Abstract
Dural venous sinus thrombosis, especially of the sigmoid sinus, is a known but uncommon intracranial extradural complication of chronic suppurative otitis media. Even rarer is the simultaneous occurrence of bilateral abducens palsy in the same patient. We report the case of an adolescent male who presented with signs of raised intracranial pressure, diplopia and bilateral lateral rectus palsy associated with a history of left ear discharge and neck swelling. Extensive dural sinus thrombosis extending right up to the left internal jugular vein was confirmed on CT imaging. The patient was successfully treated with thrombolytic agents and antibiotic therapy. The pathophysiology of the concurrent complications is discussed.
Background
Otitis media, be it acute or chronic, is a condition commonly treated in the otorhinolaryngology set-up. Complications arising from otitis media seem to be on the down-going trend, thanks to the advent and usage of effective antibiotics. However, when complications do occur, especially intracranially, they tend to carry along with them a high rate of morbidity and mortality. The death rate of lateral and sigmoid sinus thrombosis, for instance, has been reported to be in the range of 5–35%.1 However, the occurrence of bilateral abducens palsy is very rare as compared to its occurrence unilaterally. This case illustrates the concurrent occurrence of dual complications of otitis media in a single patient.
Case presentation
An 18-year-old Asian gentleman presented with a history of left ear discharge of 6 weeks’ duration, which was initially painful and had never been treated, and a left neck swelling of 1 month. There was no history of fever. Subsequently, he complained of double vision and bilateral blurring of vision of 1-month duration, which was associated with the acute onset of headache and vomiting for 1 week. The patient tends to frequently swim in the river as well as dig his ears often. Nasal or throat symptoms were unremarkable.
Clinically, the patient appeared to be healthy, not lethargic or toxic looking. He had bilateral lateral rectus palsy and bilateral papilloedema. Cerebellar signs and ptosis were absent. Rigid nasal endoscopy revealed a moderately hypertrophied adenoid tissue with bilateral fossa of Rosenmüller unaffected and normal looking. Flexible endoscopy of the larynx was unremarkable. Otoscopy confirmed the presence of a 20% perforation of the left pars tensa with yellowish, thick, foul-smelling mucopurulent discharge noted from within (figure 1). Pus culture grew a mixture of Staphylococcus aureus and a Gram-negative bacillus. The right ear was normal. A vague, diffuse, firm swelling over the left level II and III regions, which was non-tender, was present. Total white count stood at 10.5 and the erythrocyte sedimentation rate (ESR) was elevated at 81.
Figure 1.

Otoscopy of the left ear revealing perforation of the tympanic membrane.
Investigations
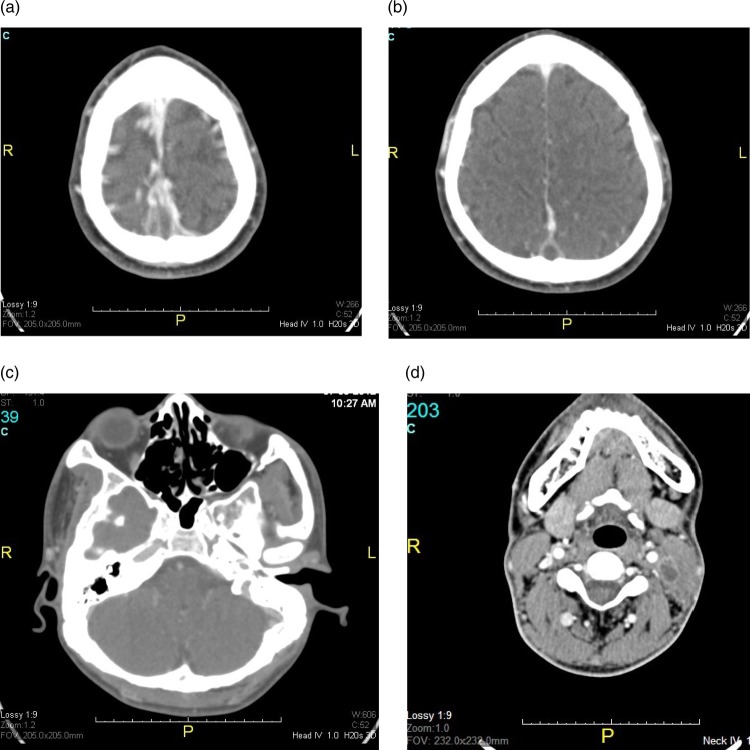
CT imaging revealed an extensive filling defect within the posterior part of the superior sagittal sinus (figure 2A), giving rise to the empty delta sign (figure 2B). The thrombosis extended into the left transverse sinus, left sigmoid sinus (figure 2C) and all the way down into a dilated left internal jugular vein (figure 2D). Numerous suspicious filling defects noted within the cavernous sinus were likely to represent cavernous sinus thrombosis, although the sinuses showed normal concave configuration bilaterally. Bilateral mastoid sclerosis was also noted. The ossicular bones, however, remained unaffected. Soft tissue, possibly granulation tissue, was noted within the middle ear cavity.
Figure 2.
(A) Thrombosis within the posterior part of the superior sagittal sinus;(B) empty delta sign on a CT scan;(C) thrombosis within the left sigmoid sinus and (D) dilated left internal jugular vein.
Differential diagnosis
Gradenigo's syndrome
Lemierre's syndrome
Nasopharyngeal carcinoma.
Treatment
The diagnosis of chronic suppurative otitis media complicated with bilateral lateral rectus palsy and extensive dural sinus thrombosis was established. Immediately, thrombolytic agent and antibiotic therapy was started, and the patient was jointly managed together with the ophthalmology, neurosurgical and neuromedical services. A bolus dose of intravenous heparin at 5000 ü and subsequent infusion at 1000 ü per hour was given and regular daily ear toileting was performed. The affected ear was instilled with ofloxacin ear drops and intravenous ceftriaxone at 2 g daily was administered.
Outcome and follow-up
The patient made a near-complete recovery within 72 h of the start of treatment. His raised intracranial pressure symptoms subsided and the bilateral lateral rectus palsy had resolved. The neck swelling was still present but was slowly subsiding. The ear had dried off and the perforation had sealed off. A myringotomy was performed and a grommet was inserted to ventilate the middle ear cavity. The patient was subsequently switched to subcutaneous enoxaparin 60 mg twice daily, which was given for 3 months. Upon completion of 2 weeks of intravenous antibiotics, 4 weeks of oral antibiotics and 3 months of anticoagulant therapy, the ESR had dropped to 28 and the only residual symptom still present was blurred vision, which had mildly improved.
Discussion
Chronic suppurative otitis media can give rise to intracranial or extracranial complications. The extracranial type can be intratemporal or extratemporal with facial nerve palsy, labyrinthitis, petrositis, subperiosteal abscess and internal carotid artery aneurysm being the intratemporal complications and Luc's abscess, Bezold's abscess, Citelli's abscess and subclavian vein thrombosis being the extratemporal complications. The intracranial complications, on the other hand, can be intradural, being subdural abscess, cerebral abscess and otic hydrocephalus or extradural, being extradural abscess, meningitis and sigmoid sinus thrombosis.
Thrombosis, which is clotting or coagulation of blood in the circulatory system, could occur in any vein or artery in any part of the body. Thrombosis tends to form when there is disruption of vessel wall integrity, hypercoagulability of the blood and stasis, three factors which make up the Virchow's triad. They could be septic in origin, which is due to an infection causing thrombophlebitis, or aseptic due to prothrombotic conditions, trauma or iatrogenic causes. Middle ear and mastoid infections cause venous sinus thrombosis by either direct spread or via the emissary veins.2 When the infection is persistent, it leads to the formation of a septic thrombus. Typically the vein is dilated with a blood clot. The smaller tributary veins tend to rupture, blood extravasates and this is followed by the loss of function of the affected organ.2 The extent of damage not only depends on the site and size of the vessel affected, but also on the sudden, rapid manner in which they extend.
The intracranial pressure at rest is normally 7–15 mm Hg for a supine adult. When it is elevated, patients present with headache, vomiting, ocular palsies, altered level of consciousness and papilloedema. At the severe end of the spectrum develops the Cushing triad. The possible logical explanation for the raised intracranial pressure due to the thrombosis in this case could be due to the presence of obstruction to the venous outflow, resulting in venous engorgement. Impaired cerebrospinal fluid reabsorption could also be a contributing factor to the elevated intracranial pressure.
Unilateral lateral rectus palsy is commonly associated with middle ear infections. This is due to the fact that when the abducens nerve passes adjacent to the mastoid region on the affected side, the infection and inflammation within the mastoid cavity could result in inflammation of the meninges and subsequent abducens palsy. Hence, one would be able to imagine that for a bilateral abducens palsy to occur due to an isolated middle ear infection, both sides of the ears and nerves would have to be affected, which is extremely rare. Diabetes mellitus, Symonds’ syndrome, Wildervanck's syndrome and trauma among others have been reported in the literature to cause bilateral lateral rectus palsy.3 Lang et al4 in 2002 had reported two cases of resolved otitis media which presented with mono and bilateral abducens paralysis, respectively, as the initial symptom of sinus vein thrombosis. Isolated unilateral otitis media causing bilateral abducens palsy has not been reported in the literature so far. The pathophysiology of such a situation can be attributed to a few mechanisms. Slow recovery of the abducens nerve palsy, without the involvement of other cranial nerves, would indicate that the palsy is posterior to the superior orbital fissure, which is either posterior where the abducens nerve passes beneath the petroclinoid ligament near the inferior petrosal sinus or in the cavernous sinus.5 Compression of the nerve against the petroclinoid ligament or interruption of the fragile arterial blood supply would cause an abducens nerve palsy.5 Transient diplopia and lateral rectus palsy could be explained by the fact that a posterior fistula may drain into the inferior petrosal sinus. This causes distension of the sinus and intermittent compression of the abducens nerve.6 A posterior fistula is a dural fistula related to the dorsomeningeal branches that can interfere with the blood supply of the abducens nerve.
Bilateral abducens palsy could also be attributed to the possibility of the raised intracranial pressure causing displacement of the brain tissue, oedema and pressure on both the abducens nerves. The abducens nerve tends to especially have a predilection to be the first and commonly affected nerve, as it not only emerges nearest to the base of the skull and has one of the longest course, but also it is the least protected as it does not have a dural covering. In this particular case, the presence of a cavernous sinus thrombosis cannot be ruled out as well due to the numerous filling defects present on the scan. This can certainly cause bilateral abducens palsy due to the obvious reason that the nerves run directly through the cavernous sinuses. Another possible explanation for the abducens palsy is the extension of the inflammation of the thrombosed sinuses directly through their walls to the abducens nerve, especially of the inferior petrosal sinus to the abducens nerve, which lies just adjacent to it in Dorello's canal.5 This holds true especially for Gradenigo's syndrome.
One could argue that the case at hand could mimic a clinical picture of Gradenigo's syndrome, which is petrous apicitis. Patients with Gradenigo's syndrome typically present with a discharging ear, retro-orbital pain due to V1 involvement and unilateral lateral rectus palsy. The diagnosis can be confirmed by the presence of apicitis on a CT scan or MRI. The patient in this case had bilateral abducens palsy and did not have a classical retro-orbital pain. Furthermore, sinus thrombosis instead of apicitis was visible on imaging.
Lemierre's syndrome, a ‘forgotten’ disease due to the advent of new antibiotics, also referred to as postanginal sepsis, was relatively common in the preantibiotic era.7 Fusobacterium necrophorum, a type of non-spore-forming anaerobe, is responsible for this condition.7 Lemierre's syndrome may follow an episode of pharyngotonsillitis.8 Characteristically, it is comprised of septic thrombosis of the internal jugular vein and bacteraemia, leading to metastatic abscess formation.8 Hence, in a previously healthy young adult who develops an otogenic infection and subsequent septic thrombosis and thrombophlebitis, it would be wise to bear this life-threatening condition in mind. There has been a report of craniocervical abscess with extensive sinus thromboses failing to improve with conventional incision and drainage and standard intravenous antibiotic therapy.9 Specific culture and isolation of Fusobacterium species with targeted appropriate antibiotic therapy managed to treat a patient effectively.9 This reiterates the importance of specific cultures for F necrophorum, which, looking back in hindsight, could have been carried out in this patient and may be worth considering for similar patients, as in this case, in the future.
Another fact to bear in mind is to never miss ruling out nasopharyngeal carcinoma as this malignancy can present with a myriad of symptoms, especially such as in this case. A point worth considering is the fact that the patient in this case made a remarkably well early recovery with good symptom resolution, probably due to the early aggressive institution of anticoagulant therapy, antibiotics and regular ear care.
Learning points.
Chronic suppurative otitis media is a condition commonly treated in the general practice or otorhinolaryngology set-up.
When intracranial complications do occur, they carry a high morbidity and death rate along with them.
Aggressive early treatment can significantly reduce the morbidity of dural sinus thrombosis.
Early referral of a complicated otitis media to an otorhinolaryngology set-up is extremely crucial in determining the subsequent outcome of the patient.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Van dn Bosch MA, Vos JA, de Letter MA, et al. MRI findings in a child with sigmoid sinus thrombosis following mastoiditis. Pediatr Radiol 2003;33:877–9 [DOI] [PubMed] [Google Scholar]
- 2.Samul J, Fernandes CMC, Steinberg JL. Intracranial otogenic complications: a persisting problem. Laryngoscope 1986;96:272–8 [DOI] [PubMed] [Google Scholar]
- 3.Shrader EC, Schlezinger NS. Neuro-opthalmologic evaluation of abducens nerve paralysis. Arch Ophthalmol 1960;63:84–91 [DOI] [PubMed] [Google Scholar]
- 4.Lang M, Schmidbauer J, Voges M, et al. Mono- or bilateral abducens paralysis as the initial symptom of sinus vein thrombosis. Ophthalmologe 2002;99:49–52 [DOI] [PubMed] [Google Scholar]
- 5.Leonard TJK, Moseley IF, Sanders MD. Ophthalmoplegia in carotid cavernous sinus fistula. Br J Ophthalmol 1984;68:128–34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Newton T, Hoyt W. Dural arteriovenous shunts in the region of the cavernous sinus. Neuroradiology 1970;1:71–81 [Google Scholar]
- 7.Riordan T. Human Infection with fusobacterium necrophorum (necrobacillosis), with a focus on Lemierre's syndrome. Clin Microbiol Rev 2007;20:622–59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stokroos RJ, Manni JJ, de Kruijk JL, et al. Lemierre syndrome and acute mastoiditis. Arch Otolaryngol Head Neck Surg 1999;125:589–91 [DOI] [PubMed] [Google Scholar]
- 9.Price K, Wilson L, Tsegaye M. A case of craniocervical abscess with sinus thrombosis in Lemierre's syndrome. Br J Neurosurg 2012;26:426–8 [DOI] [PubMed] [Google Scholar]