Abstract
We report a case of a large intra-aortic thrombosis in an 83-year-old woman concurrent with metastatic mediastinal leiomyosarcoma. Imaging studies incidentally detected a mediastinal malignant tumour metastasising to bilateral adrenals and an extensive intra-aortic mass that was suspected to be intra-aortic thrombosis. One month later massive embolism developed in the lower limb and her condition deteriorated rapidly resulting in death. Autopsy revealed diffused proliferation of highly pleomorphic atypical cells accompanied by necrosis in the mediastinum tumours and bilateral adrenal glands. Leiomyosarcoma metastasising to bilateral adrenals was confirmed by the results of immunostaining. The intra-aortic mass suggested that the fragmented thrombus might be the cause of a sudden lower-limb embolism. Microscopic examination showed that the mass lesion in the aortic arch was composed of a blood clot containing neutrophils. We report this case because leiomyosarcoma arising from the mediastinum and, especially, associated with an extraordinarily large intra-aortic thrombosis is very rare.
Background
Leiomyosarcoma is a malignant tumour of smooth muscle affecting young to elderly adults. It is a confined and encapsulated mass that may originate from various organs such as the uterus, digestive tracts, lungs, large blood vessels (including large vein, antebrachial vein and saphenous vein), retroperitoneum, mesenterium or soft parts of the extremities (from vascular wall). The tumour consists of palisade or tangled atypical spindle cells, associated with necrotic haemorrhage. Leiomyosarcoma arising from the mediastinum is very rare. Especially, mesenchymal tumours (including both benign and malignant tumours) account for only less than 2% of all the mediastinal tumours (Armed Forces Institute of Pathology (AFIP) tumours of the mediastinum, 2010). In Japan, only 15 cases have been reported till 2005.
On the other hand, intra-aortic thrombosis was reported in 1967 by Oliver et al1 and diagnosis is often made during investigation for thromboembolism. Thrombus in the non-aneurysmatic, non-atherosclerotic descending thoracic aorta (NAADTA) is also very rare and Tsilimparis et al2 identified eight cases of NAADTA over a period of 13 years. Seven cases were diagnosed by detailed investigations after embolism and the remaining cases were found incidentally.
Case presentation
An 83-year-old woman visited our hospital with a situational hypertension on 19 October 2010. Abdominal ultrasonography performed to exclude secondary hypertension showed bilateral adrenal gland swelling. Abdominal contrast-enhanced CT was performed, which detected a bilateral adrenal gland enlargement and an intra-aortic mass lesion at the descending aorta. Following a contrast-enhanced chest CT further revealed an intra-aortic mass extending from the aortic arch to the descending aorta and intra-aortic thrombosis was highly suspected (figure 1). This CT also demonstrated a mediastinal tumour of 45×40 mm and low attenuation which was enhanced by contrast (figure 1). Contrast-enhanced MRI revealed high intensity mass at the diffusion-weighted image (figure 2A), low apparent diffusion coefficient (ADC) value which was enhanced by contrast (figure 2B). Taking into account these findings, a malignant mass metastasising to bilateral adrenals was highly suspected. Biopsy was not performed because her general condition was poor due to aging, and she was an inappropriate candidate for chemotherapy or surgery. As cortisol, rennin, aldosterone and catecholamine levels were normal, the adrenal gland tumours were likely to be non-functional.
Figure 1.
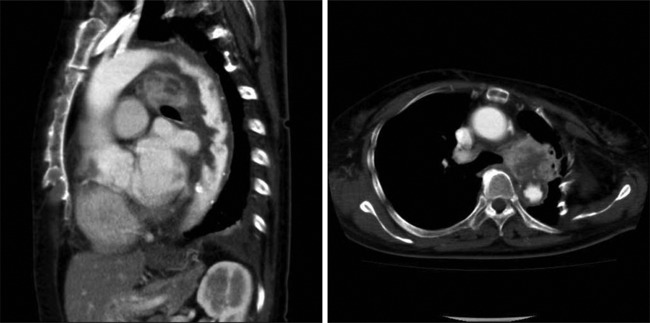
Chest contrast-enhanced CT findings: an intra-aortic mass extending from the aortic arch to descending aorta and intra-aortic thrombosis was highly suspected. A mediastinal tumour, 45×40 mm, low-attenuation mass which was enhanced by contrast was also demonstrated.
Figure 2.
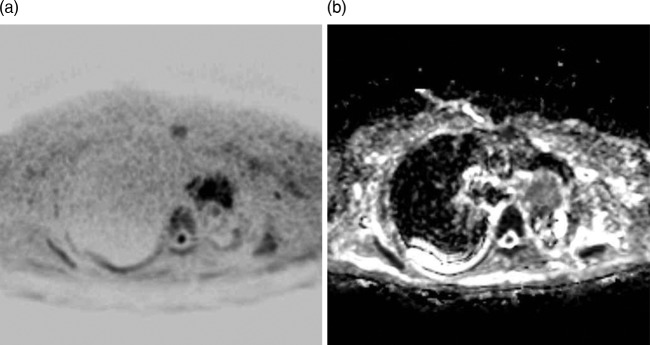
Contrast-enhanced MRI findings: (A) mediastinal tumour was a high-intensity mass at the diffusion-weighted image and (B) mediastinal tumour was low apparent diffusion coefficient value which was enhanced by contrast.
On 28 November 2010, she was urgently transported to our hospital owing to an injury from a fall when she tried to stand up from her wheelchair. Plain x-ray depicted left medial femoral neck fracture, and pathological fracture of right pubis and ischium. Pain control and rehabilitation were mainly performed, because a surgery was considered difficult. Discoloured necrosis-like findings in the left lower extremities appeared on around 6 December, and it was considered that this resulted from embolism caused by tumour or thrombus was suspected. The patient was treated with intravenous infusion of alprostadil (PGE1) and change of dressing. Subsequently, ileus, fever and increased inflammation occurred. The patient died at 3:57 on 14 December. Autopsy was performed with consent from her family.
Macroscopically, a 5×6 cm, relatively well-demarcated, nodular, whitish tumour was present in the mediastinum (figure 3). Histopathological examination of the mediastinal tumour revealed a diffuse proliferation of highly pleomorphic atypical cells with spindle to polygonal cytoplasm and bizarre and hyperchromatic nuclei (figure 4A,B). Scattered necrosis and venous invasion, and many mitoses were also noted. Leiomyosarcoma was confirmed based on the results of immunostaining: positive for smooth muscle actin (SMA), HHF-35 and vimentin; negative for myoglobin, CD34, CD56, desmin, S100 and AE1/AE3 (figure 5A,B). Histological findings were identical in the tumours of bilateral adrenals, confirming a diagnosis of mediastinal leiomyosarcoma metastasising to bilateral adrenals. No metastasis was found in other organs such as the lungs, liver and stomach. The intra-aortic mass at postmortem gross examination appeared to be smaller compared to the imaging clinical findings, which suggests that the cause of the inferior limb embolism occurred by fragmented thrombus. Microscopically, the mass lesion in the aortic arch was composed of blood clot containing neutrophils. Also, the left sternal artery was occluded by thrombus, confirming the suspicion that the aortic mass observed on antemortem CT was intra-aortic thrombosis.
Figure 3.
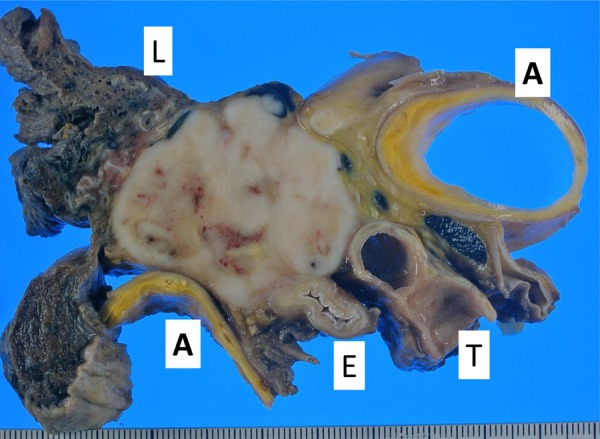
Macroscopic findings: the tumour showed a white and well-circumscribed solid lesion with focal necrotic change, and no extension into lung, trachea, oesophagus and aorta. L: lung; T: trachea; E: oesophagus; A: aorta.
Figure 4.
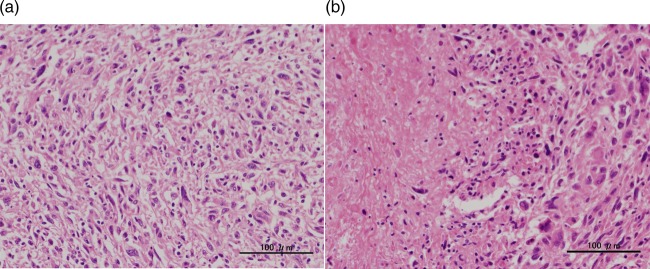
Microscopic findings: (A) the tumour was composed of highly pleomorphic and spindle cells and (B) the tumour showed necrotic changes (A, B: H&E ×200).
Figure 5.
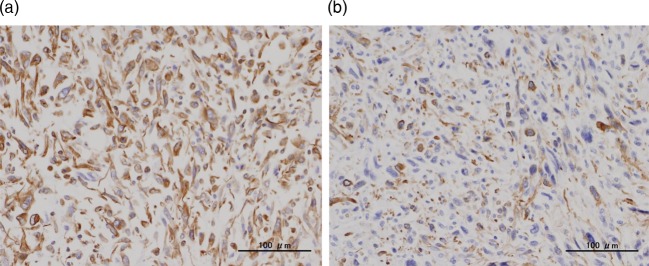
Immunohistochemical findings: the tumour cells expressed positive for vimentin and α-smooth muscle actin (SMA) (A: vimentin ×200, B: α-SMA ×200).
Outcome and follow-up
The patient died and an autopsy revealed mediastinum leiomyosarcoma metastasising only to bilateral adrenals. The intra-aortic finding suggested that fragmented thrombus might be the cause of sudden fatal lower-limb non-cancerous thromboembolism as the results of the poor basic physical status based on the leiomyosarcoma.
Discussion
We encountered a patient who presented with situational hypertension, leading to incidental detection of intra-aortic thrombosis and mediastinal leiomyosarcoma metastasising to bilateral adrenals. Leiomyosarcoma arising from the mediastinum is very rare, especially considering that mesenchymal tumours (including both benign and malignant tumours) account for only less than 2% of mediastinal tumours (AFIP tumours of the mediastinum, 2010). In Japan, only 15 cases have been reported so far. Those 15 patients consisted of 8 men and 7 women, aged 34–79 years, which suggests that this patient is the oldest. The mediastinal location of the tumours was superior in six cases, anterior in two, middle in two and posterior in five cases, and the tumours tended to metastasise to the lung. Subjective symptoms are non-specific such as cough, chest and back pain, dysponea and fever, although many cases were asymptomatic3 as was also the case in this patient. Previous study has reported that aging, many mitotic figures and tissue necrosis are the high-risk factors for the prognosis of leiomyosarcoma; especially, mitotic figure is a single predictor.4 Complete excision of the tumour is critical to improve prognosis, but the effectiveness of treatments such as chemotherapy and radiation is yet to be determined.4
In most cases, thromboembolism is the initial clinical manifestation of intra-aortic thrombosis2 though our patient had no such history as is suggestive of embolism and her intra-aortic thrombosis was diagnosed incidentally. Except that this patient was bearing cancer, laboratory tests did not show any abnormalities, as shown by protein S activity of 90%, protein C activity of 102%, negative anticardiolipin antibody test and lupus anticoagulant of 0.98. Only D-dimer increased slightly to 4.4 µg/ml. Management of NAADT has not been established, but floating thrombus is known to be a high-risk factor for embolism.5 Transthoracic echocardiography did not reveal clear floating in this case. We did not provide anticoagulant therapy after discussion with her family, because she had severe dementia and a history of bleeding owing to a fall, and the intra-aortic mass could have been intravascular invasion by malignant tumour since mediastinal tumour existed. However, she developed embolism in the lower extremities approximately 2 months after the diagnosis. Although intra-aortic thrombosis as large as our case is extremely rare, aortic mural thrombus is relatively common. In a study of 10 671 autopsy cases, mural thrombus was found in 0.9% of the cases, 50% of which were associated with aneurysm and 17% with embolism.6 Although medical treatments for this disease have yet to be established, recurrence of embolism has been reported to be prevented by anticoagulant and surgical therapies.2 Therefore, the benefits of anticoagulant therapy in patients with asymptomatic intra-aortic thrombosis should be investigated in the future.
In summary, we reported a very rare case of fatal intra-aortic thrombosis associated with a rare mediastinal leiomyosarcoma.
Learning points.
Leiomyosarcoma arising from the mediastinum is very rare, especially considering that all mesenchymal tumours account for only less than 2% of mediastinal tumours. In Japan, only 15 cases have been reported so far.
Thrombus in the non-aneurysmatic, non-atherosclerotic descending thoracic aorta is also very rare but does exist.
In most cases, thromboembolism is the initial clinical manifestation of intra-aortic thrombosis though our patient had no such history as is suggestive for embolism and her intra-aortic thrombosis was diagnosed incidentally. A physician should keep this fact in mind when he encounters a patient with thromboembolism.
Although medical treatments for intra-aortic thrombosis are yet to be established, recurrence of embolism can reportedly be prevented by anticoagulant and surgical therapies.2
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Oliver DO. Embolism from mural thrombus in the thoracic aorta. Br Med J 1967;3:655–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tsilimparis N, Hanack U, Pisimisis G, et al. Thrombus in the non-aneurysmal, non-atherosclerotic descending thoracic aorta—an unusual source of arterial embolism. Eur J Vasc Endovasc Surg 2011;41:450–7 [DOI] [PubMed] [Google Scholar]
- 3.Abiko T, Sato S, Futamata T, et al. A case of pleomorphic leiomyosarcoma of the posterior mediastinum. J Japanese Assoc Chest Surg 2005;19:819–22 [Google Scholar]
- 4.Farshid G, Pradhan M, Goldblum J, et al. Leiomyosarcoma of somatic soft tissues: a tumor of vascular origin with multivariate analysis of outcome in 42 cases. Am J Surg Pathol 2002;26:14–24 [DOI] [PubMed] [Google Scholar]
- 5.Reber PU, Patel AG, Stauffer E, et al. Mural aortic thrombi: An important cause of peripheral embolization. J Vasc Surg 1999;30:1084–9 [DOI] [PubMed] [Google Scholar]
- 6.Machleder HI, Takiff H, Lois JF, et al. Aortic mural thrombus: an occult source of arterial thromboembolism. J Vasc Surg 1986;4:473–8 [PubMed] [Google Scholar]


