Abstract
Insulin-like growth factor binding protein 3 (IGFBP-3) plays an important role in the development and progress of cancers. The association between IGFBP-3 polymorphisms and colorectal cancer remains controversial and ambiguous. The aim of this study is to explore the association between IGFBP3 A-202C and Gly32Ala polymorphisms and colorectal cancer susceptibility using meta-analyisi. Case-control studies on the association between IGFBP3 A-202C and Gly32Ala polymorphisms and colorectal cancer, which had sufficient data for estimating an odds ratio (OR) with 95% confidence interval (CI), were included in the meta-analysis. Abstracts, case reports, editorials, and review articles were excluded. Heterozygous and homozygous mutants were compared with the wild types to estimate combined OR values and 95%CIs with Review Manager 5.0. Six eligible studies were included, with 3157 patients and 6027 controls for A-202C and 1711 patients and 2995 controls for Gly32Ala. No significant association was found in all genetic models (for A-202C, AC vs. AA, OR = 0.99(0.88–1.11), CC vs. AA, OR = 1.06(0.92–1.22), dominant model, OR = 0.98(0.88–1.09), recessive model, OR = 0.94(0.84–1.05); and for Gly32Ala polymorphism, GC vs. GG, OR = 1.10(0.92–1.31), CC vs. GG, OR = 0.93(0.76–1.14), dominant model, OR = 1.05(0.89–1.24), recessive model, OR = 0.90(0.77–1.05)). The results suggest that the IGFBP3 A-202C and Gly32Ala polymorphisms are not associated with colorectal cancer susceptibility.
Introduction
Colorectal cancer is the third most common diagnosed cancer in males and the second in females, with over 1.2 million new cancer cases and 608,700 deaths worldwide in 2008 [1], [2]. Genetic susceptibility to this disease may result from inherited mutations in genes involved in proliferation and apoptosis.
The insulin-like growth factor (IGF) family, including insulin-like growth factor 1 (IGF1), insulin-like growth factor 2 (IGF2)and insulin-like growth factor binding protein (IGFBP), are involved in proliferation and apoptosis, and thus play a significant role in both normal and malignant cell growth [3]. In the circulation, about 90% of IGF1 is bound to IGFBP3, which regulates the distribution and bioavailability of IGF1 [4]. In addition, IGFBP3 exerts anti-proliferative and apoptotic effects that are mediated through a specific cell surface receptor [5]. Epidemiological studies show that high levels of IGF1 and low levels of IGFBP3 are associated with an increased risk for several common cancers, including cancer of the prostate, breast, lung, and colorectum [6]–[8]. Although many personal and lifestyle factors, including body mass index (BMI), vigorous physical activity and smoking, may affect the circulating levels of IGFBP3 [9], a twin study demonstrated that heritable factors may account for 60% of the inter-individual variation in IGFBP3 levels [10].
Two genetic polymorphisms have been identified as influencing the circulating levels of IGFBP3. One is a promoter single nucleotide polymorphism (SNP) located at position -202 (rs2854744, A>C) a transcription start site that is believed to affect the promoter activity [11]. The other polymorphism is a non-synonymous substitution, Gly32Ala (rs2854746, G>C), a site for high affinity binding of IGF1 [12]. The presence of the variant 32Ala allele was inversely associated with IGFBP3 levels [13].
Until 2009, there were several studies evaluating associations between the IGFBP3 polymorphisms and cancer risk in diverse populations and in multiple types of cancer, but their outcomes have been contradictory. Li et al’s meta-analysis showed significant association was found in additive genetic model between IGFBP3 A-202C SNP and breast cancer and prostate cancer [14], Chen et al’s meta-analysis suggest IGFBP3 202CC genotype was associated with an increased risk of prostate cancer with borderline significance [15]. However, it is hard to explore the association between IGFBP3 SNPs and colorectal cancer because there are only 3 papers to investigate this issue before 2009, another two articles(Xiang et al [16] and Feik at al [17]) exploring this issue were published in 2009 and 2010, however, these results are contrary than conclusive, so we think it is meaningful to estimate the effect of genotypes of IGFBP3 on risk for colorectal cancer.
Materials and Methods
Identification and Eligibility of Studies
To identify all articles that explored the association of IGFBP3 A-202C and Gly32Ala polymorphisms with colorectal cancer, we conducted a literature search of the PubMed database (last search on December 31st, 2011) using the following search terms: ‘IGFBP3’ or ‘Insulin growth factor binding protein 3′, ‘polymorphism’, and ‘colorectal cancer’. The search followed the guidelines of the 2009 preferred reporting items for systematic reviews and meta-analysis (PRISMA) statement (Table S1). All eligible articles were retrieved and their references were checked for other relevant articles. Abstracts, case reports, editorials, and review articles were excluded. All the studies included had to meet all the following criteria: (1) case-control design; (2) outcome of colorectal cancer; (3) sufficient data for estimating an odds ratio (OR) with 95% confidence interval (CI).
Data Extraction
Data were carefully extracted from all eligible publications independently by two investigators (Hao X and Ying W). For conflicting evaluation, an agreement was reached following discussion. For each study, the following characteristics were collected: first author, year of publication, control groups studied, ethnicity, genotypes and allele frequency of cases and controls.
Statistical Analysis
The meta-analysis examined the overall association of allele C of A-202C site and the risk for colorectal cancer, including the comparisons of co-dominant (CC vs. AA, CA vs. AA), recessive (CC vs. AC+AA) and dominant (CC+AC vs. AA) models. The same comparisons were performed for Gly32Ala allele C to G. The summary odds ratios (OR) and 95% confidence intervals (CIs) were used to assess the strength of association. DerSimonian and Laird Q test was used to assess the degree of heterogeneity between studies and the heterogeneity was considered significant when P<0.05 [18], [19]. Fixed-effect model, based on the Mantel–Haenszel method, was used when no significant heterogeneity among the studies was found (P>0.05). Otherwise, a random-effect model was chosen.
Publication bias was investigated by funnel plot, in which the standard error of log (OR) of each study was plotted against its OR. Funnel plot asymmetry was assessed by Egger’s test, a linear regression approach to measure asymmetry on the natural logarithm scale of the OR [20]. The departure from the Hardy-Weinberg equilibrium for the control group in each study was assessed with Pearson's goodness-of-fit chi-square test with 1 degree of freedom.
All data were analyzed using Statistical Analysis System software (v.9.1.3; SAS Institute, Cary, NC, USA), STATA7.0 (Stata-Corp, College Station, TX, USA) and Review Manager (v.5.0, Oxford, England). All p-values were based on two-sided tests and a p-value of less than 0.05 was considered statistically significant.
Results
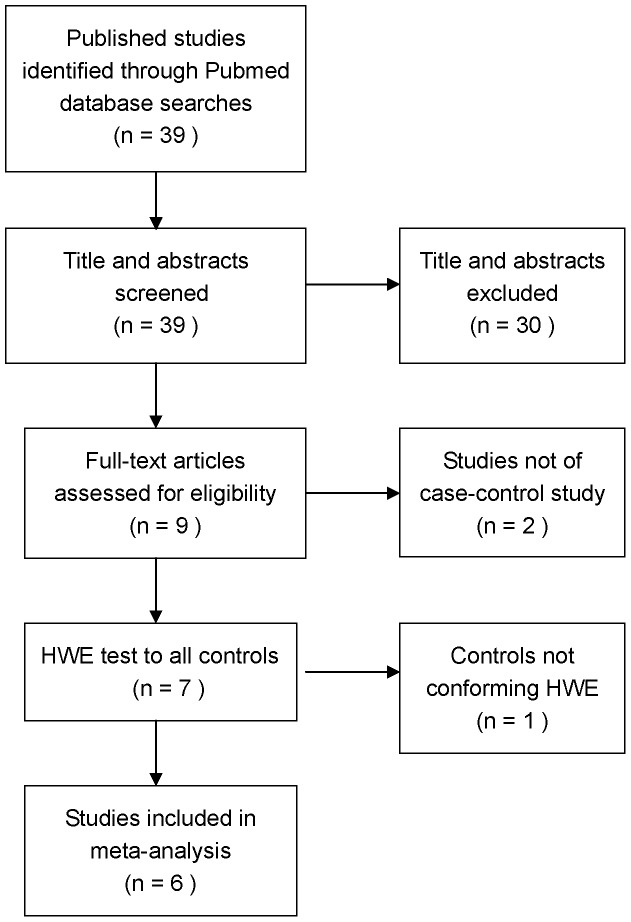
From 39 publications identified by initial data searches, nine studies examining the association of IGFBP3 -A202C and Gly32Ala polymorphisms with colorectal cancer were identified (Figure 1). Two articles were excluded because they were not case control studies. In one study [21], the distribution of genotypes in controls was not consistent with Hardy-Weinberg equilibrium, so it was also excluded. Six published studies were eligible for further analysis, including 4 population-based and 2 hospital-based case control studies. As shown in Table 1, 5 of the studies [13], [16], [22]–[24] evaluated the relationship between IGFBP3 -A202C polymorphisms and colorectal cancer and included 3157 cases and 6027 controls. Meanwhile, 4 studies [13], [16], [17], [23] evaluated the relationship between IGFBP3 Gly32Ala polymorphisms and colorectal cancer and included 1711 cases and 2995 controls.
Figure 1. The process of identifying relevant studies is summarized.
Table 1. Distribution of genotypes and alleles of IGFBP3 A-202C and Gly32Ala polymorphisms among cases and controls.
| SNP | Author(year) | Typea | Ethnicityb | Case | Control | ||||||||
| AA (%) | AC (%) | CC (%) | A (%) | C (%) | AA (%) | AC (%) | CC (%) | A (%) | C (%) | ||||
| A-202C | Slattery(2004) | PB | C | 427(21.9) | 997(51.2) | 524(26.9) | 1851(47.6) | 2045(52.5) | 463(21.5) | 1082(50.3) | 607(28.2) | 2008(46.7) | 2296(53.3) |
| Wong(2005) | PB | A | 166(61.0) | 90(33.1) | 16(5.9) | 422(77.6) | 122(22.4) | 480(58.5) | 306(37.3) | 35(4.3) | 1266(77.1) | 376(22.9) | |
| Pechlivanis(2007) | PB | C | 135(22.0) | 314(51.1) | 165(26.9) | 584(47.6) | 644(52.4) | 122(22.3) | 262(47.9) | 163(29.8) | 506(46.3) | 588(53.7) | |
| Xiang(2009) | HB | A | 121(59.9) | 69(34.2) | 12(5.9) | 311(77.0) | 93(23.0) | 134(63.2) | 68(32.1) | 10(4.7) | 336(79.2) | 88(20.8) | |
| Feik(2010) | HB | C | 37(19.8) | 59(35.5) | 32(34.7) | 133(42.6) | 109(57.4) | 504(29.1) | 845(48.8) | 381(22.0) | 1853(53.6) | 1607(46.4) | |
| GG (%) | GC (%) | CC (%) | G (%) | C (%) | GG (%) | GC (%) | CC (%) | G (%) | C (%) | ||||
| Gly32Ala | Morimoto(2005) | PB | C | 173(22.1) | 361(46.2) | 248(31.7) | 707(45.2) | 857(54.8) | 95(18.9) | 226(44.9) | 182(36.2) | 416(41.4) | 590(58.6) |
| Pechlivanis(2007) | PB | C | 111(18.3) | 317(52.3) | 178(29.4) | 539(44.5) | 673(55.5) | 114(20.7) | 259(47.1) | 177(32.2) | 487(44.3) | 613(55.7) | |
| Xiang(2009) | HB | A | 101(50.0) | 84(41.6) | 17(8.4) | 286(70.8) | 118(29.2) | 129(60.8) | 72(34.0) | 11(5.2) | 330(77.8) | 94(22.2) | |
| Feik(2010) | HB | C | 24(19.8) | 55(45.5) | 42(34.7) | 103(42.6) | 139(57.4) | 320(18.5) | 822(47.5) | 588(34.0) | 1462(42.3) | 1998(57.7) | |
Type of control source: ‘PB’ for population based, ‘HB’ for hospital based.
Ethnicity: ‘C’ for Caucasian ancestry, ‘A’ for Asian ancestry.
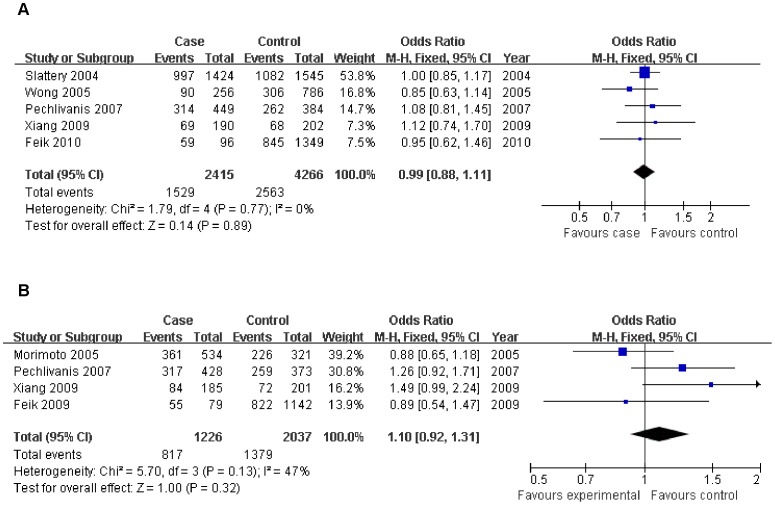
For IGFBP3 -A202C, there is no significant association with colorectal cancer risk when all studies are pooled into a meta-analysis (CA vs. AA: OR = 0.99, 95% CI = 0.88–1.11; CC vs. AA: OR = 1.06, 95% CI = 0.92–1.22; dominant model: OR = 0.98, 95% CI = 0.88–1.09; recessive model: OR = 0.94, 95% CI = 0.84–1.05) (Table 2). For the additive model, individuals carrying the C allele were not at increased risk for colorectal cancer (OR = 0.97, 95% CI = 0.91–1.04) (Figure 2A). There is no significantly elevated colorectal cancer risk in any genetic model when all studies are pooled into the analysis (CG vs. GG: OR = 1.10, 95% CI = 0.96–1.25; CC vs. GG: OR = 1.06, 95% CI = 0.82–1.37; dominant model: OR = 1.06, 95% CI = 0.88–1.27; recessive model: OR = 0.89, 95% CI = 0.80–1.01).
Table 2. Results of meta-analysis for IGFBP3 A-202C/Gly32Ala polymorphism and colorectal cancer.
| Genotype Comparisons | OR (95% C.I.) | P | Ph | I2 |
| A-202C | ||||
| AC vs. AA | 0.99(0.88–1.11) | 0.89 | 0.77 | 0% |
| CC vs. AA | 1.06(0.92–1.22) | 0.40 | 0.62 | 0% |
| CC+AC vs. AA | 0.98(0.88–1.09) | 0.71 | 0.89 | 0% |
| CC Vs. AC+AA | 0.94(0.84–1.05) | 0.28 | 0.63 | 0% |
| Gly32Ala | ||||
| GC vs. GG | 1.10(0.92–1.31) | 0.32 | 0.13 | 47% |
| CC vs. GG | 0.93(0.76–1.14) | 0.49 | 0.13 | 46% |
| CC+GC vs. GG | 1.07(0.81–1.42) | 0.62 | 0.05 | 61% |
| CC Vs. GC+GG | 0.90(0.77–1.05) | 0.17 | 0.31 | 16% |
Ph P value of Q test for heterogeneity.
Figure 2. Association of IGFBP3 A-202C and Gly32Ala polymorphisms with colorectal cancer risk.
Each comparison was presented by the year of publication. Part A analyzed the comparison between IGFBP3 A-202C(AC vs. AA) and colorectal cancer, par B analyzed the comparison between Gly32Ala polymorphism (GC vs. GG) and colorectal cancer.
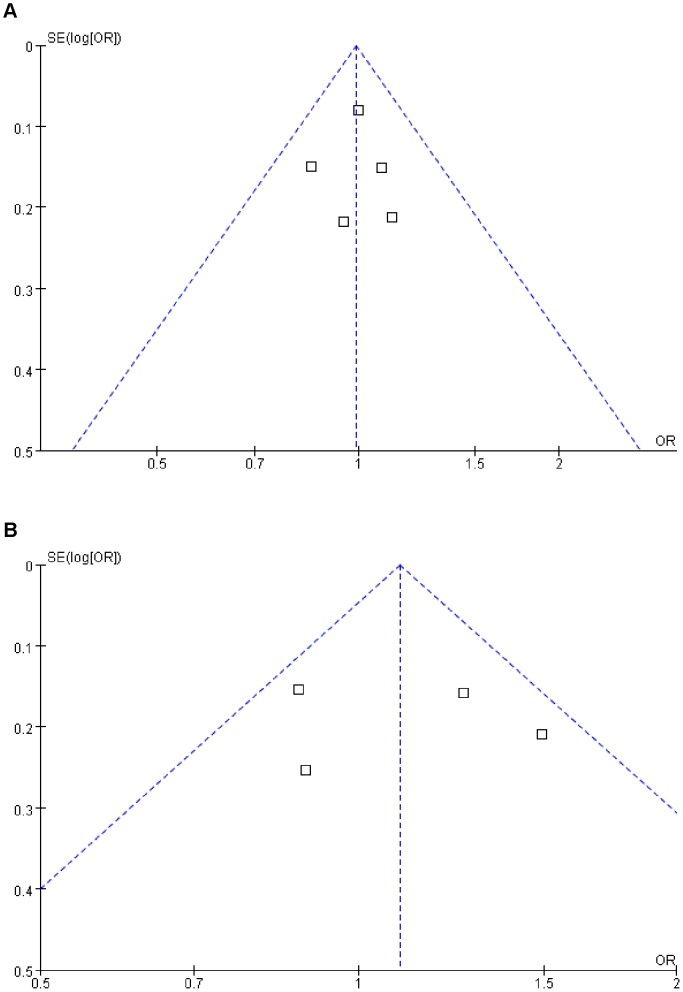
Sensitivity analysis was performed by sequential omission of individual studies for each comparison in multiple models. The results did not change the overall effects of the two SNPs on cancer risk under different genetic models, indicating that the significance of pooled ORs was not excessively influenced by any single study. The Funnel plot’s shapes of all comparisons did not reveal obvious evidence of asymmetry, and the results of Egger’s test also suggested that there was no evidence of publication bias. For example, as shown in Figure 3, the shape of the funnel plots does not reveal any evidence of obvious asymmetry, and results of Egger’s test did not suggest any evidence of publication bias (t = 1.45, P = 0.28 for A-202C, t = 0.76, P = 0.35 for Gly32Ala).
Figure 3. Funnel plots of IGFBP3 A-202C and Gly32Ala polymorphism and colorectal cancer risk.
Part A, model: A-202C (AC Vs AA), t eager’s test = 1.45, P eager’s test = 0.28. Part B, model: Gly32Ala (GC Vs GG), t eager’s test = 0.76, P eager’s test = 0.35.
Discussion
In this study, we employed a meta-analysis to provide the assessment of the association between IGFBP3 A-202C and Gly32Ala polymorphisms and colorectal cancer risk by critically reviewing 5 studies of the A-202C polymorphism (a total of 3157 cases and 6027 controls) and 4 studies of the Gly32Ala polymorphism (a total of 1711 cases and 2995 controls). Heterogeneity analysis and sensitivity analysis were also critically performed to ensure the reliability of this meta-analysis. This meta-analysis indicated that these two polymorphisms in IGFBP3 are not significantly associated with risk for colorectal cancer.
Because IGFBP3 has an important role in tumor development, polymorphisms located in IGFBP3 might be potential markers in the evaluation of exposure of target organs to endogenous IGFBP3 on cancer risk. One of the potential mechanisms may be that the variant (G to C substitution) of Gly32Ala causes an amino acid change from alanine to glycine of codon 32, reducing percent binding of IGFBP3 and leading to lower concentration of IGFBP3 in the circulation. Of the 4 articles included in this meta-analysis, only one study shows that participants carrying the Gly32Ala GC heterozygote or CC homozygote have a significantly increased risk of colorectal cancer development [16], however, the sample size of this study is so small(only 202 cases and 212 controls) that there is very limited impact on the overall result from the meta-analysis. In addition, IGFBP functions normally as an inhibitor of IGF’s action by blocking the binding of IGF to its receptor, but it can enhance the IGF’s action by protecting IGF from degradation under certain circumstance [25]. This may be another reason to explain the inconsistent findings among studies.
Previous studies revealed that IGFBP3 A-202C polymorphism was associated with circulating IGFBP3 concentration, and the potential mechanism is that the C allele of the A-202C variant decreased promoter activity, affecting IGFBP3 transcription. A few meta-analysis studies also showed that this variant is associated with increased breast and prostate cancer risk [14], [15]. Our result is inconsistent with these two meta-analysis studies. We may not have detected an association between IGFBP3 A-202C polymorphism and colorectal cancer for several reasons. First, the current knowledge of colorectal carcinogenesis indicates a multi-factorial and multi-step process that involves various genetic alterations and environmental factors. Some environmental factors, however, may predominate in the development of cancer, such as living habits and exposure to carcinogens. Without considering these factors, it may lead to the failure to detect the role of this polymorphism in cancer development. Second, the IGF axis includes the polypeptide ligands IGF1 and IGF2, the IGF receptors, and six binding IGF proteins (IGFBP1-IGFBP6), there are relation between many members, some single-nucleotide polymorphisms of familiar members, such as polymorphisms of, IGFBP2 and IGFBP3, may exert their complex and interacting functions with each other, which could affect the effects of A-202C polymorphism in the pathogenesis of cancer. Therefore, other polymorphisms as cancer risk factors should be taken into account to conclude a true effect. Third, the number of current case control studies is relatively small (only including five studies), we may have insufficient statistical power to generate an real risk estimation.
A few studies have confirmed that IGFBP-3 levels are influenced by the -A202C IGFBP3 polymorphism [11], [26], and this polymorphism could influence responsiveness to growth inhibitors whose action involves up-regulation of IGFBP3 and the efficacy of various agents proposed for cancer chemoprevention [11]. A difficult issue for clinicians is determing which subpopulations are more sensitive to chemoprevention. If large sample studies could explore the association between IGFBP3 polymorphisms and colorectal cancer, IGFBP3 may provide an example of a gene whose polymorphic variation is relevant to the pharmacogenomics of cancer prevention.
Assessment of heterogeneity is necessary for most meta-analyses. Heterogeneity could result from genotyping error, population stratification, selection bias, gene-environment interaction, or chance. There is no significant heterogeneity in IGFBP3 A-202C and Gly32Ala genotype comparisons (see Table 2), and meta-analysis results showed that there were no significant effect between IGFBP3 A-202C, Gly32Ala polymorphisms and colorectal cancer. We concluded that subgroup analysis is not necessary in the present study.
Although we have put considerable effort and resources into testing the possible association between IGFBP3 polymorphisms and colorectal cancer risk, there are still some limitations inherited from the published studies. First, some non-differential misclassification bias is possible. One hospital based case control study selected hospital patients without colorectal cancer as the reference group. Therefore, non-differential misclassification bias is possible because the study may have included the control group who has different risk of developing colorectal cancer. Second, we can not perform subgroup analysis for specific cancer sites because of limited information from original studies; for example, patients in only one article were divided by colon and rectum [22].
In conclusion, this meta-analysis suggests that IGFBP3 A-202C and Gly32Ala polymorphisms may not be associated with colorectal cancer development. However, it is necessary to conduct large sample studies using standardized unbiased genotyping methods and well matched controls. Such studies taking these factors into account may eventually lead to a better, comprehensive understanding of the association between the polymorphisms in the GH-IGF pathway and colorectal cancer risk.
Supporting Information
PRISMA checklist. This table described reported page number of each necessary section of Meta-analysis according to PRISMA Statement.
(DOC)
Acknowledgments
We thank Dr. Kristen J. Mertz of Department of epidemiology, Graduate School of Public Health, University of Pittsburgh for her thoughtful comments and scientific editing. We also thank Dr. Zhijiang Zhang of Department of Epidemiology and Biostatistics, School of Public Health, Wuhan University for his invaluable suggestions.
Funding Statement
The authors have no support or funding to report.
References
- 1. Center MM, Jemal A, Ward E (2009) International trends in colorectal cancer incidence rates. Cancer Epidemiol Biomarkers Prev 18: 1688–1694. [DOI] [PubMed] [Google Scholar]
- 2. Jemal A, Bray F (2011) Center MM, Ferlay J, Ward E, et al (2011) Global cancer statistics. CA Cancer J Clin 61: 69–90. [DOI] [PubMed] [Google Scholar]
- 3. Bustin SA, Jenkins PJ (2001) The growth hormone-insulin-like growth factor-I axis and colorectal cancer. Trends Mol Med 7: 447–454. [DOI] [PubMed] [Google Scholar]
- 4. Khandwala HM, McCutcheon IE, Flyvbjerg A, Friend KE (2000) The effects of insulin-like growth factors on tumorigenesis and neoplastic growth. Endocr Rev 21: 215–244. [DOI] [PubMed] [Google Scholar]
- 5. Firth SM, Baxter RC (2002) Cellular actions of the insulin-like growth factor binding proteins. Endocr Rev 23: 824–854. [DOI] [PubMed] [Google Scholar]
- 6. Yu H, Rohan T (2000) Role of the insulin-like growth factor family in cancer development and progression. J Natl Cancer Inst 92: 1472–1489. [DOI] [PubMed] [Google Scholar]
- 7. Gallagher EJ, LeRoith D (2010) The proliferating role of insulin and insulin-like growth factors in cancer. Trends Endocrinol Metab 21: 610–618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Renehan AG, Zwahlen M, Minder C, O’Dwyer ST, Shalet SM, et al. (2004) Insulin-like growth factor (IGF)-I, IGF binding protein-3, and cancer risk: systematic review and meta-regression analysis. The Lancet 363: 1346–1353. [DOI] [PubMed] [Google Scholar]
- 9. Giovannucci E, Pollak MN, Platz EA, Willett WC, Stampfer MJ, et al. (2000) A prospective study of plasma insulin-like growth factor-1 and binding protein-3 and risk of colorectal neoplasia in women. Cancer Epidemiol Biomarkers Prev 9: 345–349. [PubMed] [Google Scholar]
- 10. Harrela M, Koistinen H, Kaprio J, Lehtovirta M, Tuomilehto J, et al. (1996) Genetic and environmental components of interindividual variation in circulating levels of IGF-I, IGF-II, IGFBP-1, and IGFBP-3. J Clin Invest 98: 2612–2615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Deal C, Ma J, Wilkin F, Paquette J, Rozen F, et al. (2001) Novel promoter polymorphism in insulin-like growth factor-binding protein-3: correlation with serum levels and interaction with known regulators. J Clin Endocrinol Metab 86: 1274–1280. [DOI] [PubMed] [Google Scholar]
- 12. Vorwerk P, Yamanaka Y, Spagnoli A, Oh Y, Rosenfeld RG (1998) Insulin and IGF binding by IGFBP-3 fragments derived from proteolysis, baculovirus expression and normal human urine. J Clin Endocrinol Metab 83: 1392–1395. [DOI] [PubMed] [Google Scholar]
- 13. Morimoto LM, Newcomb PA, White E, Bigler J, Potter JD (2005) Insulin-like growth factor polymorphisms and colorectal cancer risk. Cancer Epidemiol Biomarkers Prev 14: 1204–1211. [DOI] [PubMed] [Google Scholar]
- 14. Li L, Huang X, Huo K (2009) IGFBP3 polymorphisms and risk of cancer: a meta-analysis. Molecular Biology Reports 37: 127–140. [DOI] [PubMed] [Google Scholar]
- 15. Chen W, Wang S, Tian T, Bai J, Hu Z, et al. (2009) Phenotypes and genotypes of insulin-like growth factor 1, IGF-binding protein-3 and cancer risk: evidence from 96 studies. European Journal of Human Genetics 17: 1668–1675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Xiang H, Liu L, Chu G-d, Wei S, Liu J-p, et al. (2009) Association Between Two Functional Polymorphisms of Insulin-Like Growth Factor Binding Protein 3 and Colorectal Cancer Risk in a Chinese Population. Journal of Toxicology and Environmental Health, Part A 72: 706–711. [DOI] [PubMed] [Google Scholar]
- 17. Feik E, Baierl A, Hieger B, Führlinger G, Pentz A, et al. (2009) Association of IGF1 and IGFBP3 polymorphisms with colorectal polyps and colorectal cancer risk. Cancer Causes & Control 21: 91–97. [DOI] [PubMed] [Google Scholar]
- 18. Deeks JJ (2001) Systematic reviews in health care: Systematic reviews of evaluations of diagnostic and screening tests. BMJ 323: 157–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Little J, Ashktorab H, Nguza B, Fatemi M, Nouraie M, et al. (2011) Case-Control Study of Vitamin D, dickkopf homolog 1 (DKK1) Gene Methylation, VDR Gene Polymorphism and the Risk of Colon Adenoma in African Americans. PLoS ONE 6: e25314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315: 629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Le Marchand L (2005) Association of an Exon 1 Polymorphism in the IGFBP3 Gene with Circulating IGFBP-3 Levels and Colorectal Cancer Risk: The Multiethnic Cohort Study. Cancer Epidemiology Biomarkers & Prevention 14: 1319–1321. [DOI] [PubMed] [Google Scholar]
- 22. Slattery ML, Samowitz W, Curtin K, Ma KN, Hoffman M, et al. (2004) Associations among IRS1, IRS2, IGF1, and IGFBP3 genetic polymorphisms and colorectal cancer. Cancer Epidemiol Biomarkers Prev 13: 1206–1214. [PubMed] [Google Scholar]
- 23. Pechlivanis S, Wagner K, Changclaude J, Hoffmeister M, Brenner H, et al. (2007) Polymorphisms in the insulin like growth factor 1 and IGF binding protein 3 genes and risk of colorectal cancer. Cancer Detection and Prevention 31: 408–416. [DOI] [PubMed] [Google Scholar]
- 24. Wong HL, Koh WP, Probst-Hensch NM, Van den Berg D, Yu MC, et al. (2008) Insulin-like growth factor-1 promoter polymorphisms and colorectal cancer: a functional genomics approach. Gut 57: 1090–1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Chen JC, Shao ZM, Sheikh MS, Hussain A, LeRoith D, et al. (1994) Insulin-like growth factor-binding protein enhancement of insulin-like growth factor-I (IGF-I)-mediated DNA synthesis and IGF-I binding in a human breast carcinoma cell line. J Cell Physiol 158: 69–78. [DOI] [PubMed] [Google Scholar]
- 26. Jernstrom H, Deal C, Wilkin F, Chu W, Tao Y, et al. (2001) Genetic and nongenetic factors associated with variation of plasma levels of insulin-like growth factor-I and insulin-like growth factor-binding protein-3 in healthy premenopausal women. Cancer Epidemiol Biomarkers Prev 10: 377–384. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PRISMA checklist. This table described reported page number of each necessary section of Meta-analysis according to PRISMA Statement.
(DOC)