Abstract
Granulomatosis with polyangiitis (Wegener's) (GPA) is a chronic disease of unknown aetiology that leads to necrotising vasculitis in small and medium-sized vessels characterised by respiratory system and kidney involvement. Intestinal involvement is rare and perforation is even rarer in GPA. In this study, we are presenting a literature review of related cases, and a 29-year-old man referred from the emergency department with a multiple distal ileal perforation that was diagnosed with GPA, and successfully treated with rituximab.
Background
Treatment of steroid and cyclophosphamide-resistant granulomatosis with polyangiitis (Wegener's) (GPA) patients becomes gradually increasing matter of fact. However, there are emerging biological therapeutic alternatives that promise valuable progress. Generating new alternatives for steroid and cyclophosphamide-resistant patients is very important. Owing to the immunosuppressive features rituximab seems to be a promising therapy in GPA and we have decided to present it in this case report.
Case presentation
Introduction
GPA is a chronic multisystemic disorder of unknown aetiology that leads to necrotising vasculitis in small-sized and medium-sized vessels characterised by respiratory system and kidney involvement.1 In the light of the latest data, as a rare case, the prevalence of GPA was estimated to be at least 3 cases/100 000 persons.2
Although intestinal involvement is rare in GPA, the disease can be presented with obstruction, rectal bleeding, perforation or ileo-colonic ulcers. Owing to life-threatening complications such as intestinal perforation in the early stage of the disease, the diagnosis and treatment of GPA is vitally important.1 3 Although the use of rituximab in the treatment of many forms with different systemic involvement of GPA has been shown to be useful, there is limited data concerning the management of severe intestinal involvement.4
Besides the clinical and histopathological findings, high sensitivity and specificity of cytoplasmic antineutrophil cytoplasmic antibodies (c-ANCA) positivity is extremely important for diagnosis of the disease during the acute stage.5 We, here, present a severe progressive of the GPA case with a multiple distal ileal perforation developed in the aftermath of diagnosis and during treatment that reached remission with rituximab added to conventional therapy. Furthermore, we are presenting a compilation of GPA cases with intestinal involvement treated with rituximab.
Case report
A 29-year-old man was admitted to the gastroenterology clinic with complaints of bloody stools and rectal bleeding six or seven times in a day. The patient had a history of 6-month arthralgia, haemoptysis inflamed in the last 3 weeks, the outer right leg red colour rash and bloody stools, since the day before admission to the clinic. The laboratory analyses revealed the following; white blood cell count 19 000/mm3, haemoglobin 12 g/dl, platelet 363 000/ mm3, C reactive protein 197 mg/l, erythrocyte sedimentation rate 83 mm/h and creatine 0.9 mg/dl.
In the colonoscopy of the patient, circle-shaped diffuse 1–3 cm multiple ulcers were observed in distal ileum, the caecum, ascending colon and hepatic flexura in the first 40 cm, where there was no detected bleeding focus (figure 1). Histopathological evaluation of the distal ileum and caecum's biopsies showed non-specific, active-chronic inflammation and ulcer bases. Stool microscopy and culture revealed no evidence of infectious agent. Rectal bleeding improved on the third day following palliative treatment. Chest CT analyses due to haemoptysis demonstrated peripherally localised fibro-reticular infiltration areas in bilateral lungs (figure 2). Although there was a progressive deterioration in proteinuria and kidney function tests of the patients during hospitalisation, the patient's serum c-ANCA (PR3) test was positive (54.4 U/ml, normal level 0–5 U/ml). In order to observe and measure the disease's activity, we have used Birmingham Vasculitis Activity Score (BVAS) for Wegener's granulomatosis (WG). BVAS/WG scores range from 0 to 63, with higher scores indicating more active disease.6 Prior to the treatment, BVAS/WG score of the patient was 54 which is considered as a severe disease. After the patient was diagnosed with GPA comorbiding Ileo-colonic involvement, methylpredinisolone 1 g/day, bolus (3 days) and then 1 mg/kg/day orally and 750 mg/m2/month cyclophosphamide treatment was started. On the seventh day of the treatment, acute abdomen and direct x-ray showed free air under the diaphragm, and during laparotomy, seven different perforation points were detected in the distal ileum. Pathological examinations revealed vasculitic changes (figure 3). On the 28th day of the treatment, the patient's BVAS/WG was remeasured, and there were improvements which were not sufficient to eliminate the patient's complains (28th day BVAS/WG score, 40). Owing to aggressive progression of the disease, we have planned a four-cured rituximab therapy with a dosage of 1000 mg intravenously administered twice in the course of 15 days, which will be repeated in the 6th and 12th month. There was an observable improvement in clinical, radiological and laboratory parameters of the patient following the second rituximab cure (BVAS/WG score on 16th day after rituximab therapy, 17). The patient remained asymptomatic for 6 months after the third cure and is still under follow-up.
Figure 1.
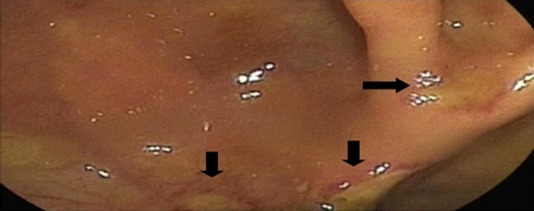
Multiple ulcers in the caecum that show colonic involvement.
Figure 2.

Fibro-reticular infiltration areas in bilateral lungs.
Figure 3.
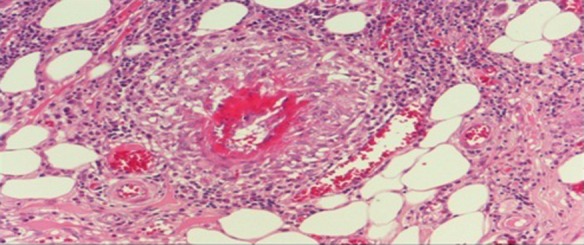
Vasculitis image in the distal ileum tissue.
Outcome and follow-up
The patient remains asymptomatic and under remission for 6 months after the third cure and is still under follow-up.
Discussion
Owing to GPA's multisystemic nature, it can be presented with diverse clinical features and because of that differential diagnoses of the disease are needed . Roughly, 90% of GPA cases have lesions of upper respiratory tract, 87% have lesions in lungs, 85% in kidneys and rarely vasculitic skin lesions.7 Diagnostic clinical findings and serum c-ANCA positivity, held to show the presence of any tissue, granuloma, or vasculitis, and the differential diagnosis by excluding other diseases, which are placed. In our case, the lung parenchyma and prominent infiltrates, renal involvement, vasculitic skin lesions and c-ANCA were positive and had severe intestinal involvement.
The initial treatment is generally started with a corticosteroids and cyclophosphamide combination and expected treatment was achieved in several cases. Especially, the use of cyclophosphamide in the last 2 years, diminished the death rates by almost 80%. A recent study concerning the use of rituximab, a chimeric anti-CD20 monoclonal antibody, in GPA patients having systemic involvement and faced with serious adverse events during the use of immunosuppressive drugs or had resistance to these drugs, showed sustainable remission in these patients.8 On the other hand, there were very limited data concerning the use of rituximab in GPA cases with intestinal perforation. A detailed literature review revealed that there were four GPA cases reported. In these reported cases, the patients had life-threatening serious perforation and complications, aggressive intestinal involvement and other systemic involvements. These patients were treated with rituximab and achieved sustainable remission due to limited response or adverse events with immunosuppressive drugs (table 1).4 9–11 In our case, the patient had intestinal perforation and multiple systemic involvements under initial classical treatment and initiation of rituximab led to a valuable response, and the patient's BVAS/WG score diminished significantly. While rituximab was used 375 mg/m2 in four cures in previously reported cases, we planned 1000 mg/intravenously in four cures to achieve sustainable remission.
Table 1.
Reported cases concerning the use of rituximab in WG patients with intestinal involvement
| Author/year of publication | Number of cases | Sex/age | Involvement | Type of bowel involvement | c-ANCA | Indication | Previous treatment | Therapy regimen | Follow-up duration |
|---|---|---|---|---|---|---|---|---|---|
| Minami et al (2007)9 | 1 | F/55 | Upper respiratory tract, eyes, lungs, bowel and neurological | Intestinal perforation | + | Refractory disease , aggressive progression | Steroid cyclophosphamide γ-globulin | 375 mg/m2/every 4 weeks Totally 4 cures | 14 months |
| Oristrellet al (2009)4 | 1 | M/73 | Upper respiratory tract, lungs, bowel, | Mesenteric ischaemia, intestinal perforation | + | Pancytopenia and infection due to cyclophosphamide , aggressive progression | Steroid cyclophosphamide | 375 mg/m2/every 4 weeks Totally 4 cures | 22 months |
| Steinbach et al (2010)9 | 1 | NA/45 | Lungs, bowel, kidney | Paralitic ileus, haemorrhagic necrosis | + | Aggressive progression | Steroid cyclophosphamide | Rituximab Dosage: NA | NA |
| Witsch et al (2011)10 | 1 | F/70 | Lungs, bowel, neurological, kidney | Intestinal haemorrhagy, ileo-caecal involvement | + | Aggressive progression | Steroid plasmapheresis γ-globulin | 375 mg/m2/every 4 weeks totally 4 cures | NA |
In GPA, gastrointestinal involvement is very rare and, in several cases, it is reported to be around 10–24%.1 More importantly, the cases presented with serious intestinal involvement, early intestinal perforation or rectal bleeding are rarer.3 12 These cases are generally non-specific in colonoscopic biopsies and are generally reported as acute/chronic inflammations and mucosal ulcerations. Patients having intestinal perforation also had rare vasculitic changes in the perforation area. Owing to the initial immunosuppressive treatment, most of the patients did not reveal typical histopathological changes. There are also some other cases reporting that, in perforation cases, the use of immunosuppressive drugs would lead to an increase in risk of perforation.13 14 In the present case, the results of colonoscopic biopsies are non-specific and there are limited vasculitic changes in perforal intestinal segment. Other histopathological findings that may support the comorbid existence of other inflammatory bowel diseases are not observed. Unlike other reported cases, perforation development was observed in a short while following the first week after diagnoses. Despite presence of vasculitis in perforation material, the role of colonoscopy and biopsy in the previous week and immunosuppressive treatment during this period is estimated besides the perforation aetiology of GPA.
c-ANCA positivity plays a crucial role in serological diagnosis of GPA. c-ANCA is a type of autoantibody, produced by the T lymphocytes against cytoplasmic antigens of neutrophils and, according to recent analyses, the sensitivity and specificity of c-ANCA in active GPA patients varies from 66% to 98%, respectively. However, the negativity of c-ANCA is possible during limited or inactive diseases, and this situation must be estimated.5 In this reported case, besides multisystemic involvement, aggressive progression and acute diseases’ findings, the c-ANCA scores were 11 times higher than the normal laboratory limits.
Consequently, the presented case report illustrates that, although there is rarity of intestinal involvement, life-threatening complications such as intestinal perforation can be seen in the early stage of the disease, and anti-CD20 antibody rituximab, added to conventional therapy, will provide successful induction and maintenance of remission. However, further experimental randomised studies are needed to verify and prove the results and findings presented in this study.
Learning points.
Rituximab is likely to be effective in steroid and cyclophosphamide-resistant granulomatosis with polyangiitis (Wegener's) patients.
Rituximab is safely tolerated and no adverse event observed during the treatment.
Adding rituximab to conventional therapy will provide successful induction and maintenance of remission in patients with GPA and comorbiding complications like intestinal perforation.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Fauci AS, Haynes BF, Katz P, et al. Wegener's granulomatosis: prospective clinical and therapeutic experience with 85 patients for 21 years. Ann Intern Med 1983;98:76–85 [DOI] [PubMed] [Google Scholar]
- 2.Langford CA, Hoffman GS. Rare diseases. 3: Wegener's granulomatosis. Thorax 1999;54:629–37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Samim M, Pronk A, Verheijen PM. Intestinal perforation as an early complication in Wegener's granulomatosis. World J Gastrointest Surg 2010;2:169–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Oristrell J, Bejarano G, Jordana Ret al. Effectiveness of rituximab in severe Wegener's granulomatosis: report of two cases and review of the literature. Open Respir Med J 2009;3:94–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rao JK, Weinberger M, Oddone EZ, et al. The role of antineutrophil cytoplasmic antibody (c-ANCA) testing in the diagnosis of Wegener granulomatosis. A literature review and meta-analysis. Ann Intern Med 1995;123:925–32 [DOI] [PubMed] [Google Scholar]
- 6.Stone JH, Hoffman GS, Merkel PAet al. A disease-specific activity index for Wegener's granulomatosis: modification of the Birmingham Vasculitis Activity Score. International Network for the Study of the Systemic Vasculitides (INSSYS). Arthritis Rheum 2001;44:912–20 [DOI] [PubMed] [Google Scholar]
- 7.Duna GF, Galperin C, Hoffman GS. Wegener's granulomatosis. Rheum Dis Clin North Am 1995;21:949–86 [PubMed] [Google Scholar]
- 8.Seo P, Specks U, Keogh KA. Efficacy of rituximab in limited Wegener's granulomatosis with refractory granulomatous manifestations. J Rheumatol 2008;35:2017–23 [PubMed] [Google Scholar]
- 9.Minami R, Miyamura T, Watanabe H, et al. Successful treatment of a patient with refractory Wegener's granulomatosis by rituximab. Nihon Rinsho Meneki Gakkai Kaishi 2007;30:133–8 [DOI] [PubMed] [Google Scholar]
- 10.Steinbach J, Bartsch P, Langer D, et al. (Necrotizing granulomatosis with pulmonary, intestinal and renal involvement. Med Klin (Munich) 2010;105:831–6 [DOI] [PubMed] [Google Scholar]
- 11.Witsch J, Stenzel W, Witsch T, et al. Rituximab in c-ANCA associated vasculitic polyneuropathy complicated by local peritonitis. J Neurol 2011;258:2281–315 [DOI] [PubMed] [Google Scholar]
- 12.Qian Q, Cornell L, Chandan V, et al. Hemorrhagic colitis as a presenting feature of Wegener granulomatosis. J Gastrointestin Liver Dis 2010;19:445–7 [PubMed] [Google Scholar]
- 13.Storesund B, Gran JT, Koldingsnes W. Severe intestinal involvement in Wegener's granulomatosis: report of two cases and review of the literature. Br J Rheumatol 1998;37:387–90 [DOI] [PubMed] [Google Scholar]
- 14.Muller-Ladner U. Vasculitides of the gastrointestinal tract. Best Pract Res Clin Gastroenterol 2001;15:59–82 [DOI] [PubMed] [Google Scholar]


