Abstract
Background
Multiple studies have demonstrated varying rates of successful endotracheal intubation (ETI). Until the application of video laryngoscopy, little information regarding prehospital intubation could be analyzed objectively by individuals other than the provider performing the ETI.
Objective
To evaluate the association of variables recorded during video laryngoscopy and successful ETI attempts, defined as placing the endotracheal tube in the trachea.
Methods
We retrospectively reviewed intubations performed by a single helicopter emergency medical service (HEMS) using a video larygoscope from March 1, 2010, to October 1, 2010. All videos were de-identified and analyzed by a single researcher. Time intervals (e.g., attempt time) and intubation process variables (e.g., Cormack-Lehane [C-L] view) were abstracted from all videos. Time intervals were begun when the laryngoscope blade passed the lips and entered the oral cavity (entry). We describe variables using means and standard deviations (continuous), medians with interquartile ranges (ordinal), and percentages with 95% confidence intervals (categorical). We then looked at univariate associations between these variables and ETI success using logistic regression.
Results
We recorded 116 intubations during the study period. Twenty-nine recordings were either incomplete (n = 26) or of insufficient quality for analysis (n = 3). The remaining 87 videos represented 87 different patients with a total of 102 attempts at laryngoscopy. Thirty-six providers performed 64 cases, with the majority of providers (n = 21) performing only one intubation. The first-pass success rate in this series was 76% (n = 66), with 98% success within three attempts. Successful ETI attempts had lower entry–to–percentage of glottic opening (POGO) times (16.6 sec vs. 32.1 sec, p = 0.013), entry–to–first view of the endotracheal tube or entry-to-tube times (17.6 sec vs. 27.4 sec, p = 0.04), higher POGO scores (76 vs. 39, p < 0.001), and a lower C-L view (one vs. three, p < 0.001). Recognized esophageal intubation was more likely to occur during unsuccessful ETI attempts (43% vs. 8%, p < 0.001).
Conclusion
Video laryngoscopy can measure multiple components of ETI performance. Successful ETI attempts have significantly shorter entry-to-POGO times and entry-to-tube times, obtain better views of the glottic opening (POGO and C-L view), and have a lower incidence of recognized esophageal intubation.
Keywords: airway, intubation, video laryngoscopy, helicopter emergency medical service (HEMS)
Introduction
Endotracheal intubation (ETI) is a critical skill performed by prehospital providers. Previous studies recommended ETI as the method to definitively secure an airway in the prehospital setting, whereas others have questioned its utility and argue that it puts patients at unnecessary risk.1–3 Endotracheal intubation is a complicated skill that requires a significant amount of training and continuing education to maintain proficiency.4 The rates of successful ETI on the first attempt (first-pass success) are poor (45%–85%).5–7 These rates are worrisome, as multiple ETI attempts and prolonged ETI attempts are associated with worse patient outcomes, including severe hypoxemia (saturation of peripheral oxygen [SpO2] <70%) and death, which can rapidly occur in the prehospital setting.8–10 It is important to accurately evaluate ETI in this environment to ensure proficiency and maintain patient safety.
Video laryngoscopy is a relatively new tool that provides substantial data for the analysis of ETI in the prehospital setting and may be used to review ETIs in the clinical setting. Until the application of video laryngoscopy, little information regarding prehospital intubation could be analyzed objectively by individuals other than the provider performing the ETI. This technology allows for detailed analysis of time intervals during ETI in addition to intubation process variables, including predictors of ETI difficulty (e.g., the C-L view) previously evaluated using direct laryngoscopy.11–14 We sought to evaluate the association between time intervals and intubation process variables and ETI success collected using video laryngoscopy.
Methods
This study was deemed exempt by the University of Pittsburgh Institutional Review Board. We obtained retrospective data from a quality improvement (QI) database. Videos were recorded during ETIs performed by crew members of a helicopter emergency medical service (HEMS) from March 1, 2010, to October 1, 2010. The HEMS medical director provided all videos collected during the eight-month interval after being de-identified of both patient and provider information.
The crew members are nurses and paramedics with prior training in airway management, including a minimum of three years of prior patient care experience. To maintain ETI proficiency, crew members are required to complete three successful intubations every three months. If the required intubations are not achieved while on duty, crew members must complete their requirements with anesthesiology supervision in the operating rooms of local hospitals. Through previous QI projects (local data, not published), we have determined the self-reported first-pass success rate for this HEMS agency to be 91%.
Six aircraft were equipped with video laryngoscopes (C-MAC, Karl Storz Corp., El Segundo, CA) that use a traditional #3 or #4 Macintosh laryngoscope blade with a video camera adjacent to the light source. This device digitally records the procedure to a flash memory card that was retrieved after the incident for offline review.
Aircraft were selected based on historical reviews of airway management indicating that the number and type of airway encounters (trauma vs. medical) were representative of the overall system. All flight crew members were instructed on C-MAC use before implementation and were allowed to practice using an intubating manikin. As part of the QI process, crew members were instructed to record all ETI attempts via the video laryngoscope, which were then reviewed by the HEMS medical directors. The HEMS medical director queried the electronic chart database for all ETI attempts performed from March 1, 2010, to October 1, 2010, to ensure that the videos collected represented all ETI attempts and not simply a convenience sample.
An attempt at ETI was defined by placing the blade of the laryngoscope into the patient’s mouth. Success at ETI was defined as passing the endotracheal tube into the trachea.
A single reviewer (JQ) examined these videos using commercial editing software (Final Cut Pro, Apple, Inc., Cupertino, CA). A second reviewer (JNC) rated 10% of the videos to evaluate interrater reliability using Cohen’s kappa for categorical/ordinal data and Pearson correlation coefficients for continuous data. Videos that were incomplete (e.g., turned off prior to intubation) or for which the video file was unable to be viewed (e.g., a corrupt file) were excluded from the analysis.
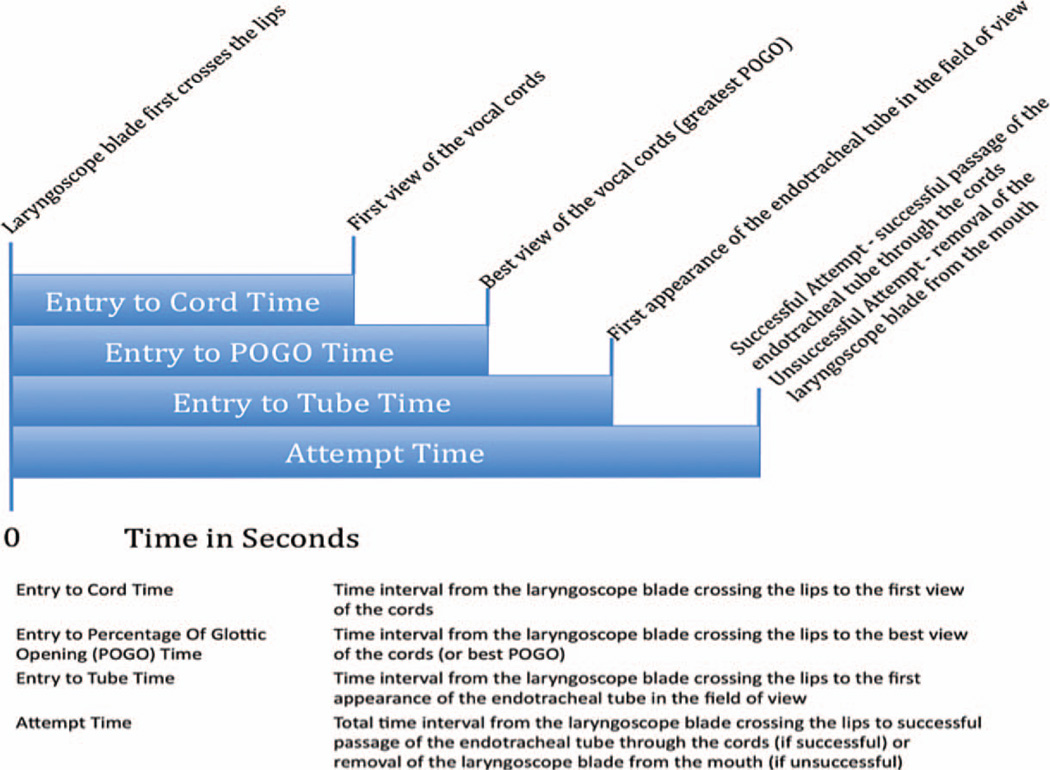
Variables recorded from the videos included both time intervals (Fig. 1) and intubation process variables (Table 1). The authors watched a sample of the videos prior to data analysis to compartmentalize and describe steps during ETI as recorded by video laryngoscopy. These steps, detailed in Figure 1, define time intervals from when the laryngoscope blade first enters the mouth by crossing the lips (time 0) until the vocal cords are first visualized (entry-to-cord time), until the best view of the glottic opening is obtained (entry–to–percentage of glottic opening [POGO] time), until the endotracheal tube first appears in view (entry-to-tube time), and until completion of the ETI attempt (attempt time). Completion of an ETI attempt was defined as either successfully passing the endotracheal tube into the trachea or removing the laryngoscope from the mouth (past the lips).
Figure 1.
Time interval variables. POGO = percentage of glottic opening.
Table 1.
Intubation Process Variables
| Variable | Definition |
|---|---|
| Percentage of glottic opening (POGO) score (0%–100%) | POGO is a validated score for determining the difficulty of an intubation11,12* |
| C-L view (1–4) | Technique for describing laryngeal view during laryngoscopy13 |
| Number of attempts | The total number of times the laryngoscope blade was put in the mouth |
| Esophageal Intubation (yes/no) | Was the endotracheal tube at any time during the attempt incorrectly placed in the esophagus as opposed to correctly placed in the trachea? |
| Number of forward movements | The number for forward movements made by the endotracheal tube prior to successful placement or aborting the attempt |
| First-pass success (yes/no) | Successfully passing the endotracheal tube past the vocal cords the first time the laryngoscope blade is placed in the patient’s mouth |
For complete reference citations, see the reference list.
POGO = percentage of glottic opening.
Intubation process variables (Table 1) were selected from variables associated with difficult ETI. We also examined the number of forward movements of the endotracheal tube recorded on the video to examine its association with ETI success.
Continuous variables were described using means with standard deviations. Ordinal variables were described using medians with interquartile ranges. Categorical variables were described using percentages with 95% confidence intervals (CIs). Because of the small sample size and small number of failed attempts at ETI, it was decided a priori to evaluate the associations between measured variables and ETI success using univariate logistic regression. Statistical analyses were performed using Stata version 11 (StataCorp LP, College Station, TX).
Results
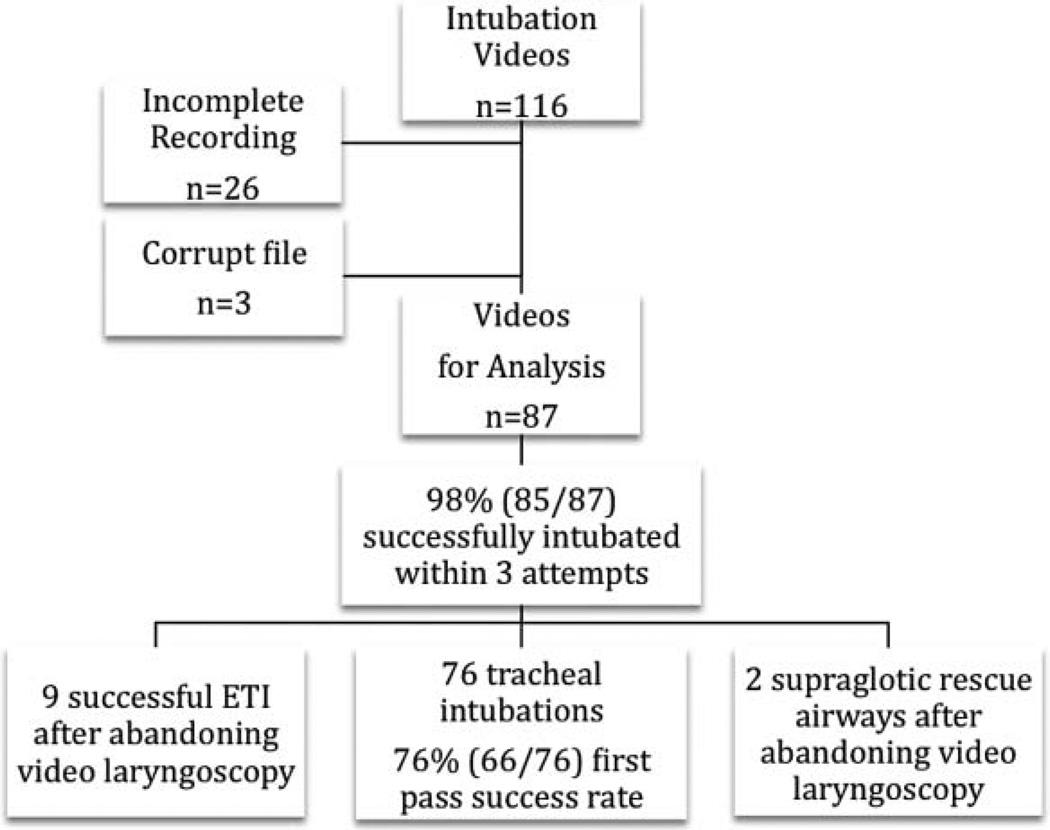
A total of 116 video files were collected over a six-month period. Twenty-nine were excluded because of corrupt data files (n = 3) or incomplete recordings where the video recording stopped prior to completing the intubation attempt (n = 26). Unique identification numbers were assigned to each provider to evaluate for clustering based on provider performance. A total of 36 unique providers performed 64 intubations. The majority of providers (n = 21) performed only one intubation. For 23 cases, the specific individual performing the intubation could not be identified from the recordings.
There were 102 ETI attempts for the 87 patients (Fig. 2). The trachea was successfully intubated using video laryngoscopy in 87% of cases (n = 76), with a first-pass success rate of 76% (n = 66). No ETIs in our data set had more than two attempts performed using video laryngoscopy. Whether the attempt was the first or second attempt at ETI did not predict success (odds ratio 0.64 [CI 0.20–2.07], p = 0.453). Tracheal intubation was not seen in 11 cases, either because the provider stopped video recording and appeared to have abandoned video laryngoscopy for direct laryngoscopy (n = 9) or inserted a supraglotic rescue device (n = 2). All direct laryngoscopy attempts were successful (9/9). The overall success rate for ETI in this case series was 98% within three attempts, which is similar to our previous QI chart reviews.
Figure 2.
Consolidated Standards of Reporting Trials (CONSORT) diagram of airway cases.
All time interval variables had a Pearson correlation coefficient between 0.960 and 0.999. The POGO scores (a continuous value between 0 and 100) had a Pearson correlation coefficient of 0.890. All ordinal variables were exact matches between the two reviewers, except for the C-L view (Cohen’s kappa = 0.65).
We describe the association of measured variables with first-pass success in Table 2. Successful ETI attempts had lower entry-to-POGO times (16.6 sec vs. 32.1 sec, p = 0.013) and entry-to-tube times (17.6 sec vs. 27.4 sec, p = 0.04). There was also an association between higher POGO scores (p < 0.001) and a lower C-L view (p < 0.001) and successful ETI attempts. There were instances in which the endotracheal tube inadvertently was placed in the esophagus; however, this was immediately identified before removing the laryngoscope and then correctly placed in the trachea. Recognized esophageal intubation was more likely to occur during unsuccessful ETI attempts (43% vs. 8%, p < 0.001).
Table 2.
Data for All Attempts, Unsuccessful Attempts, and Successful Attempts at Intubation
|
All Attempts (n = 102) |
Unsuccessful Attempts (n = 26) |
Successful Attempts (n = 76) |
Odds Ratio p-Value |
|
|---|---|---|---|---|
| Time interval variables—mean (±SD) | ||||
| Entry-to-cord time | 12.4 ( ± 12.5) | 18.7 ( ± 25.7) | 11.4 ( ± 8.8) | 0.103 |
| Entry-to-POGO time | 18.7 ( ± 16.4) | 32.1 ( ± 29.4) | 16.6 ( ± 12.4) | 0.013* |
| Entry-to-tube time | 18.6 ( ± 11) | 27.4 ( ± 18.4) | 17.6 ( ± 9.3) | 0.04* |
| Attempt time | 30.3 ( ± 23.9) | 35.8 ( ± 31.7) | 28.4 ( ± 20.5) | 0.181 |
| Intubation process variables | ||||
| POGO score—mean (±SD) | 66 ( ± 37) | 39 ( ± 45) | 76 ( ± 29) | <0.001* |
| C-L view—median (IQR) | 1 (1, 1) | 3 (1, 4) | 1 (1, 1) | <0.001* |
| Number of forward attempts—mean (SD) | 4.7 ( ± 6.5) | 8.3 ( ± 6.8) | 4.9 ( ± 6.6) | 0.131 |
| Esophageal intubation (95% CI) | 17% (n = 17) (10–25) | 43% (n = 11) (23–63) | 8% (n = 6) (3–16) | <0.001* |
Statistically significant differences between successful and unsuccessful attempts.
CI = confidence interval; IQR = interquartile range; POGO = percentage of glottic opening; SD = standard deviation.
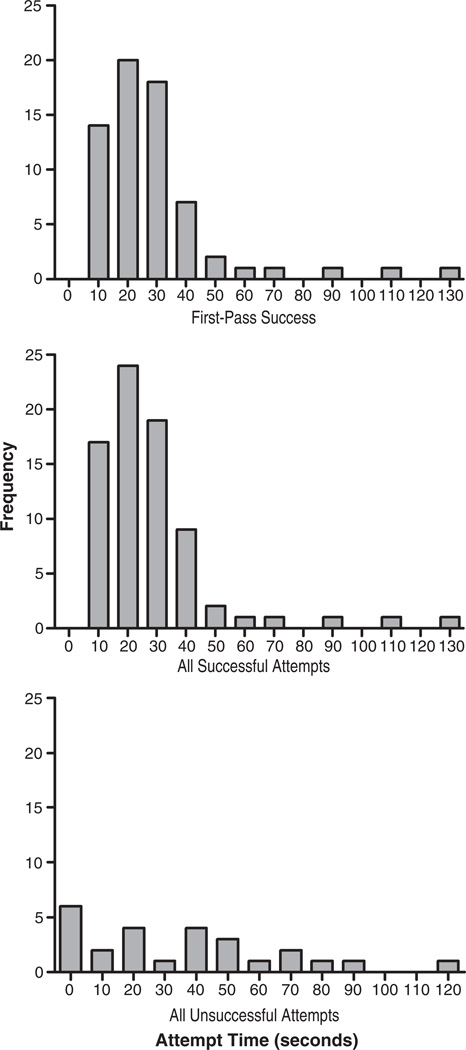
Attempt times were not different between successful and unsuccessful attempts. Figure 3 shows the distribution of attempt durations for those where first-pass success was achieved, any successful attempt (whether first or second), and any unsuccessful attempt. The progressions of steps did appear to be different between the two groups. Successful ETI attempts progressed through motions as shown in Figure 1. Unsuccessful attempts, on average, had entry-to-tube times that were less than entry-to-best-POGO times, possibly indicating that efforts were made to pass the endotracheal tube before obtaining the best view of the glottic opening. Sample videos can be viewed by accessing the airway research tab at the following link: http://www.emergencymedicine.pitt.edu/research.
Figure 3.
Attempt time for those with first-pass success (top); any successful attempts, including both first and second attempts (middle); and all unsuccessful attempts whether first or second overall attempt (bottom).
Discussion
Improving ETI in the prehospital setting is a challenging task. Until the advent of video laryngoscopy, little objective information was available for ETI proficiency beyond individual recall and self-report. Although the review of these videos does not directly change clinical care at the time of intubation, video laryngoscopy provides a new level of detail to the analysis of prehospital ETI that was previously unavailable and allows for more formal evaluation of ETI. This tool may be used to review ETIs and assist with QI.
Video laryngoscopy can be used to evaluate the associations between ETI success and both time intervals and intubation process variables. We found an association between successful ETI attempts and several of these measured variables. Successful ETI attempts had shorter entry-to-POGO times, shorter entry-to-tube times, higher POGO scores, and a lower C-L view. These data suggest that it is not only important to obtain a good view of the vocal cords, but that successful attempts obtain this view rapidly. This would suggest that if individuals do not quickly obtain an adequate view of the vocal cords, the attempt is likely to be unsuccessful and the provider should rapidly change strategies or abort the attempt.
Successful ETI attempts also have shorter entry-to-tube times, indicating that once the best view of the glottic opening is obtained, the endotracheal tube quickly enters the field of view. Alternatively, unsuccessful attempts in our data appear to have a progression whereby the endotracheal tube enters the field of view before the best view of the glottic opening is obtained and, as a result, these unsuccessful attempts have shorter entry-to-tube times than entry-to-POGO times. On review of these videos, it appeared as though successful attempts had a standard progression of ETI steps: 1) laryngoscope blade first crosses the lips, 2) first view of the vocal cords, 3) best view of the vocal cords, 4) endotracheal tube appears in view, and 5) successful placement of the endotracheal tube (Fig. 1). Failed attempts occurred when the progression of ETI steps varied from this pattern. This again points to the importance of rapidly and accurately identifying the best view of the glottic opening for increasing the chance for ETI success.
There are several challenging aspects to ETI, including not only obtaining an adequate view of the vocal cords, but also successfully passing the endotracheal tube after a view is obtained. In our study, the numbers of forward movements with the endotracheal tube were not different between successful and unsuccessful ETI attempts. There are likely other subtleties that allow for successful passage of the endotracheal tube that we were unable to illicit through this video review and will require further study.
Finally, recognized esophageal intubation did occur in both successful and unsuccessful ETI attempts but occurred more commonly in the unsuccessful ETI attempts. This higher rate likely occurred because the poor view in these unsuccessful attempts. In all cases, the esophageal intubation was recognized by the provider and removed prior to removing the laryngoscope from the mouth, indicating the heightened awareness and technical skill of this group of providers.
Limitations and Future Research
This study has several limitations. The videos had been de-identified of any patient information prior to evaluation, which does not allow for analysis of patient-related factors such as height, weight, or survival. Future studies should prospectively collect patient, location, and provider information for a better understanding of the intubation parameters during ETI and reduce the amount of missing data (such as the 23 cases that had been de-identified of the provider performing the intubation in our study).
Some of these metrics have been shown to have poor interrater reliability (C-L view) and others have not been externally validated.15–17 Although the interrater reliability between our two reviews was excellent for many variables, these metrics need further validation to ensure they can be reproduced.
The number of failed attempts was small. This eliminated our ability to perform multivariate analyses. Larger sample sizes will be required for multivariate analyses to evaluate independent associations of these new metrics with ETI success.
Conclusion
Video laryngoscopy provides textured detail of ETI and has potential to help providers improve proficiency with this challenging skill and may have future applications in ETI QI. Successful ETI attempts have significantly shorter entry-to-POGO times and entry-to-tube times, obtain better views of the glottic opening (POGO and C-L view), and have a lower incidence of temporary, recognized esophageal intubation.
Acknowledgments
The authors would like to thank Mr. Matthew Weaver for his assistance with the graphics for this study.
Footnotes
This paper was presented at American Heart Association Resuscitation Science Symposium, Orlando, FL, November 2011 as well as National Association of Emergency Medical Service Physicians Annual meeting, Tucson, AZ, January 2012.
The authors have no financial interests to disclose. The C-MAC Video Laryngoscopes were loaned from the Karl Storz Corp. (El Segundo, CA). The Karl Storz Corp. had no input in the study design, data collection, data analysis, writing of the manuscript, or decision to publish the data. The providers were trained in the use of the C-MAC video laryngoscope by their local medical director.
References
- 1.Pepe PE, Copass MK, Joyce TH. Prehospital endotracheal entubation: rationale for training emergency medical personnel. Ann Emerg Med. 1985;14:1085–1092. doi: 10.1016/s0196-0644(85)80927-6. [DOI] [PubMed] [Google Scholar]
- 2.Steward RD, Paris PM, Winter PM, Pelton GH, Cannon GM. Field endotracheal intubation by paramedical personnel. Success rates and complications. Chest. 1984;85:3421–3425. doi: 10.1378/chest.85.3.341. [DOI] [PubMed] [Google Scholar]
- 3.Davis DP, Hoyt DB, Ochs M, et al. The effect of paramedic rapid sequence intubation on outcome in patients with sever traumatic brain injury. J Trauma. 2003;54:444–453. doi: 10.1097/01.TA.0000053396.02126.CD. [DOI] [PubMed] [Google Scholar]
- 4.Wang HE, Seitz SR, Hostler D, Yealy DM. Defining the “learning curve” for paramedic student endotracheal intubation. Prehosp Emerg Care. 2005;9:156–162. doi: 10.1080/10903120590924645. [DOI] [PubMed] [Google Scholar]
- 5.Wang HE, Yealy DM. How many attempts are required to accomplish out-of-hospital endotracheal intubation. Acad Emerg Med. 2006;13:372–377. doi: 10.1197/j.aem.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 6.Hubble MW, Brown L, Wilfong DA, Hertelendy A, Benner RW, Richards ME. A meta-analysis of prehospital airway control techniques part I: orotracheal and nasotracheal intubation success rates. Prehosp Emerg Care. 2010;14:337–362. doi: 10.3109/10903121003790173. [DOI] [PubMed] [Google Scholar]
- 7.Wang HE, Mann NC, Mears G, Jacobson K, Yealy DM. Out-of-hospital airway management in the United States. Resuscitation. 2011;82:378–385. doi: 10.1016/j.resuscitation.2010.12.014. [DOI] [PubMed] [Google Scholar]
- 8.Mort TC. Emergency tracheal intubation: complications associated with repeated laryngoscopic attempts. Anesth Analg. 2004;99:607–613. doi: 10.1213/01.ANE.0000122825.04923.15. [DOI] [PubMed] [Google Scholar]
- 9.Benumof JL, Dagg R, Benumof R. Critical hemoglobin desaturation will occur before return to an unparalyzed state following 1mg/kg intravenous succinylcholine. Anesthesiology. 1997;87:979–982. doi: 10.1097/00000542-199710000-00034. [DOI] [PubMed] [Google Scholar]
- 10.Davis DP, Hwang JQ, Dunford JV. Rate of decline in oxygen saturation at various pulse oximetry values with prehospital rapid sequence intubation. Prehosp Emerg Care. 2008;12:46–51. doi: 10.1080/10903120701710470. [DOI] [PubMed] [Google Scholar]
- 11.Ochroch EA, Hollander JE, Kush S, Shofer FS, Levitan RM. Assessment of laryngeal view: percentage of glottic opening score vs. Cormack and Lehane grading. Can J Anesthesiol. 1999;47:447–448. doi: 10.1007/BF03013137. [DOI] [PubMed] [Google Scholar]
- 12.Levitan RM, Ochroch EA, Kush S, Shofer FS, Hollander JE. Assessment of airway visualization: validation of the percentage of glottic opening (POGO) Scale. Acad Emerg Med. 1998;5:919–923. doi: 10.1111/j.1553-2712.1998.tb02823.x. [DOI] [PubMed] [Google Scholar]
- 13.Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia. 1984;39:1105–1111. [PubMed] [Google Scholar]
- 14.Wayne MA, McDonnell M. Comparison of traditional versus video laryngoscopy in out-of-hospital tracheal intubation. Prehosp Emerg Care. 2010;14:278–282. doi: 10.3109/10903120903537189. [DOI] [PubMed] [Google Scholar]
- 15.Krange R, van Rijn C, van Groeningen D, Loer SA, Schwarte LA, Schober P. Cormack-Lehane classification revisited. Br J Anaesth. 2010;105:220–225. doi: 10.1093/bja/aeq136. [DOI] [PubMed] [Google Scholar]
- 16.Wang HE, Simeone SJ, Weaver MD, Callaway CW. Interruptions in cardiopulmonary resuscitation from paramedic endotracheal intubation. Ann Emerg Med. 2009;54:645–562. doi: 10.1016/j.annemergmed.2009.05.024. [DOI] [PubMed] [Google Scholar]
- 17.Neumar RW, Otto CW, Link MS, et al. Part 8: Adult Advanced Cardiovascular Life Support. Circulation. 2010;122(suppl):S729–S767. doi: 10.1161/CIRCULATIONAHA.110.970988. [DOI] [PubMed] [Google Scholar]