Abstract
We report the case of a 30-year-old housewife who presented with fever and lower abdominal pain, and was diagnosed with an adnexal collection. Initial evaluation was suggestive of tubercular pelvic inflammatory disease (PID). Subsequently, from a culture of pus aspirated from the collection grew out Nocardia species. She was treated with amikacin and cotrimoxazole and made a complete recovery. Clinical and laboratory evaluation for immunosuppression was negative. Primary abdominal nocardiosis is an unusual cause for PID and an important differential diagnosis for tuberculosis.
Background
Pelvic inflammatory disease (PID) is a potentially underdiagnosed condition, especially in developing countries. It is characterised by inflammation of the upper female reproductive tract due to infection with a variety of organisms including Neisseria gonorrhoea, Chlamydia trachomatis, Escherichia coli, Trichomonas vaginalis and anaerobes. PID can also develop as a complication of granulomatous salpingitis due to Mycobacterium tuberculosis. Tubercular PID is particularly common in countries with a high prevalence of tuberculosis such as India.1
PID has a propensity to spread to adjacent pelvic organs. Advanced cases can develop perihepatitis; this is known as the Fitz–Hugh–Curtis syndrome.2 In addition to the risk of systemic dissemination of infection, PID can also produce local complications including infertility and ectopic pregnancy. Indeed, the WHO estimates that up to 40% of all cases of female infertility and 50% of all tubal pregnancies can be attributed to PID.3
In the absence of adequate laboratory facilities, it is often useful for physicians in the Indian subcontinent to rely on the syndromic approach to PID. The major drawback of an empiric approach is the tendency to overdiagnose pelvic tuberculosis—a natural consequence of the high prevalence of female genito-urinary tuberculosis within the subcontinent.1
This case highlights nocardiosis as an aetiological agent for PID. Although extremely unusual in immunocompetent individuals, abdominal nocardiosis should be considered as a differential diagnosis for tubercular PID.
Case presentation
A 30-year-old woman presented with low-grade fever with evening rise since the past 2 weeks. She also complained of dull aching pain over the left lower part of her abdomen since the past 1 week. She denied significant weight loss or night sweats. There was no alteration in bowel or bladder habits. Her menstrual cycles were regular. She had never been in contact with diagnosed cases of tuberculosis. There was no history of abdominal surgeries or intrauterine contraceptive usage in the past. She had never received steroid or immunosuppressant medication in any form and she denied any history of substance abuse.
At admission, the patient was haemodynamically stable. General examination ruled out significant lymphadenopathy. Abdominal palpation revealed tenderness in the left iliac fossa. There were no palpable masses. Respiratory examination was normal.
Investigations
Routine laboratory tests showed mild leucocytosis (total leucocyte count: 12 300 cells/µl) and an elevated erythrocyte sedimentation rate (ESR: 95 mm/h). Other tests including blood glucose (random blood glucose: 91 mg/dl), renal (serum creatinine 1.0 mg/dl) and liver function tests were normal. Urinalysis was unremarkable. Abdominal ultrasonography showed a left adnexal collection extending into the anterior abdominal wall. CT was confirmatory (figure 1). Pus was aspirated from the collection under ultrasonic guidance. Analysis revealed low glucose (5 mg/dl) and high protein (5.2 g/dl). Adenosine deaminase level was also elevated (222 U/l). Cytology showed 41 600 leucocytes/µl; predominantly neutrophils. Gram staining was negative for bacteria. Although Ziehl–Neelsen staining ruled out the presence of acid fast bacilli, pus culture was performed for M tuberculosis. Mantoux tuberculin skin test was negative. Chest x-ray did not show any stigmata of tubercular infection. HIV serology by ELISA technique was negative.
Figure 1.
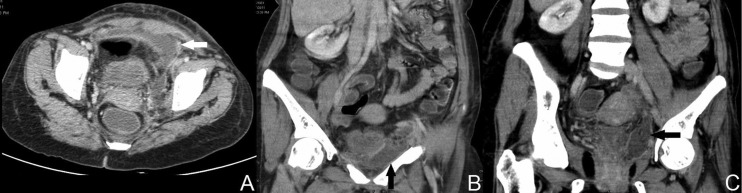
CT of the abdomen (axial section) showing left adnexal collection (white arrow, A). Note collection in coronal section (black arrows, B, C).
Subsequently aerobic culture of the aspirate on Sabouraud dextrose agar yielded a growth of Nocardia species, sensitive to amikacin and cotrimoxazole. Mycobacterial culture remained sterile after 6 weeks of incubation.
Differential diagnosis
Primary abdominal nocardiosis involving the pelvic adnexa
Tubercular pelvic inflammatory disease with extension into the abdominal wall
Pyogenic pelvic abscess (unlikely, as both gram stain and culture did not yield any pyogenic organism).
Treatment
The patient was treated with amikacin (750 mg intravenous every 24 h) for 14 days and cotrimoxazole (960 mg orally every 6 h) for 6 months, in accordance with the sensitivity of the isolate. Drainage of the collection was deferred due to its small size and the relatively asymptomatic condition of the patient.
Outcome and follow-up
The patient tolerated antibiotic therapy and made a complete recovery over the next 6 months with full resolution of her symptoms. Follow-up ultrasonography confirmed resolution of the adnexal collection. She remains asymptomatic on follow-up 1 year after the index illness.
Discussion
Nocardiosis results from infection with members of the genus Nocardia—an aerobic actinomycete. It preferentially involves the lungs, skin and subcutaneous tissue and the central nervous system; haematogenous spread from a pulmonary focus can result in disseminated systemic infection.4 Primary abdominal nocardiosis without evidence of systemic or pulmonary infection is rare and typically limited to immunocompromised individuals. AIDS, prolonged corticosteroid therapy, administration of immunosuppressive drugs, continuous ambulatory peritoneal dialysis and chronic medical illness constitute the principal risk factors for nocardiosis.5 In contrast, medical literature on abdominal nocardiosis in immunocompetent individuals is restricted to a handful of individual case reports.
Saeed et al6 reported a case of nocardial intra-abdominal abscess in a young female with Crohn's disease. The presentation of this patient with fever and abdominal pain was similar to our own; the authors also emphasised that their patient had never received immunosuppressive therapy for Crohn's disease. Nevertheless, the presence of Crohn's disease by itself could have led to some degree of immunosuppression; as noted above, chronic illness is a recognised risk factor for nocardial infection.
Another case report by Patil et al7 described abdominal nocardiosis mimicking ovarian malignancy in an immunocompetent individual. The patient in question underwent extensive surgery including total hysterectomy, salpingo-oophorectomy and local lymph node dissection. Histopathological examination of tissue samples from these organs then revealed the true diagnosis of nocardiosis. This case clearly demonstrated an atypical presentation of nocardiosis as well as the peril of overlooking nocardiosis as a differential diagnosis of PID. In our instance, culture of Nocardia from the aspirated pus allowed for timely initiation of appropriate antibiotic therapy; the patient made a complete recovery without further incident.
The patient described by Patil et al had also received an intrauterine contraceptive device 3 years prior to the index illness. Nocardiosis is known to occur after percutaneous inoculation,4 and the implanted device most likely provided the route of infection. In our own instance, there was no such history of instrumentation in the past. The source and route of Nocardia infection is therefore obscure.
Learning points.
Abdominal nocardiosis can produce pelvic inflammatory disease.
Although rarely encountered, abdominal nocardiosis can occur in immunocompetent individuals.
Abdominal nocardiosis can masquerade as tuberculosis, and should be considered as a differential diagnosis.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Avan BI, Fatmi Z, Rashid S. Comparison of clinical and laparoscopic features of infertile women suffering from genital tuberculosis (TB) or pelvic inflammatory disease (PID) or endometriosis. J Pak Med Assoc 2001;51:393–9 [PubMed] [Google Scholar]
- 2.Peter NG, Clark LR, Jaeger JR. Fitz–Hugh–Curtis syndrome: a diagnosis to consider in women with right upper quadrant pain. Cleveland Clin J Med 2004;71:233–9 [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. 2011. Sexually transmitted infections. http://www.who.int/mediacentre/factsheets/fs110/en/ (accessed 2 Dec 2012).
- 4.Corti ME, Villafañe-Fioti MF. Nocardiosis: a review. Int J Infect Dis 2003;7:243–50 [DOI] [PubMed] [Google Scholar]
- 5.John MA, Madiba TE, Mahabeer P, et al. Disseminated nocardiosis masquerading as abdominal tuberculosis. S Afr J Surg 2004;42:17–19 [PubMed] [Google Scholar]
- 6.Saeed S, Varela JE, Nelson RL, et al. An unusual case of intra-abdominal nocardia abscess detected by Tc-99m HMPAO-labeled WBC study. Clin Nucl Med 2004;29:270–1 [DOI] [PubMed] [Google Scholar]
- 7.Patil RN, Bafna UD, Pallavi VR, et al. Successful intra-peritoneal antibiotic therapy for primary abdominal nocardiosis in an immunocompetent young female masquerading as carcinoma ovary. Online J Health Allied Sci 2011;10:11 [Google Scholar]


