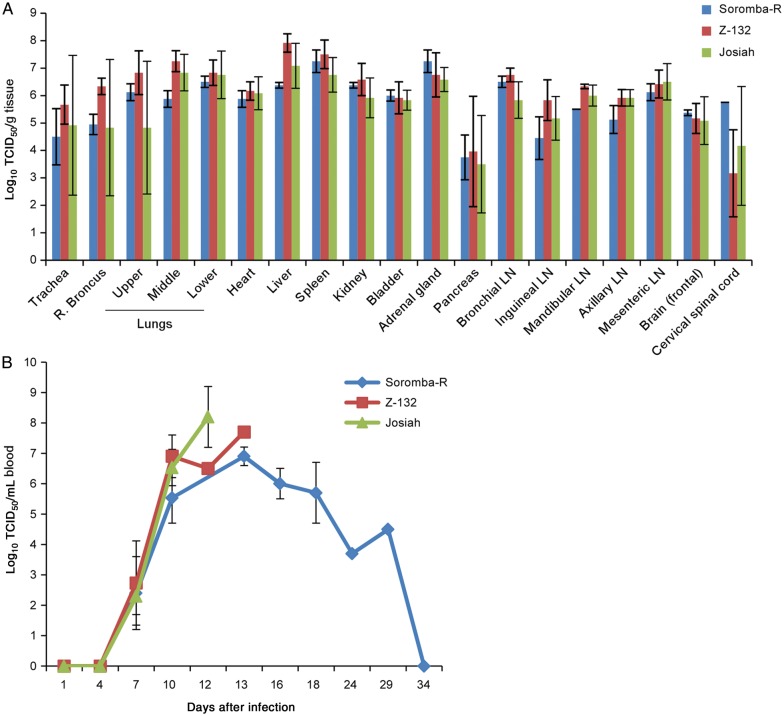
Viremia and Viral Load in Tissues
LASV produced a systemic infection in macaques, with all 3 isolates replicating to similarly high titers in all organs analyzed (Figure 6A). Viremia was detected in all animals by days 7–10 after infection, with high viral titers in blood maintained until euthanasia (Figure 6B). There was no significant difference in LASV titers from the blood of the surviving animal as compared to those with lethal infections. Viremia was detected for approximately 1 month after challenge in the survivor. These findings suggest the potential for increased risk of person-to-person transmission of LASV by individuals who recover from LF.
Figure 6.
Viremia and organ titers from Lassa virus (LASV)–infected cynomolgus macaques. Macaques infected with a median tissue culture infective dose (TCID50) of 1 × 104 LASV isolates Josiah (green; n = 3), Z-132 (red; n = 3), or Soromba-R (blue; n = 2) were euthanized as indicated by individual clinical scores, underwent necropsy, and had tissues titered by standard methods. A, LASV titers in solid organs did not differ across the 3 infection groups. B, LASV Josiah demonstrated slightly increased levels of viremia when compared to Z-132 or Soromba-R–infected nonhuman primates. The single survivor in the Soromba-R group did not have significantly lower levels of viremia (data not shown). Error bars represent the standard error of the mean. Shown are results for the right lung.
CONCLUSIONS
The apparently low incidence of clinically significant cases of LF in Mali (and other countries between Sierra Leone, Liberia, Guinea, and Nigeria) led us to speculate that the Malian LASV isolate may be less virulent. Recently, we found that the LASV prevalence among peridomestic Mastomys natalensis collected in southern Mali was 25%–50% [7, 28], suggesting that there is a high probability that people living in close contact with these animals are being exposed to LASV. However, even with the increased awareness of LF in Mali, only the imported case in early 2009 has been identified to date [6]. Differences in the virulence of Liberian LASV isolates have been previously demonstrated in inbred guinea pigs but not in a more stringent NHP model [20]. Here, we provide evidence in both animal models of LF that Soromba-R is less pathogenic, with decreased lethality and increased time to death in macaques, compared with LASV isolates from Sierra Leone and Liberia. In support of these findings, LASV AV, which was also isolated from outside the historical region of LASV endemicity [5] and is phylogenetically most closely related to Soromba-R [6, 7], was recently shown to be less pathogenic in cynomolgus macaques [27].
Soromba-R–infected NHPs demonstrated increased immune activation, which was possibly responsible for decreased virulence and increased pulmonary manifestations. An important virulence factor for LASV is the ability to evade the host's immune responses, with several studies demonstrating that LASV is extremely effective at dampening innate responses [18, 26, 29–33]. Consistent with published reports, LASV Josiah resulted in little to no activation of host responses in macaques. In contrast, LASV Z-132 infection and, most notably, Soromba-R infection resulted in increased innate responses, compared with the Josiah infection group. Importantly, TNF-α levels were considerably increased in NHPs infected with Soromba-R, which may partially explain the increased pulmonary manifestations noted in these animals, since TNF-α is known to increase the permeability of endothelial cells [34]. A key finding in this study was the atypical presentation of LF associated with Soromba-R infection. While the hallmarks of LF were present in these animals, we also found that NHPs infected with Soromba-R presented with increased pulmonary manifestations. On the basis of these observations, it seems possible that LF patients seeking medical attention in Mali may receive a misdiagnosis of pulmonary syndrome. Although the degree of respiratory involvement in the Josiah and Z-132 infection groups was low in our study, it is also possible that pulmonary manifestations associated with LASV infection in general are underrecognized throughout West Africa.
Genetically, LASV isolates have a large degree of diversity, which may result in differences in pathogenicity and disease manifestations [20, 35]. Combined, the findings of differences in clinical manifestations and immune suppression/activation observed here support this hypothesis and demonstrate the importance of studying geographically distinct LASV isolates in animal models of disease to gain a better understanding of LASV pathogenesis and to evaluate potential medical countermeasures against LF. Despite the high incidence of LF in Sierra Leone, Liberia, Guinea, and Nigeria, as well as the increasing frequency of imported cases of LF worldwide, currently there are no antivirals or vaccines licensed for treating or preventing LASV infection or LF [4, 36]. Ribavirin has been proven effective and is frequently used in an off-label manner to treat LF, although its efficacy is reliant on early administration [4, 13, 37, 38]. To date, the few therapeutic modalities tested in animal models have mainly been evaluated against the commonly used LASV Josiah [13, 17, 39–41]. The results of our study provide an important point of reference for evaluating therapeutic agents against these other strains of LASV.
Supplementary Data
Supplementary materials are available at The Journal of Infectious Diseases online (http://jid.oxfordjournals.org/). Supplementary materials consist of data provided by the author that are published to benefit the reader. The posted materials are not copyedited. The contents of all supplementary data are the sole responsibility of the authors. Questions or messages regarding errors should be addressed to the author.
Notes
Acknowledgments. We thank the Rocky Mountain Veterinary Branch (Division of Intramural Research [DIR], National Institute of Allergy and Infectious Diseases [NIAID], National Institutes of Health [NIH]), for assistance in animal care and basic animal procedures; Tina Thomas, Dan Long, and Rebecca Rosenke (DIR, NIAID, NIH), for preparing the pathology slides; Anita Mora and Heather Murphy (DIR, NIAID, NIH), for assistance with graphical work; Luis Branco and Robert Garry (Tulane University Health Science Center), for providing enzyme-linked immunosorbent assay reagents; and Lisa Hensley (US Army Medical Research Institute of infectious Diseases), for providing the primary antibody used in IHC analysis.
Financial support. This work was supported by the Division of Intramural Research, National Institute of Allergy and Infectious Diseases, National Institutes of Health.
Potential conflicts of interest. All authors: No reported conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.McCormick JB, King IJ, Webb PA, et al. A case-control study of the clinical diagnosis and course of Lassa fever. J Infect Dis. 1987;155:445–55. doi: 10.1093/infdis/155.3.445. [DOI] [PubMed] [Google Scholar]
- 2.Frame JD. Clinical features of Lassa fever in Liberia. Rev Infect Dis. 1989;11(Suppl 4):S783–9. doi: 10.1093/clinids/11.supplement_4.s783. [DOI] [PubMed] [Google Scholar]
- 3.Bausch DG, Demby AH, Coulibaly M, et al. Lassa fever in Guinea: I. Epidemiology of human disease and clinical observations. Vector Borne Zoonotic Dis. 2001;1:269–81. doi: 10.1089/15303660160025903. [DOI] [PubMed] [Google Scholar]
- 4.Ogbu O, Ajuluchukwu E, Uneke CJ. Lassa fever in West African subregion: an overview. J Vect Borne Dis. 2007;44:1–11. [PubMed] [Google Scholar]
- 5.Gunther S, Emmerich P, Laue T, et al. Imported Lassa fever in Germany: molecular characterization of a new Lassa virus strain. Emerg Infect Dis. 2000;6:466–76. doi: 10.3201/eid0605.000504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Atkin S, Anaraki S, Gothard P, et al. The first case of Lassa fever imported from Mali to the United Kingdom, February 2009. Euro Surveil. 2009;14 pii:19145. [PubMed] [Google Scholar]
- 7.Safronetz D, Lopez J, Sogoba N, et al. Detection of Lassa virus, Mali. Emerg Infect Dis. 2010;16:1123–6. doi: 10.3201/eid1607.100146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McCormick JB, Webb PA, Krebs JW, Johnson KM, Smith ES. A prospective study of the epidemiology and ecology of Lassa fever. J Infect Dis. 1987;155:437–44. doi: 10.1093/infdis/155.3.437. [DOI] [PubMed] [Google Scholar]
- 9.Fisher-Hoch SP, Tomori O, Nasidi A, et al. Review of cases of nosocomial Lassa fever in Nigeria: the high price of poor medical practices. Br Med J. 1995;311:857–9. doi: 10.1136/bmj.311.7009.857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gunther S, Lenz O. Lassa virus. Crit Rev Clin Lab Sci. 2004;41:339–90. doi: 10.1080/10408360490497456. [DOI] [PubMed] [Google Scholar]
- 11.Gowen BB, Holbrook MR. Animal models of highly pathogenic RNA viral infections: Hemorrhagic fever viruses. Antiviral Res. 2007;78:79–90. doi: 10.1016/j.antiviral.2007.10.002. [DOI] [PubMed] [Google Scholar]
- 12.Walker DH, Wulff H, Lange JV, Murphy FA. Comparative pathology of Lassa virus infection in monkeys, guinea pigs, and Mastomys natalensis. Bull World Health Organ. 1975;52:523–34. [PMC free article] [PubMed] [Google Scholar]
- 13.Jahrling PB, Hesse RA, Eddy GA, Johnson KM, Callis RT, Stephen EL. Lassa virus infection of rhesus monkeys: pathogenesis and treatment with ribavirin. J Infect Dis. 1980;141:580–9. doi: 10.1093/infdis/141.5.580. [DOI] [PubMed] [Google Scholar]
- 14.Callis RT, Jahrling PB, DePaoli A. Pathology of Lassa virus infection in the rhesus monkey. Am J Trop Med Hyg. 1982;31:1038–45. doi: 10.4269/ajtmh.1982.31.1038. [DOI] [PubMed] [Google Scholar]
- 15.Lange JV, Mitchell SW, McCormick JB, Walker DH, Evatt BL, Ramsey RR. Kinetic study of platelets and fibrinogen in Lassa virus-infected monkeys and early pathologic events in Mopeia virus infected monkeys. Am J Trop Med Hyg. 1985;34:999–1007. doi: 10.4269/ajtmh.1985.34.999. [DOI] [PubMed] [Google Scholar]
- 16.Fisher-Hoch SP, Mitchell SW, Sasso DR, Lange JV, Ramsey R, McCormick JB. Physiological and immunologic disturbances associated with shock in a primate model of Lassa fever. J Infect Dis. 1987;155:465–74. doi: 10.1093/infdis/155.3.465. [DOI] [PubMed] [Google Scholar]
- 17.Geisbert TW, Jones S, Fritz E, et al. Development of a new vaccine for the prevention of Lassa fever. PLoS Med. 2005;6:e183. doi: 10.1371/journal.pmed.0020183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hensley LE, Smith MA, Geisbert JB, et al. Pathogenesis of Lassa fever in cynomolgus macaques. Virol J. 2011;8:205. doi: 10.1186/1743-422X-8-205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wulff H, Johnson KM. Immunoglobulin M and G responses measured by immunofluorescence in patients with Lassa and Marburg virus infections. Bull WHO. 1979;57:631–5. [PMC free article] [PubMed] [Google Scholar]
- 20.Jahrling PB, Frame JD, Smith SB, Monson MH. Endemic Lassa fever in Liberia. III. Characterization of Lassa virus isolates. Trans R Soc Trop Med Hyg. 1985;79:374–9. doi: 10.1016/0035-9203(85)90386-4. [DOI] [PubMed] [Google Scholar]
- 21.Brining D, Mattoon J, Kercher L, et al. Thoracic radiography as a refinement methodology for the study of H1N1 influenza in the cynomolgus macaque (Macaca fascicularis) model. Comp Med. 2010;60:389–95. [PMC free article] [PubMed] [Google Scholar]
- 22.Ebihara H, Rockx B, Marzi A, et al. Host response dynamics following lethal infection of rhesus macaques with Zaire ebolavirus. J Infect Dis. 2011;204:S991–9. doi: 10.1093/infdis/jir336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Falzarano D, Feldmann F, Grolla A, et al. Single immunization with a monovalent vesicular stomatitis virus-based vaccine protects nonhuman primates against heterologous challenge with Bundibugyo ebolavirus. J Infect Dis. 2011;204:S1082–9. doi: 10.1093/infdis/jir350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vieth S, Drosten C, Lenz O, et al. RT-PCR for detection of Lassa virus and related Old World arenaviruses targeting the L gene. Trans R Soc Trop Med Hyg. 2007;101:1253–64. doi: 10.1016/j.trstmh.2005.03.018. [DOI] [PubMed] [Google Scholar]
- 25.Branco LM, Matschiner A, Fair JN, et al. Bacterial-based systems for expression and purification of recombinant Lassa virus proteins of immunological relevance. Virol J. 2008;5:74. doi: 10.1186/1743-422X-5-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mahanty S, Bausch DG, Thomas RL, et al. Low levels of interleukin-8 and interferon-inducible protein-10 in serum are associated with fatal infections in acute Lassa fever. J Infect Dis. 2001;183:1713–21. doi: 10.1086/320722. [DOI] [PubMed] [Google Scholar]
- 27.Baize S, Marianneau P, Loth P, et al. Early and strong immune responses are associated with control of viral replication and recovery in Lassa virus-infected cynomolgus monkeys. J Virol. 2009;83:5890–903. doi: 10.1128/JVI.01948-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sogoba N, Feldmann H, Safronetz D. Lassa fever in West Africa: evidence for an expanded region of endemicity. Zoonoses Public Health. 2012;59(Suppl 2):43–7. doi: 10.1111/j.1863-2378.2012.01469.x. [DOI] [PubMed] [Google Scholar]
- 29.Mahanty S, Hutchinson K, Agarwal S, McRae M, Rollin PE, Pulendran B. Cutting edge: impairment of dendritic cells and adaptive immunity by Ebola and Lassa viruses. J Immunol. 2003;170:2797–801. doi: 10.4049/jimmunol.170.6.2797. [DOI] [PubMed] [Google Scholar]
- 30.Baize S, Kaplon J, Faure C, Pannetier D, Georges-Courbot MC, Deubel V. Lassa virus infection of human dendritic cells and macrophages in productive but fails to activate cells. J Immunol. 2004;172:2861–9. doi: 10.4049/jimmunol.172.5.2861. [DOI] [PubMed] [Google Scholar]
- 31.Lukashevich IS, Maryankova R, Vladyko AS, et al. Lassa and Mopeia virus replication in human monocytes/macrophages and in endothelial cells: different effects on IL-8 and TNF-α gene expression. J Med Virol. 1999;59:552–60. [PMC free article] [PubMed] [Google Scholar]
- 32.Qi X, Lan S, Wang W, et al. Cap binding and immune evasion revealed by Lassa nucleoprotein structure. Nature. 2010;468:779–83. doi: 10.1038/nature09605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hastie KM, Kimberlin CR, Zandonatti MA, MacRae IJ, Ollmann Saphire E. Structure of the Lassa virus nucelprotein reveals a dsRNA-specific 3′ to 5′ exonuclease activity essential for immune suppression. Proc Natl Acad Sci U S A. 2011;108:2396–401. doi: 10.1073/pnas.1016404108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Feldmann H, Bugani H, Mahner F, Klenk HD, Drenckhahn Schnittler HJ. Filovirus-induced endothelial leakage triggered by infected monocytes/macrophages. J Virol. 1996;70:2208–14. doi: 10.1128/jvi.70.4.2208-2214.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bowen MD, Rollin PE, Ksiazek TG, et al. Genetic diversity among Lassa virus strains. J Virol. 2000;74:6992–7004. doi: 10.1128/jvi.74.15.6992-7004.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Macher AM, Wolfe MS. Historical Lassa fever reports and 30-year clinical update. Emerg Infect Dis. 2006;12:835–7. doi: 10.3201/eid1205.050052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McCormick JB, King IJ, Webb PA, et al. Lassa fever. Effective therapy with ribavirin. N Engl J Med. 1986;314:20–6. doi: 10.1056/NEJM198601023140104. [DOI] [PubMed] [Google Scholar]
- 38.Bausch DG, Hadi CM, Khan SH, Lertora JJ. Review of the literature and proposed guidelines for the use of oral ribavirin postexposure prophylaxis for Lassa fever. Clin Infect Dis. 2010;51:1435–41. doi: 10.1086/657315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lukashevich IS, Patterson J, Carrion R, et al. A live attenuated vaccine for Lassa fever made by reassortment of Lassa and Mopeia viruses. J Virol. 2005;79:13934–42. doi: 10.1128/JVI.79.22.13934-13942.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cashman KA, Smith MA, Twenhafel NA, et al. Evaluation of Lassa antiviral compound ST-193 in a guinea pig model. Antiviral Res. 2011;90:70–9. doi: 10.1016/j.antiviral.2011.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jiang X, Dalebout TJ, Bredenbeek PJ, et al. Yellow fever 17D-vectored vaccines expressing Lassa virus GP1 and GP2 glycoproteins provide protection against fatal disease in guinea pigs. Vaccine. 2011;29:1248–57. doi: 10.1016/j.vaccine.2010.11.079. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.