Abstract
Fibrous dysplasia is a bone pathology characterised by abnormal differentiation of osteoblasts leading to replacement of normal marrow and cancellous bone by immature bone and fibrous stroma. A case report of a 20-year-old female patient with a chief complaint of a swelling in the right upper back tooth region, of 6 months duration which was diagnosed as an immature fibrous dysplasia is presented.
Background
Fibrous dysplasia was first described by Lichtenstein in 1938.1 Fibrous dysplasia is a bone pathology characterised by abnormal differentiation of osteoblasts leading to the replacement of normal marrow and cancellous bone by immature bone and fibrous stroma.2 The fibroblastic proliferation and immature woven bone have been traced to a mutation in the Gsα gene at chromosome 20q13.2–13.3.3 4 The usual course of the disease involves an osteolytic stage and fibro-osteoblatic proliferation. The osteolysis process destroys the normal bony architecture in the affected region followed by deposition of a fibrous stroma. The fibrous stroma gradually proceeds to calcification in the form of an immature woven bone.
Case presentation
A 20-year-old female patient reported to the outpatient department of oral and maxillofacial surgery with a chief complaint of a swelling in the right upper back tooth region, of 6 months duration. Relevant medical history revealed that patient had developed pain in right maxillary posterior region 2 years back, for which she got her second maxillary molar extracted. With the initial intervention the pain subsided and she remained asymptomatic for 6 months. After a year following dental extraction, she again developed pain in the same region. This time her first right maxillary molar was also extracted based on a suspicion of pain of dental origin at the same clinic, where patient was also advised a course of clindamycin, due to a suspicion of osteomylitis. After this, a palatal swelling appeared in the region of the extracted teeth, which was associated with dull aching pain, which bought the patient to us. The patient gave a history of a very slow increase in size of the swelling since then. On clinical examination, the swelling extended from the second right maxillary premolar to the third right maxillary molar. The second right maxillary premolar was mobile (grade II) and the swelling was tender on palpation. The right maxillary posterior vestibule was obliterated. The firm swelling was limited to 2 cm from the mid palate in its medial extent. Based on the consistency and inspectory findings, a provisional diagnosis of malignant bony pathology was considered.
Investigations
CT scan was advised for radiological assessment of the lesion. CT scan revealed a radiolucent lesion with specks of radiodensities in the mass and the destruction of normal bony architecture in the region. The CT scan findings pointed toward the working diagnosis of an ossifying fibroma of the right posterior maxillary region (figure 1). An incisional biopsy was planned to confirm the diagnosis before subjecting the patient for complete excision of the pathological mass.
Figure 1.
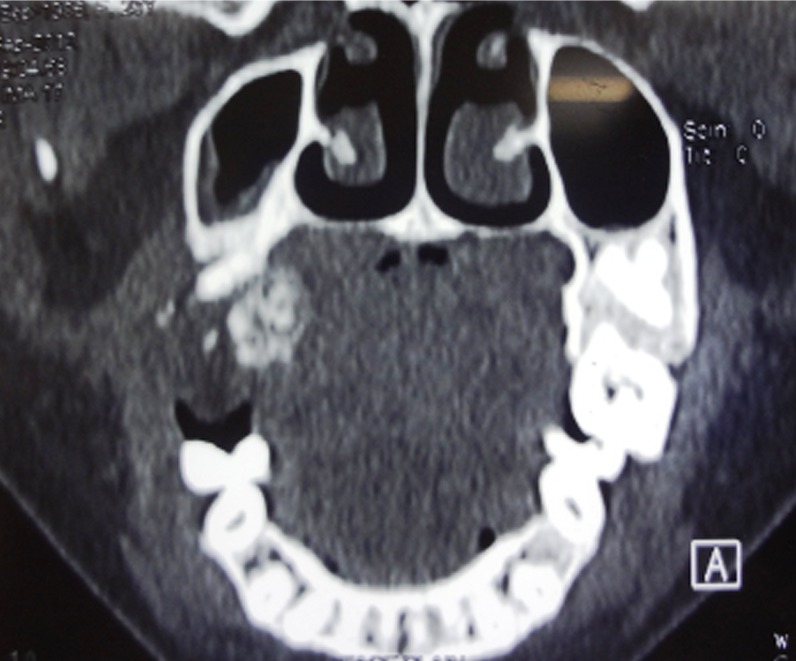
CT image (coronal) showing the right posterior maxillary lesion with calcifications.
The incisional biopsy specimen when processed with the standard protocol for H&E staining revealed osseous structures in a fibrous stoma, suggestive of a fibro-osseous lesion.
Differential diagnosis
As the case was initially presented to the department, a suspicion of a malignant bony pathology was high among all the differentials, considering the duration of the pathology. Incisional biopsy pointed toward a diagnosis of a fibro-osseous lesion in posterior maxilla.
Treatment
The complete surgical excision of the mass was done after reflection of a triangular buccal flap from first right maxillary premolar to the third molar region (figures 2 and 3). The second right maxillary premolar and the third molar were clinically involved in the pathological mass, and were extracted during the excision of the lesion. The excised specimen was subjected to the histopathological examination which confirmed the diagnosis of maturing fibrous dysplasia (figure 4).
Figure 2.

Right posterior maxillary alveolus after resection of the lesion.
Figure 3.

Resected specimen.
Figure 4.
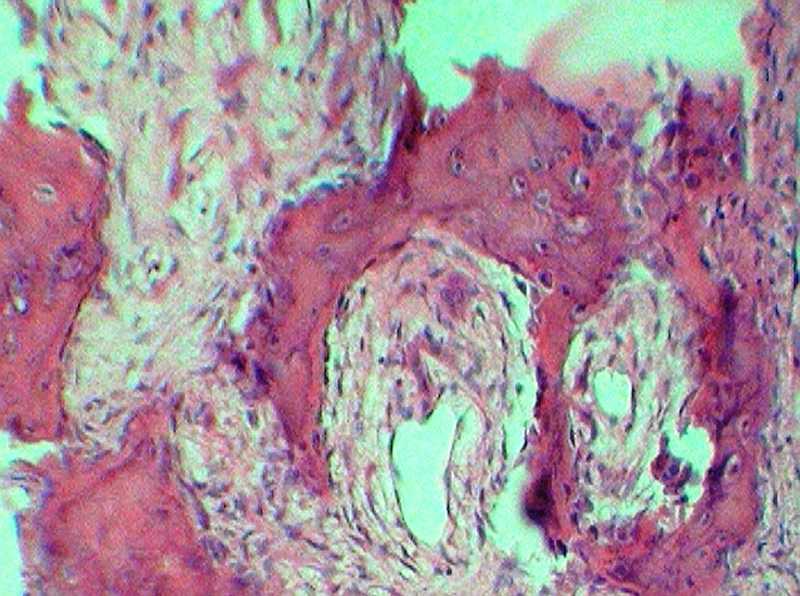
Chinese letter pattern of calcification typical of fibrous dysplasia (40× H&E).
Outcome and follow-up
Postexcision, the patient had reduction in pain with satisfactory healing at the surgical site. The patient was rehabilitated with an immediate denture (figures 5 and 6).
Figure 5.

Surgical site at the fifth postoperative day.
Figure 6.
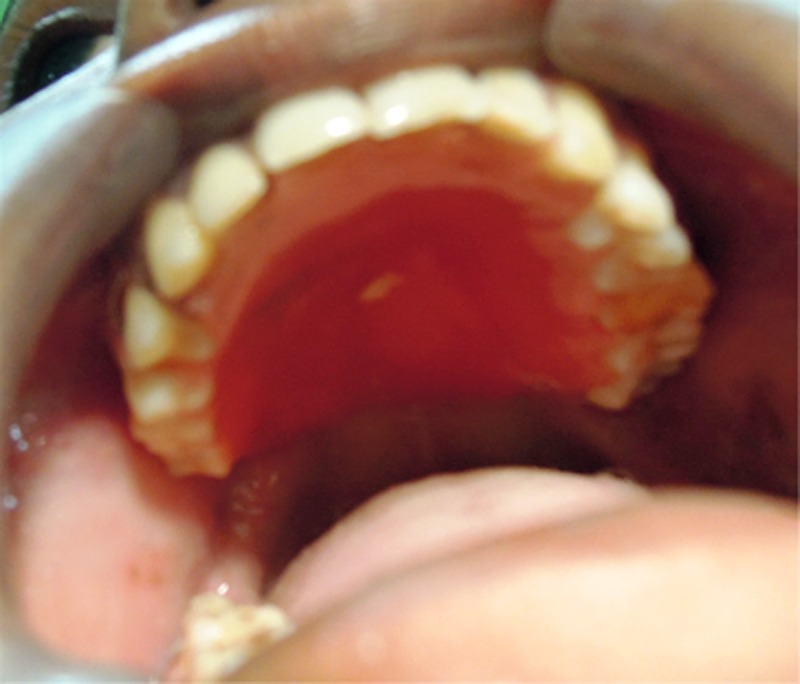
Rehabilitation with a removable partial denture.
Discussion
Fibro-osseous lesions are characterised by replacement of normal bone with pathological calcifications in a hypercellular fibroblastic marrow.5 Fibrous dysplasia is common benign fibro-osseous pathology that affects the jawbones.6 Fibrous dysplasia usually arises within the first or second decades of life. The incidence of craniofacial involvement in fibrous dysplasia has been reported as 10–25% in the monostotic form and 50–90% in polyostotic form.7 Fibrous dysplasia involving the craniofacial complex can be broadly classified into monostotic, polyostotic or polyostotic with associated endocrinopathy (Jaffe-Lichtenstein syndrome, McCune-Albright syndrome, and Mazabraud syndrome). The monostotic forms limiting to the bones of the cranio-facial skeleton are better classified as ‘craniofacial fibrous dysplasia’ because of the suture crossing character of the pathology in this region. The usual clinical presentation is of a slow-growing, painless expansion of the affected bone.8 In the case presented, patient was in second decade of her life and contrasting to the reviewed literature, patient presented with pain in the right posterior maxillary region. The radiographic appearance of fibrous dysplasia differs with the stage of development and ossification and is described as well defined and radiolucent at initial stages to largely sclerotic matured forms. Classically fibrous dysplasia is represented as a ground-glass or orange-peel appearance which blends with normal surrounding bone.5 The lesion in the patient presented in this case report appeared as mixed radio-opaque and radiolucent, correlating with the stage of initial calcifications in a fibrous stroma. Loss of lamina dura in the involved teeth is a characteristic finding in classical fibrous dysplasia.8–10 Two of the maxillary molars (16, 17) were missing at the presentation in the out-patient department, out of the other two teeth (15, 18) which were involved in the lesion; the second maxillary premolar did not show any loss of lamina dura. The maxillary third molar had partial loss of the lamina dura. This presentation may be a feature of the initial osteolytic stage with fibrous tissue deposition and preliminary phase of woven trabaculae formation. A clear surgical plane for dissection was noted between the normal bone and the pathological mass. This was contrasting to the cases which present with matured fibrous dysplasia in maxillofacial region.
Learning points.
Immature fibrous dysplasia of maxillofacial region may have a varied radiographic presentation from a radiolucent to mixed to a matured radiolucent lesion, and therefore should be considered as an important differential diagnosis in all three forms of presentation.
Fibrous dysplasia may present clinically mimicking a bony malignancy.
Histopathology remains a gold standard to the diagnosis of fibrous dysplasias.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Chen YR, Chang CN, Tan YC. Craniofacial fibrous dysplasia: an update. Chang Gung Med J 2006;29:543–9 [PubMed] [Google Scholar]
- 2.Fitzpatrick KA, Taljanovic MS, Speer DP, et al. Imaging findings of fibrous dysplasia with histopathologic and intraoperative correlation. AJR Am J Roentgenol 2004;182:1389–98 [DOI] [PubMed] [Google Scholar]
- 3.Weinstein LS, Shenker A, Gejman PV, et al. Activating mutations of the stimulating G protein in the McCune-Albright syndrome. N Engl J Med 1991;325:1688–95 [DOI] [PubMed] [Google Scholar]
- 4.Weinstein LS, Chen M, Liu J. Gs (alpha) mutations and imprinting defects in human disease. Ann NY Acad Sci 2002;968:173–97 [DOI] [PubMed] [Google Scholar]
- 5.Eversole R, Su L, ElMofty S. Benign fibro-osseous lesions of the craniofacial complex. A review. Head Neck Pathol 2008;2:177–202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alawi F. Benign fibro-osseous diseases of the maxillofacial bones. A review and differential diagnosis. Am J Clin Pathol 2002;118 (Suppl):S50–70 [DOI] [PubMed] [Google Scholar]
- 7.Ricalde P, Magliocca KR, Lee JS. Craniofacial fibrous dysplasia. Oral Maxillofac Surg Clin North Am 2012;24:427–41 [DOI] [PubMed] [Google Scholar]
- 8.Eversole LR. Craniofacial fibrous dysplasia and ossifying fibroma. Oral Maxillofac Surg Clin North Am 1997;9:625–42 [Google Scholar]
- 9.Mohammadi-Araghi H, Haery C. Fibro-osseous lesions of craniofacial bones: the role of imaging. Radiol Clin North Am 1993;31:121–34 [PubMed] [Google Scholar]
- 10.Waldron CA. Fibro-osseous lesions of the jaws. J Oral Maxillofac Surg 1993;51:828–35 [DOI] [PubMed] [Google Scholar]


