Abstract
Haemangioma is the most common benign tumour of the liver. Most of them are small in size (less than 4 cm) and are often asymptomatic and discovered incidentally on modern diagnostic imaging. Lesions with a diameter larger than 4 cm are called giant haemangiomas, and these are usually located in the right hepatic lobe. Although haemangioma is the most frequent benign tumour of the liver, ‘giant’ haemangiomas are rare. Such lesions may give rise to symptoms requiring treatment. In this case report, we describe the case of a 50-year-old Indian man who presented with giant liver haemangioma and systemic inflammatory manifestations.
Background
Haemangioma of the liver is a benign tumour of vascular origin with a reported incidence at autopsy of 0.4–20%. It is usually small (<4 cm) in dimension and is found in multiples in 20% of patients.1 It is composed of cavities lined with endothelial cells and filled with blood. It is usually of cavernous type. In children, a capillary pattern may be seen. Most of the cases with liver haemangioma are asymptomatic and discovered incidentally on a liver ultrasound or CT scan. Most patients with liver haemangioma have normal liver function tests. Rarely, it may present with signs and symptoms of acute inflammation with only a few cases being mentioned in the literature.2 In this article, we elaborate the clinical and radiological properties of such a case who presented with features of acute inflammation that normalised after surgical resection.
Case presentation
A 50-year-old Indian man presented to the outpatient department after being referred from a primary centre with chief complaints of lump in the epigastric region, fever, weight loss and progressive weakness since 11 months. The patient was a known alcoholic who was being evaluated for malignancy.
On physical examination of the patient, a hard non-tender lump was felt in the epigastric region, and mild pallor was noticed. There was no icterus, and no stigmata of chronic liver disease were present.
Investigations
On laboratory examination, the patient's haemoglobin was 9.7 gm/dl, total platelet count was 4.35 lac/mm3, erythrocyte sedimentation rate (ESR) was 60 mm in the first hour, and the fibrinogen level was 3.1/l (normal 1.5–2.77 g/l). However, the patient had a normal white cell count.
Liver function tests including serum glutamic oxaloacetic transaminase, serum glutamic pyruvic transaminase, alkaline phosphatase, gammaglutamyl transferase and bilirubin were normal. Blood sugar, blood urea and serum creatinine were within normal limits. Hepatitis B surface antigen and anti-hepatitis C virus antibodies were negative.
On radiological examination, ultrasound abdomen showed a large heterogeneous, predominantly hyperechoic mass lesion involving segments 2 and 3 of the left lobe of the liver with a few small, well-defined hyperechoic lesions in segments 4b and 7 of the liver (figure 1). The lesion in segments 2 and 3 of the liver was seen to be displacing the left hepatic vein laterally and compressing the pancreas posteriorly. On colour Doppler examination, no internal vascularity was seen in any of the lesions (figure 2). For further evaluation, a contrast-enhanced CT scan of the upper abdomen was advised, which showed a large heterogeneously enhancing predominantly hypodense lesion in segments 2 and 3 of the liver with a few well-defined non-enhancing hypodense lesions in segments 4b and 7 of the liver. On delayed scans, the lesions showed progressive centripetal enhancement characteristic of haemangioma (figure 3).
Figure 1.

Ultrasonography of the abdomen showing a well-defined large heterogeneous predominantly hyperechoic lesion in segments 2 and 3 of the liver.
Figure 2.

On colour Doppler imaging no internal vascularity is seen in the lesion.
Figure 3.
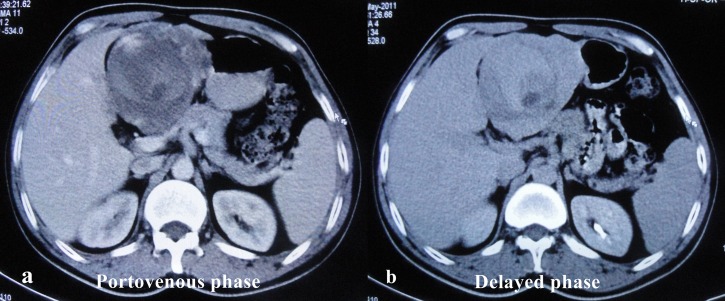
(A,B) Axial contrast-enhanced CT of the abdomen shows a low-density lesion with progressive centripetal enhancement on delayed images.
Treatment
Surgical resection of the mass was done.
Outcome and follow-up
Postoperative course was uneventful, and the patient recovered well. After surgical resection, the symptoms of the patient disappeared, and the ESR and fibrinogen levels normalised. Histopathological examination of the lesion was confirmatory of giant liver haemangioma (GLH).
Discussion
Although GLH is most often asymptomatic, there have been a few case reports of GLH associated with inflammatory manifestations. The underlying pathophysiology of the inflammatory process in patients with GLH is not fully understood. One theory suggests that cytokines released from hepatic macrophages and endothelial cells are responsible for the inflammatory process. Others consider the key mediator to be interleukin 1 and 6. The most likely explanation for the pain and increased ESR, C reactive protein and fibrinogen is thrombosis within the tumour.3 From an imaging standpoint, it is well known that GLH usually does not demonstrate the classic findings on either ultrasound, CT scan or MRI. On ultrasound, typically haemangiomas are small, well defined, homogeneous and hyperechoic. Larger lesions tend to be heterogeneous, with central hypoechoic areas corresponding to fibrous collagenous scars, large vascular spaces or both. Calcification is rare. On colour or duplex Doppler sonograpy, haemangiomas are characterised by extremely slow blood flow that will not routinely be detected. In general practice, ultrasound findings of haemangioma are often confirmed with a CT scan or MRI. Typical hepatic haemangiomas are often hypodense on precontrast CT scanning. In the arterial phase, there is peripheral enhancement in the lesion with the central portion typically remaining hypodense. In the portal venous and delayed phases, the enhancement is usually seen to progress centripetally.4 MRI is highly sensitive and specific in the diagnosis of hepatic haemangioma. On MRI, these lesions have well-defined margins and exhibit a low signal on T1- and high signal on T2-weighted images. In a similar fashion, the contrast uptake enhancement pattern is like that seen on dynamic CT scanning.5 With T2-weighted spin-echo and dynamic gadolinium-enhanced T1-weighted gradient-echo sequences, the reported sensitivity and specificity of MR imaging are 98% and the accuracy is 99%.6
Learning points.
Liver haemangiomas, although mostly asymptomatic, can sometimes present with systemic inflammatory manifestation.
Ultrasonography and CT scan are useful investigations in diagnosing giant haemangiomas of the liver.
Surgical resection of haemangiomas leads to remission of symptoms and fall in inflammatory markers.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Karhunen PJ. Benign hepatic tumours and tumour like conditions in men. J Clin Pathol 1986;39:183–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pol B, Disdier P, Le Treut YP, et al. Inflammatory process complicating giant hemangioma of the liver: report of three cases. Liver Transpl Surg 1998;4:204–7 [DOI] [PubMed] [Google Scholar]
- 3.Smyrniotis V, Kehagias D, Arkadopoulos N, et al. Liver hemangioma with systemic inflammatory manifestations. Am J Gastroenterol 2000;95:830–2 [DOI] [PubMed] [Google Scholar]
- 4.Scatarige JC, Kenny JM, Fishman EK, et al. CT of giant cavernous hemangioma. AJR Am J Roentgenol 1987;149:83–5 [DOI] [PubMed] [Google Scholar]
- 5.Choi BI, Han MC, Park JH, et al. Giant cavernous hemangioma of the liver: CT and MR imaging in 10 cases. AJR Am J Roentgenol 1989;152:1221–6 [DOI] [PubMed] [Google Scholar]
- 6.Vilgrain V, Boulos L, Vullierme MP, et al. Imaging of atypical hemangiomas of the liver with pathologic correlation. Radiographics 2000;20:379–97 [DOI] [PubMed] [Google Scholar]


