Abstract
We report the case of an adult male patient who was admitted to our hospital with a diagnosis of vivax malaria complicated with renal insufficiency and acute respiratory distress syndrome (ARDS). The patient was treated with intravenous artesunate. He was intubated and mechanically ventilated and taken up for haemodialysis in view of worsening renal parameters. He developed tachycardia a few hours later. ECG showed sinus tachycardia. Tachycardia persisted though the blood pressure was normal, there was no evidence of bleeding, and the heart was clinically normal. We tried to control the heart rate with diltiazem, adenosine and metoprolol but the tachycardia persisted. The heart rate was finally controlled with amiodarone. The patient improved, was weaned off from the ventilator and extubated. His renal functions gradually improved. Oral amiodarone was continued and there was no recurrence of tachycardia. We present this case to highlight the interesting association of vivax malaria with persistent, difficult to treat tachycardia.
Background
Vivax malaria was previously considered to be benign tertian malaria. However, patients with severe Plasmodium vivax mono infection are being recognised more frequently. Although the incidence of complicated vivax malaria is increasing, cardiac complications have been only infrequently reported. We write this case to highlight that tachyarrhythmia is a possible complication of vivax malaria. With worldwide travel and globalisation, diseases are no longer strictly limited to specific geographical areas and it behoves physicians to have at least a passing familiarity not just with common infectious diseases, but also with their complications and rare manifestations so that these can be identified and treated.
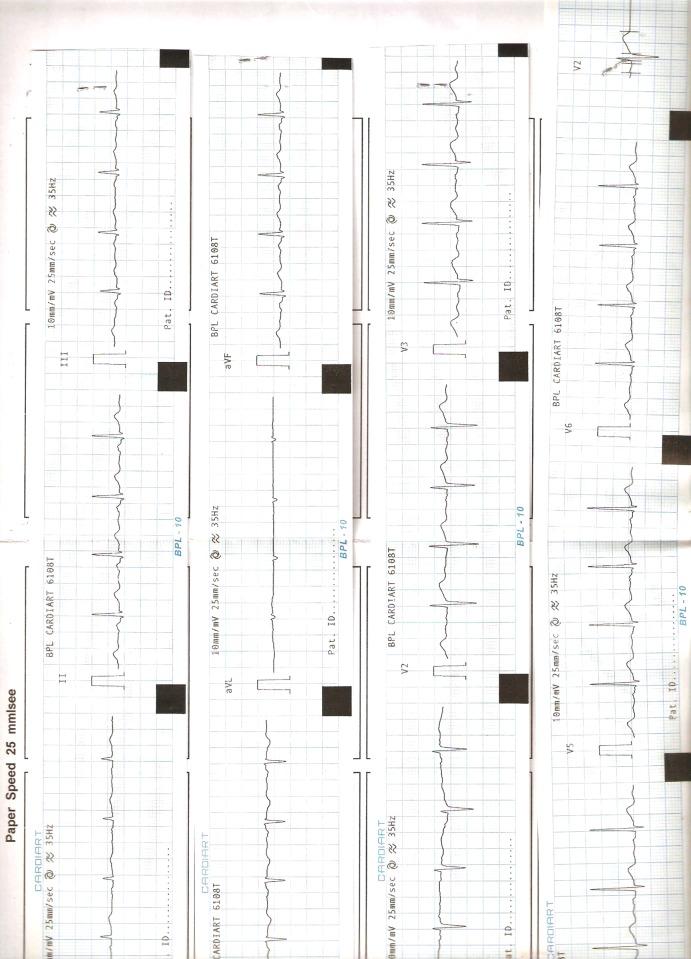
Figure 1.
ECG showing supraventricular tachycardia.
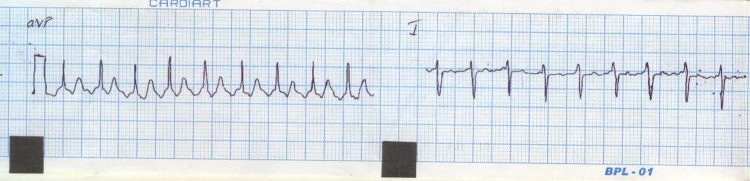
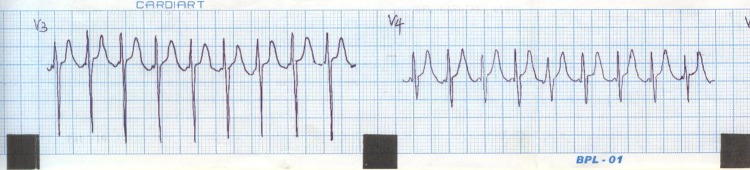
Figure 2.
ECG showing supraventricular tachycardia.
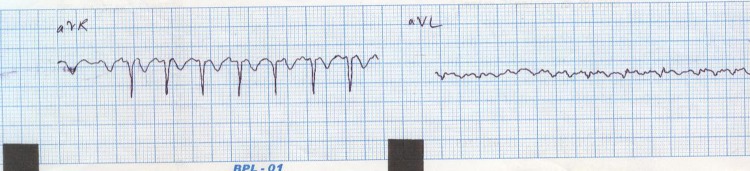
Figure 3.
ECG showing supraventricular tachycardia.
Figure 4.
ECG showing supraventricular tachycardia.
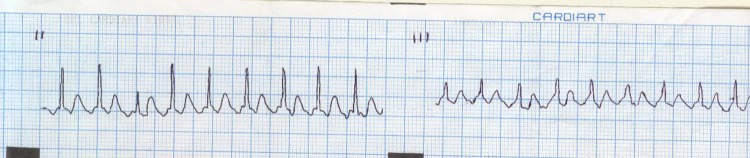
Figure 5.
ECG after treatment.
Case presentation
A 23-year-old male manual labourer, presented with a history of high-grade fever associated with chills and rigours. He also complained of severe bifrontal headache, two episodes of vomiting and decreased urine output. He was admitted to a peripheral hospital where he was diagnosed to have had vivax malaria with acute kidney injury. On the second day in the hospital the patient complained of breathlessness. He was found to be tachypneic and his pulse oximetry showed an SpO2 of 74%. The patient was endotracheally intubated and shifted to our hospital for further management.
On presentation to our hospital the patient was conscious and obeying verbal commands. His blood pressure was 130/80 mm Hg, respiratory rate was 40 cycles/min and he had no fever. He was icteric. Mild pallor was present.
His cardia and lungs were clear. Abdominal and central nervous system examination did not reveal any abnormality.
Investigations
Haemoglobin—12.9 g%
Total count —21 300 cells/mm3
Differential count —N93 L5 E1 M1
Erythrocyte sedimentation rate —57 mm
Platelets—57 000
Urine—protein ++, rest normal
Urea—159 mg%
Creatinine—5.5 mg%
Sodium—129 mEq/l
Potassium—8.3 mEq/l
Chlorine—91
Creatine phosphokinase (CPK)—6516
Lactate dehydrogenase—7311
Serum glutamic oxaloacetic transaminase (SGOT)—2203
Serum glutamic pyruvate transaminase (SGPT)—2260
Total bilirubin—2.7 mg%
Direct—2.2 mg%
Indirect—0.5 mg%
Calcium—7.7
Albumin—3.4
Peripheral smear—ring forms and schizonts of P vivax seen +
Treatment
The patient was managed as a case of severe, complicated malaria with acute renal insufficiency and acute respiratory distress syndrome (ARDS). He was treated with intravenous artesunate and antibiotics along with supportive therapy. He was mechanically ventilated—SIMV with pressure support with FiO2 of 60% and a PEEP of 10. In view of persisting oliguria, hyperkalemia and worsening renal parameters, femoral catheterisation was done, and haemodialysis was initiated.
Two hours after completion of the first session of dialysis, the patient was noted to have a heart rate of 180 bpm. However, there was no hypotension or fall in haematocrit. ECG showed sinus tachycardia. A 2 dimensional echocardiogram done to rule out structural myocardial damage was normal. The tachycardia persisted even after the administration of Inj metoprolol 5 mg intravenous 3 times.
Inj adenosine 6 mg intravenous over 3 s was administered. The heart rate transiently dropped to 96 bpm. The effect of adenosine did not last however, and the tachycardia persisted. In view of persistent tachycardia, and all other measures having failed, Inj amiodarone 150 mg intravenous was administered over 10 min followed by amiodarone infusion at 1 mg/min for 6 h. The tachycardia responded to amiodarone and finally stabilised at 90/min.
Meanwhile, the antimalarials, antibiotics and haemodialysis were continued. The patient gradually improved and was weaned off from the ventilator, was extubated and shifted to the ward. The patient's renal function gradually improved with progressively increasing urine output. There was no recurrence of tachycardia.
Outcome and follow-up
The patient was stable on discharge with normal renal function and stable vitals.
Discussion
Malaria is a disease caused by the protozoans Plasmodium falciparum, Plasmodium vivax and Plasmodium ovale and is transmitted by the infected anopheles mosquito. The estimated annual incidence of malaria varies at 10–500 million cases annually. It causes approximately 1 million deaths a year. Malaria is a disease of the tropics—with the annual incidence being highest in sub Saharan Africa and South East Asia.1
Traditionally, vivax malaria is considered to be relatively benign and has even been termed as benign tertian malaria. However, vivax malaria causing complications is being reported with increasing frequency.2 This patient had severe malaria as indicated by the neutrophilia, increased CPK, SGOT and SGPT.
P falciparum can cause severe infections and can be complicated by ARDS, acute kidney injury, hypoglycaemia, cerebral malaria and metabolic acidosis. Cardiac complications due to malaria or the drugs used in its treatment have been reported to be infrequent.3
Malaria can affect the heart by causing myocarditis4 and ischaemic heart disease.5 Cardiac dysfunction has been reported in children with hypovolemia and metabolic acidosis as a consequence of severe malaria.6
Tachycardia and tachyarrhythmia seen in malaria are mainly a consequence of the treatment and can be caused by amodiaquine and halofantrine. Quinine, used extensively in the treatment of malaria in the preartesunate era is known to affect the conduction system causing broad complex tachycardia and death.7 Artemether, with which we treated the patient, does not significantly affect the pulse or blood pressure and does not result in ECG changes.8 We present this case to highlight the fact that vivax malaria can have a complicated course and that malaria can affect the heart and its conducting system.
Learning points.
Vivax malaria can be severe and complicated by acute respiratory distress syndrome (ARDS) and acute kidney injury.
Malaria can affect the heart and its conducting system.
Amiodarone can be tried to treat tachycardia associated with malaria.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Murray CJL, Lopez AP, eds. The global burden of disease: a comprehensive assessment of mortality and disability from diseases, injuries and risk factors in 1990 and projected to 2020. Geneva: World Health Organization, 1996 [Google Scholar]
- 2.Bammigatti C, Shetty S, Shetty S, et al Benign tertian malaria—a misnomer? Trop Doct 2011;41:168–9 [DOI] [PubMed] [Google Scholar]
- 3.Bethell DB, Phuong PT, Phuong CX, et al Electrocardiographic monitoring in severe falciparum malaria. Trans R Soc Trop Med Hyg 1996;90:266–9 [DOI] [PubMed] [Google Scholar]
- 4.Mohsen AH, Green ST, West JN, et al. Myocarditis associated with plasmodium falciparum malaria: a case report and a review of the literature. J Travel Med 2001;8:219–220 [DOI] [PubMed] [Google Scholar]
- 5.Jain K, Chakrapani M. Acute myocardial infarction in a hospital cohort of malaria. J Global Infect Dis 2010;2:72–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yacoub S, Lang HJ, Shebbe M, et al. Cardiac function and hemodynamics in Kenyan children with severe malaria. Crit Care Med 2010;38:940–5 [DOI] [PubMed] [Google Scholar]
- 7.Morrison LD, Velez LI, Shepherd G, et al. Death by quinine. Vet Hum Toxicol 2003;45:303–6 [PubMed] [Google Scholar]
- 8.Kochar DK, Joshi A, Vallabh B, et al. Effect of arteether on electrocardiogram in the patients of falciparum malaria—a preliminary study. Indian J Malariol 1999;36:61–4 [PubMed] [Google Scholar]