Abstract
Tuberous sclerosis complex (TSC) is an autosomal dominant multisystem disorder caused by mutations in either of the two genes, TSC1 or TSC2, which code for the proteins hamartin and tuberin, respectively. These proteins act as tumour-growth suppressors with mutations in their genes leading to multiple hamartomatous growths throughout the central nervous system, lungs, heart, kidneys, eyes and skin. There have been reports of patients with TSC having an increased incidence of cardiac neoplasms, especially rhabdomyomas. A much smaller proportion of TSC patients have also been reported to have either, angiomyolipomas or lipomas, the diagnosis in these cases being made via CT. We present the first case of an adult with TSC, where a histological diagnosis of cardiac lipoma was made and discuss its implications.
Background
Tuberous sclerosis complex (TSC) is an autosomal dominant multisystem disorder caused by mutations in either of two genes, TSC1 and TSC2, which code for the proteins hamartin and tuberin, respectively. These proteins act as tumour-growth suppressors with mutations in their genes leading to multiple hamartomatous growths throughout the central nervous system, lungs, heart, kidneys, eyes and skin. TSC usually consists of a classic triad of facial angiofibromas, mental retardation and seizures, although only 30% of patients have all the three symptoms together. Patients with TSC have been reported to have an increased incidence of benign cardiac neoplasms, with 50–65% of them being rhabdomyomas.1 There have also been reports of patients with TSC having developed intramyocardial lipomatous lesions which were thought to be either angiomyolipomas or lipomas.2 In these reports, CT was the primary mode of investigation, which resulted in the lesions being strongly suspicious of angiomyolipomas rather than lipomas. There are also some reports of lipomas, diagnosed via CT and MRI, in children with TSC.3 No histological diagnosis of these cardiac lipomatous lesions was made in these reports. We present the first case of an adult with TSC, where a histological diagnosis of cardiac lipoma was made.
Case presentation
A middle-aged individual with a 40-year history of TSC was found on the floor at home by a friend. It was confirmed that the individual was dead and hence an autopsy was carried out to determine the cause of death. On gross examination of the heart, a lipomatous lesion of 20 mm was noted in the left ventricle.
A tissue sample from the heart was obtained for histology. Histological examination confirmed that the lesion was a lipoma. There was no evidence of smooth muscle component or abnormal blood vessels (figure 1).
Figure 1.
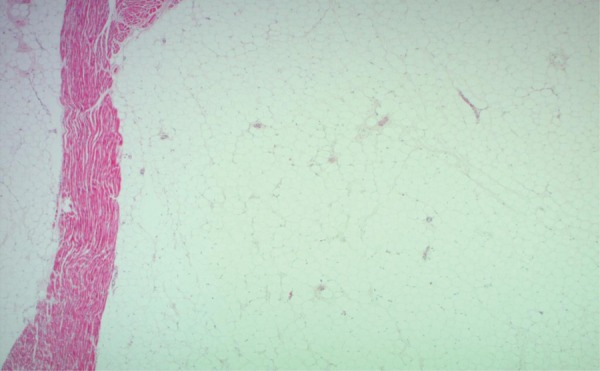
Histology of the cardiac lesion showing striated cardiac muscle with adjacent solid population of adipocytes without smooth muscles or abnormal vessels.
In addition, histology confirmed the presence of bilateral multiple angiomyolipomas in the kidneys (figure 2) and features of a subependymal giant cell astrocytoma and hippocampal sclerosis in the brain. The cause of death appeared to be due to an epileptic fit secondary to subependymal giant cell astrocytoma and hippocampal sclerosis.
Figure 2.
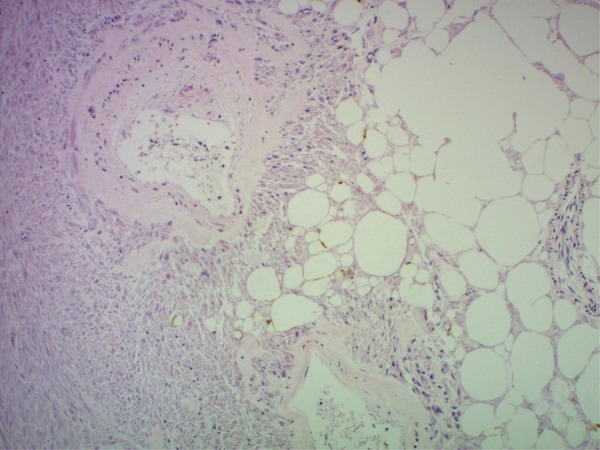
Renal angiomyolipoma showing three components; adipose tissue, smooth muscle fibres and abnormal blood vessels are noted.
Discussion
Cardiac lipomas account for around 4% of benign cardiac tumours and consist of adipose tissue.4 Cardiac lipomas occur most commonly in the pericardial space. They may also occur in the myocardium, most commonly in the left ventricle, right atrium and interatrial septum. Occasionally, they may contain muscle or vascular tissue, but rarely result in haemorrhage. They are usually asymptomatic and are only discovered incidentally via imaging investigations such as echocardiography or CT/MRI. They are usually solitary tumours, as in our case.
It is difficult to distinguish a lipoma from other lesions which may have a similar consistency such as angiomyolipomas via imaging techniques alone. Histological diagnosis would be considered the gold standard. This is, however, not often necessary as lipomas are commonly benign.
It is clear from our case that apart from rhabdomyomas (which are a common intracardiac finding in patients with TSC) and angiomyolipomas, intracardiac lipomas are another possible differential diagnosis for incidental intracardiac lesions found in these patients. However, imaging alone may be sufficient to differentiate a rhabdomyoma from a lipoma, while differentiating an angiomyolipoma from a lipoma may not be as easy.5 It may be important to differentiate between the two as angiomyolipomas have a risk of haemorrhage and hence may require pre-emptive embolisation. In such cases, cardiac CT may be more useful owing to its wide field of view and increased spatial resolution.
Learning pointss.
TSC is an autosomal dominant multisystem disorder caused by mutations in either of the two genes, TSC1 or TSC2, which result in the growth of multiple hamartomatous lesions throughout the central nervous system, lungs, heart, kidney, eyes and skin.
Patients with TSC have an increased risk of developing benign cardiac neoplasms, including rhabdomyomas (most common), angiomyolipomas and lipomas (less common).
Rhabdomyomas may be differentiated from angiomyolipomas and lipomas by standard imaging techniques alone; however, it may be difficult to differentiate angiomyolipomas from lipomas via these standard techniques alone. Thus, we suggest that cardiac-specific imaging techniques such as cardiac CT be used in such cases. This is because angiomyolipomas have a risk of spontaneous haemorrhage which may require pre-emptive embolisation.
The gold standard technique for diagnosing an intracardiac neoplasm is via histological examination. This is, however, not always possible or necessary as newer cardiac imaging techniques have made differentiating the various lesions much easier.
Footnotes
Contributors: SJ was responsible for writing up the entire case report. SA-H was responsible for editing the manuscript and obtaining pictures of the histology samples. He also annotated the pictures.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review : Not commissioned; externally peer reviewed.
References
- 1.Nir A, Tajik AJ, Freeman WKet al. Tuberous sclerosis and cardiac rhabdomyoma. Am J Cardiol 1995;76:419–21 [DOI] [PubMed] [Google Scholar]
- 2.Winterkorn EB, Dodd JD, Inglessis I, et al. Tuberous sclerosis complex and myocardial fat-containing lesions: a report of four cases. Clin Genet 2007;71:371–3 [DOI] [PubMed] [Google Scholar]
- 3.Lichtenberger JP, Woo JKH, Venkatesh V, et al. Cardiac lipoma in a patient with tuberous sclerosis complex. Cardiovascular images http://www.mghcardiovascimages.org/index.php?src=gendocs&ref=cv_september_2010 (accessed 17 Aug 2012)
- 4.Salanitri JC, Pereles FS. Cardiac lipoma and lipomatous hypertrophy of the interatrial septum: cardiac magnetic resonance imaging findings. J Comput Assist Tomogr 2004;28:852–6 [DOI] [PubMed] [Google Scholar]
- 5.Luna A, Ribes R, Caro P, et al. Evaluation of cardiac tumours with magnetic resonance imaging. Eur Radiol 2005;15:1446–55 [DOI] [PubMed] [Google Scholar]


