Abstract
Abdominal paracentesis is a frequently employed diagnostic and therapeutic procedure for patients with refractory ascites, typically in patients with cirrhosis. It is generally regarded as a safe procedure with significant complications occurring in <1% of cases. Most hemorrhagic complications are due to abdominal wall trauma, during which clear evidence of active bleeding is usually visualized during the procedure. Delayed hemoperitoneum is a rare complication of large-volume paracentesis in which clinical evidence of active bleeding is typically absent until substantial blood loss has taken place (often several days to a week later), leading to an exceedingly high mortality rate. Herein we describe a case of delayed hemoperitoneum in a 55-year-old man with heart failure. This case emphasizes the importance of identifying patients who are at high risk for delayed hemoperitoneum as well as the need to closely monitor complete blood counts in the days following a large-volume paracentesis.
CASE DESCRIPTION
A 55-year-old man presented with a 2-week history of worsening dyspnea and abdominal distention. He had atrial fibrillation, chronic heart failure (last known ejection fraction 25%), and chronic kidney disease. He reported nonadherence to his furosemide for 3 weeks. He had a massively tense and protruding abdominal wall and 3/4+ pitting lower extremity edema to his knees bilaterally. His international normalized ratio was 2.3 (on warfarin), serum creatinine 2.33 mg/dL (baseline: 2.0–3.0 mg/dL), and albumin 2.3 g/dL. Abdominal ultrasound revealed hepatomegaly without cirrhosis. Two doses of 80 mg intravenous furosemide led to minimal reduction of his abdominal ascites. A paracentesis under ultrasound guidance was performed in the left lower quadrant and yielded 5 L of clear, transudative fluid. No evidence of hematoma was noted, and the procedure provided immediate symptomatic relief.
Three days later the patient began complaining of mild, diffuse abdominal discomfort. Over the previous 3 days his hemoglobin level had dropped from 8.4 to 6.9 g/dL. No evidence of gastrointestinal or genitourinary blood loss was noted. The patient, a Jehovah's Witness, refused transfusion of any blood products and in the next 2 days his hemoglobin declined to 2.9 g/dL. A repeat diagnostic paracentesis was performed and showed 10 mL of blood-tinged fluid. The following day a tagged red blood cell scan indicated evidence of increased activity near the duodenum and gastric antrum (Figure 1). An urgent upper endoscopy demonstrated no evidence of active upper gastrointestinal bleeding but did demonstrate a bluish hue on the posterior stomach wall, suggestive of a possible intraperitoneal or retroperitoneal bleed. Subsequent noncontrast computed tomography (CT) of the abdomen and pelvis showed likely hemoperitoneum localized to the mid-lower abdominal wall (Figure 2). An urgent epigastric and gastroduodenal angiogram did not reveal any evidence of active bleeding.
Figure 1.
Red blood cell scan tagged with Technetium-99m to evaluate for active gastrointestinal bleed shows increased activity in the region of the duodenum and the gastric antrum.
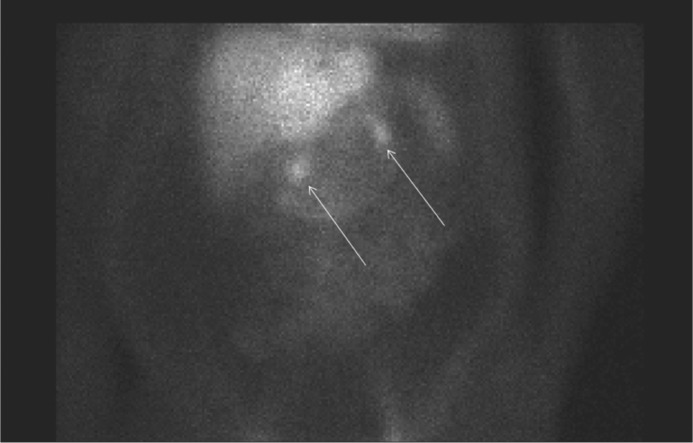
Figure 2.

CT of the abdomen and pelvis without contrast reveals hemoperitoneum (arrows) localized to the lower left and middle quadrant.
The patient continued to refuse blood transfusion and was treated supportively with intravenous fluid and albumin infusions. Slight improvements in serum creatinine (3.6 mg/dL) and hemoglobin (4.1 g/dL) were noted. The patient refused any further intervention and was discharged to home hospice; he died 3 days later, 11 days after the initial paracentesis.
DISCUSSION
Large-volume paracentesis (>4 L) is a common bedside procedure utilized in patients with refractory abdominal ascites with poor response to diuretic therapy. The procedure is typically regarded as safe and carries a hemorrhagic complication rate of <1% (1, 2) (further reduced with ultrasound guidance and a left lower quadrant approach [3, 4]). When hemorrhagic complications occur, they are typically due to abdominal wall vessel puncture, with visible bleeding during the procedure (2). Consequently, many patients are discharged soon after the procedure and without close follow-up.
Delayed hemoperitoneum is a rare hemorrhagic complication of large-volume paracentesis. The proposed mechanism is the large volume fluid removal, which results in a rapid drop in intraperitoneal pressure. This promotes a transient pressure gradient in the splanchnic circulation, promoting dilation and rupture of friable mesenteric varices (1, 5, 6). Due to slow venous bleeding rates, patients are often initially asymptomatic. The most commonly reported symptom is vague abdominal pain (1), which may be overlooked in patients with chronic ascites. Peritoneal signs typically do not occur until late stages (if at all), and any clinical signs of bleed may be absent until substantial blood loss has taken place as long as several days to a week later (1, 5). Consequently, patients have been known to present in hemorrhagic shock, and mortality rates are reported to exceed 70% (5).
Given the rare occurrence of delayed hemoperitoneum, clinicians must be made aware of high-risk patient groups. Previously established risk factors include advanced cirrhosis with refractory ascites, history of previous large-volume paracentesis, and the appearance of retrograde mesenteric venous flow on ultrasound (due to the occurrence of large mesenteric collaterals, which are predisposed to rupture) (5). Additionally, an association between postparacentesis hemorrhagic complications and chronic kidney disease has also been noted (likely due to platelet dysfunction) (6). Surprisingly, no associations between coagulopathy and hemorrhagic complications of paracentesis have been shown, so there are currently no guidelines for either preprocedural coagulation parameters that contraindicate paracentesis or the prophylactic administration of fresh frozen plasma or platelets (3, 5).
Previously described cases of delayed hemoperitoneum have not demonstrated evidence of intraprocedural abdominal wall trauma or other complications; thus, it is critical to recognize potential warning signs (1, 6). Complete blood counts should be closely monitored for a minimum of several days in high-risk groups, and once a notable drop in hemoglobin is detected, a diagnostic paracentesis should be performed to assess the presence of visible blood (5). If blood is detected on diagnostic paracentesis, an abdominal CT scan or ultrasound should be performed to evaluate for abdominal wall hematoma. In the absence of apparent hematoma formation, angiography should be strongly considered (5, 6).
Initial management should focus on identification of a bleeding source with interim supportive management. Coagulopathies should be corrected, and patients should be fluid resuscitated with normal saline and packed red blood cells as needed (6). In the event of patient blood transfusion refusal (as in our case), albumin or artificial colloid solution should be given. Previously described successful interventions include portocaval shunting and embolization or surgical ligation of bleeding vessels (2, 5). Unfortunately, angiographic visualization of bleeding vessels is often difficult, and in the setting of hemodynamic instability, laparotomy may be needed for adequate visualization of the bleeding site (5).
The most important preventative measure in delayed hemoperitoneum is daily monitoring of complete blood counts for a minimum of several days to ensure rapid detection and minimize blood loss (1, 5). Patients with underlying renal dysfunction may benefit from prophylactic transfusion of fresh frozen plasma or desmopressin acetate—a target of future studies (6). Finally, patients with risk factors for hemoperitoneum may benefit from either a lower-volume paracentesis, slower drainage of ascites, or concurrent administration of albumin to guard against rapid changes in the intraperitoneal pressure gradient (1).
References
- 1.Webster ST, Brown KL, Lucey MR, Nostrant TT. Hemorrhagic complications of large volume abdominal paracentesis. Am J Gastroenterol. 1996;91(2):366–368. [PubMed] [Google Scholar]
- 2.Martinet O, Reis ED, Mosimann F. Delayed hemoperitoneum following large-volume paracentesis in a patient with cirrhosis and ascites. Dig Dis Sci. 2000;45(2):357–358. doi: 10.1023/a:1005424929241. [DOI] [PubMed] [Google Scholar]
- 3.Runyon BA. AASLD Practice Guidelines Committee. Management of adult patients with ascites due to cirrhosis: an update. Hepatology. 2009;49(6):2087–2107. doi: 10.1002/hep.22853. [DOI] [PubMed] [Google Scholar]
- 4.Grabau CM, Crago SF, Hoff LK, Simon JA, Melton CA, Ott BJ, Kamath PS. Performance standards for therapeutic abdominal paracentesis. Hepatology. 2004;40(2):484–488. doi: 10.1002/hep.20317. [DOI] [PubMed] [Google Scholar]
- 5.Arnold C, Haag K, Blum HE, Rössle M. Acute hemoperitoneum after large-volume paracentesis. Gastroenterology. 1997;113(3):978–982. doi: 10.1016/s0016-5085(97)70210-5. [DOI] [PubMed] [Google Scholar]
- 6.Pache I, Bilodeau M. Severe haemorrhage following abdominal paracentesis for ascites in patients with liver disease. Aliment Pharmacol Ther. 2005;21(5):525–529. doi: 10.1111/j.1365-2036.2005.02387.x. [DOI] [PubMed] [Google Scholar]


