Abstract
Background
Cancer patients and their oncologists often report differing perceptions of consultation discussions and discordant expectations regarding treatment outcomes. CONNECT™, a computer-based communication aid, was developed to improve communication between patients and oncologists.
Methods
CONNECT includes assessment of patient values, goals, and communication preferences; patient communication skills training; and a pre-consult physician summary report. CONNECT was tested in a three-arm, prospective, randomized clinical trial. Prior to the initial medical oncology consultation, adult patients with advanced cancer were randomized to (a) control; (b) CONNECT with physician summary, or (c) CONNECT without physician summary. Outcomes were assessed with post-consultation surveys.
Results
Of 743 patients randomized, 629 completed post-consultation surveys. Patients in the intervention arms (versus control) felt that the CONNECT program made treatment decisions easier to reach (p=0.003) and helped them to be more satisfied with these decisions (p<0.001). In addition, patients in the intervention arms reported higher levels of satisfaction with physician communication format (p=0.026) and discussion regarding support services (p=0.029) and quality of life concerns (p=0.042). The physician summary did not impact outcomes. Patients with higher levels of education and poorer physical functioning experienced greater benefit from CONNECT.
Conclusion
This prospective randomized clinical trial demonstrates that computer-based communication skills training can positively affect patient satisfaction with communication and decision making. Measureable patient characteristics may be used to identify subgroups most likely to benefit from an intervention such as CONNECT.
Keywords: Cancer communication, health communication, physician-patient communication, decision making, computer assisted, cancer
Introduction
Cancer patient treatment decision making ideally involves consideration of potential outcomes in the context of individual values and goals. A primary source of information for patients is their oncologists. However, data suggest that communication between cancer patients and their oncologists may be suboptimal.1–3 We4, 5 and others6 previously reported that advanced cancer patients have discordant expectations compared with their physicians regarding potential benefits and toxicities of therapeutic options. For example, we found that patients considering phase I trials overestimate the potential benefits and toxicities associated with both standard and investigational therapy.4 Although optimistic expectations of benefit among patients may not always be a source of bioethical concern,7 we also found that patients and their doctors differ markedly in their perceptions of topics discussed during their consultations. In a survey of advanced cancer patients and their oncologists, 73% of doctors reported that they discussed the impact of treatment on quality of life (QOL), but only 28% of patients reported that this topic was discussed.4 This observation is of particular interest given that 95% of these patients reported that QOL was at least as important to them as length of life (LOL). These findings raised concern regarding the adequacy of patient-provider communication.
We sought to develop an intervention to assist patients and their physicians in matching communication to individual patient values and needs. The Cognitive-Social Health Information Processing (C-SHIP) framework is a theoretical model that delineates the psychosocial factors involved in health information processing.8, 9 C-SHIP postulates that health information processing is influenced by the individual’s unique constellation of cognitive and affective factors (i.e., disease and treatment related expectancies and beliefs; concerns and worries, values and goals) that influence satisfaction and decision making. In addition, C-SHIP postulates that to the extent to which information provides clear action planning, there will be greater likelihood that the targeted health action, i.e., enhanced communication skills, will be adopted and valued.
Based on this framework, we adapted a communication skills training intervention from the primary care setting (PACE system, Presenting Information, Asking Questions, Checking Understanding, Expressing Concerns)10, 11 and designed an interactive web-based communication aid that assesses patient information and communication preferences (cognitions); cancer-specific anxiety and values (affects); and provides communication skills training to patients to facilitate planful actions.12, 13 We conducted a prospective, randomized clinical trial to test the hypothesis that the communication aid (CONNECT™: Cinicaltrials.gov registration ID NCT00244868) would improve satisfaction with patient-physician communication, reduce decisional conflict and generate more accurate expectations about the benefits and toxicities associated with treatment. Further, we explored background characteristics (e.g., education, marital status, physical status) that could potentially moderate the impact of the intervention.
Methods
Study Participants
Eligible participants were cancer patients at three academic medical centers. Eligibility criteria included: 1) first outpatient consultation with a medical oncologist at the study center; 2) documented metastatic solid tumor; 3) ≥ 18 years of age; 4) able to read English; 5) written informed consent. Potential participants were identified by review of new patient schedules and medical information forwarded at the time of scheduling, before the initial medical oncologist consultation. Medical oncologists for each patientgave permission to contact eligible patients and provided written consent to be audio taped and to receive summary reports of patient baseline surveys before the consultation. This study was approved by institutional review boards at the study sites (Fox Chase Cancer Center, Philadelphia, PA; Robert H. Lurie Comprehensive Cancer Center, Chicago, IL; and MeharryMedical College, Nashville, TN). All patients provided written informed consent before participating in the study.
Procedures
Recruitment procedures were described previously.13 Briefly, a Health Educator at each site contacted eligible patients by phone to explain the study. If patients agreed to participate, the Health Educator entered their information into a secure web-based patient tracking system that randomized participants to one of three arms: A) control group; B) communication aid, which included a preferences and values assessment, and communication skills training (CST),plus summary report to the physician; and C) communication aid and CST without physician summary. Randomization was stratified by participant gender. Participants had the option to complete the baseline survey at home or at the clinical center immediately before their appointment. All participants received a unique username and created a password to access the secure web site, reviewed electronic informed consent and HIPAA forms before beginning the survey, and typed their names into text boxes indicating agreement to provide written consent upon arriving for their consultation. They received a toll-free number for technical support, and only minimal assistance was required to help participants uncomfortable with computers. For participants randomized to Arm B, an automated report was generated and printed for the medical oncologist to review prior to the consultation. This three-page paper report summarized participant responses regarding current health state, cancer-related distress, shared decision making preferences, values assessment, and communication preferences.
Participants received a post-consultation paper survey to return by mail immediately after the consultation, and at three months post-consultation, a final follow up survey was mailed to the participants.
Intervention
Randomization was 1:1:1 among the study arms, and patients were blinded to their assignment. The web-based application consisted of two components: computer survey and communication skills training.
Communication Skills Training(CST) was provided to patients in the two intervention groups after baseline survey completion (control group participants were given a link to the National Cancer Institute’s website).11 The CST module featured four diverse cancer patients who “talked” (through short written narratives) to participants about four subjects: 1) How to prepare for your visit, 2) How to talk to your doctor, 3) What to ask your doctor about your medical condition, 4) What to ask your doctor about your lifestyle needs. The CST module was written at a 7th grade reading level. Participants were given the opportunity to print questions from this module to ask their doctors. Based on pilot testing the CST module was expected to take approximately 15 minutes.
Measures
The baseline computer survey for the intervention groups collected demographic information and measured cancer-related distress,14 decision making preference,15, 16 relative health stock,17, 18 value assigned to quality of life and length of life,4, 7, 13 communication preferences,19 interest in clinical trials, and current health state.20 The baseline survey for control group participants included only demographics, current health state, and cancer-related distress. The post-consultation survey assessed consultation content,4 treatment outcome expectations,4 decisional conflict,21 patient satisfaction with the content and format of the communication, and satisfaction with the survey and/or communication skills training. The 3-month follow-up survey reassessed participants’ decisional conflict, current health state, cancer-related distress, and treatment outcome expectations.
Statistical Analyses
We used ANOVA tests to compare average baseline differences in continuous variables and chi-square tests to compare proportions in baseline categorical variables among study groups. We used simple and multiple linear regressions with robust standard errors to investigate whether there were differences in satisfaction and decisional conflict among treatment arms, and also whether such outcomes were moderated by demographic characteristics. We used multiple linear regressions with robust standard errors to examine intervention differences between arms on patient expectations. The robust standard errors22 accounted for clustering within physician. The study protocol pre-specified outcome comparisons among pairwise arms and also between the control arm and the combined intervention arms.
Subgroups for exploratory analyses were created by dichotomizing education (high school education or less versus more than a high school education) and SF-12 health survey subscales20 (<=50 versus >50 on a 0 to 100 point scale).
The criterion for statistical significance was defined as a p-value of less than 0.05. We considered standard effect sizes of 0.2, 0.5, and 0.8 as modest, moderate, and large clinical effects. The protocol did not specify adjustment for multiple hypothesis testing.
Results
Participant Characteristics
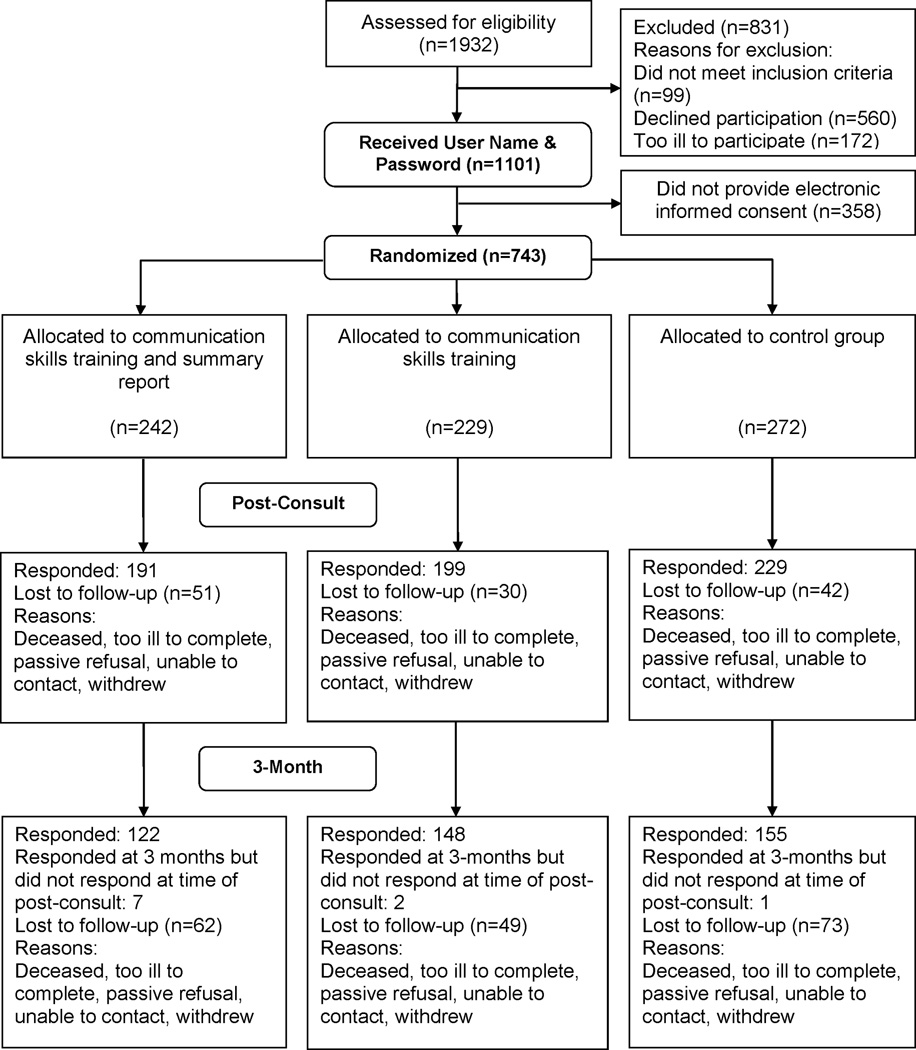
1932 patients were contacted and 1101 (57%) agreed to be assigned a password to consider participation. 743 patients (68%) provided informed consent, were randomized, and completed baseline surveys. 629 of the 743 patients completed post-consultation or three-month follow-up surveys (Figure 1). Patient demographics are shown in Table 1. The sample that completed at least one post-baseline survey was primarily white (92%), male (51%), and well-educated (41% with a college degree). There were no significant differences in demographic variables shown in Table 1 between study groups by ANOVA or chi-squared tests. Patients reported the following prior cancer treatments: intravenous (44.8%), surgical (44.8%), hormonal (11%), and radiation (27.5%).Of the 42 physicians who participated in the study, 86% were white, 60% were male, and the average age was 45.2 +/−9.4 years.
Figure 1.
CONSORT Diagram
Table 1.
Patient Baseline Demographics
| Control Arm A |
Physician Summary Arm B |
No Physician Summary Arm C |
P-value | |
|---|---|---|---|---|
| Number | 230 | 198 | 201 | |
| Age (mean, SD) | 58.8 (11.3) | 59.7 (11.1) | 60.0 (12.0) | NS |
| Sex/gender | NS | |||
| Male | 119 (52%) | 106 (54%) | 94 (47%) | |
| Female | 111 (48%) | 90 (46%) | 104 (53%) | |
| Race | NS | |||
| Black | 13 (6%) | 6 (3%) | 13 (6%) | |
| White | 212 (92%) | 186 (94%) | 181 (90%) | |
| Other | 5 (2%) | 6 (3%) | 7 (3%) | |
| Education | NS | |||
| High School | 69 (30%) | 67 (34%) | 49 (24%) | |
| Some College | 68 (30%) | 58 (29%) | 58 (29%) | |
| College | 92 (40%) | 73 (37%) | 94 (47%) | |
| Married/Partnered | 185 (80%) | 160 (81%) | 148 (74%) | NS |
| High Physical Function (SF-12 physical function >50) |
104 (45%) | 85 (43%) | 86 (43%) | NS |
| Diagnosis | NS | |||
| Breast | 21 (9%) | 24 (12%) | 21 (11%) | |
| Colorectal | 42 (18%) | 33 (17%) | 27 (13%) | |
| Esophagus/Stomach | 11 (5%) | 8 (4%) | 10 (5%) | |
| Lung | 43 (19%) | 35 (18%) | 31 (15%) | |
| Pancreas | 15 (7%) | 12 (6%) | 14 (7%) | |
| Prostate | 11 (5%) | 15 (8%) | 16 (8%) | |
| Renal | 17 (7%) | 9 (5%) | 12 (6%) | |
| Other | 70 (30%) | 62 (31%) | 70 (35%) |
Includes only patients who completed a follow-up survey; partner status data missing, n=1; physical function data missing, n=1; NS = p value > 0.10
Intervention Effects
There were no statistically significant and clinically relevant differences between the two intervention arms on any of the satisfaction or decisional conflict responses. Hence, we combined the intervention arms and compared them to the control arm in all subsequent analyses. Table 2 summarizes the satisfaction outcomes among the three study arms. Patients who were assigned to the intervention arms had higher levels of satisfaction with discussions about the format of physician communication (p<0.05) and quality of life issues (p=0.04). No statistically significant differences in satisfaction were seen regarding discussion of diagnosis/prognosis, treatment options, or support/community services. There were no statistically significant differences between the study arms in the decisional conflict scores. However, patients assigned to the intervention arms felt that taking part in the program made their decisions easier to reach (p<0.01) and helped them be more satisfied with their treatment decisions (p<0.001).
Table 2.
Intervention Effect on Satisfaction, Mean (SD)
| Variable Satisfaction with Communication (0 = Not Satisfied; 3 = Extremely Satisfied) |
Control Arm A mean (SD) |
Arm B (Physician Summary) mean (SD) |
Arm C (No physician Summary) mean (SD) |
Regression difference and p-value comparing two intervention arms to control, 95% confidence interval |
|---|---|---|---|---|
|
Satisfaction with discussion about diagnosis / prgnosis How satisfied were you with discussion about:
|
10.4 (3.9) | 10.5 (3.7) | 10.7 (3.7) | A vs. B, 0.0 (−0.6, 0.6) p=NS A vs. C, 0.3 (−0.2, 0.7) p=NS A vs. B/C, 0.2 (−0.3, 0.6) p=NS |
|
Satisfaction with discussion about treatment options How satisfied were you with discussion about:
|
14.9 (6.7) | 15.4 (6.0) | 16.1 (5.8) | A vs. B, 0.5 (−0.7, 1.8) p=NS A vs. C, 1.2 (0.1, 2.3) p<0.05 A vs. B/C, 0.9 (−0.1, 1.9) p<0.10 |
|
Satisfaction with discussion about support/community services How satisfied were you with discussion about:
|
3.0 (2.1) | 3.3 (1.8) | 3.4 (1.9) | A vs. B, 0.3 (−0.2, 0.8) p=NS A vs. C, 0.4 (−0.1, 0.9) p<0.10 A vs. B/C, 0.4 (−0.1, 0.8) p=NS |
|
Satisfaction with discussion about QOL How satisfied were you with discussion about your:
|
9.0 (4.6) | 9.9 (3.9) | 9.7 (4.3) | A vs. B, 0.8 (0.1, 1.5) p<0.05 A vs. C, 0.6 (−0.3, 1.6) p=NS A vs. B/C, 0.7 (0.01, 1.5) p<0.05 |
|
Satisfaction with format of communication How satisfied are you:
|
7.0 (2.4) | 7.4 (2.0) | 7.4 (2.0) | A vs. B, 0.4 (−0.1, 0.9) p<0.10 A vs. C, 0.4 (0.05, 0.8) p<0.05 A vs. B/C, 0.4 (0.03, 0.8) p<0.05 |
|
Overall Satisfaction 23 Questions |
44.9 (17.0) | 46.9 (14.8) | 47.5 (15.6) | A vs. B, 1.9 (−1.1, 4.9) p=NS A vs. C, 2.6 (−0.04, 5.2) p<0.10 A vs. B/C, 2.3 (−0.2, 4.7) p<0.10 |
|
Do you feel that taking part in this program made your decision easier to reach? |
0.9 (1.2) | 1.3 (1.2) | 1.2 (1.3) | A vs. B, 0.4 (0.2, 0.6) p<0.001 A vs. C, 0.3 (0.05, 0.5) p<0.05 A vs. B/C, 0.3 (0.1, 0.5) p<0.01 |
|
Do you feel that taking part in this program helped you to be more satisfied with your treatment decision? |
1.1 (1.2) | 1.6 (1.2) | 1.5 (1.3) | A vs. B, 0.4 (0.2, 0.7) p<0.01 A vs. C, 0.4 (0.2, 0.6) p<0.01 A vs. B/C, 0.4 (0.2, 0.6) p<0.001 |
NS = p value > 0.10
Covariates in intervention effect regressions included patient sex (sex was the sole stratification factor) and an intervention arm indicator.
In terms of patient expectations, those in the intervention arms were less likely to believe that they would experience severe side effects with standard or experimental therapy (p<0.05 for comparison of intervention arms to control arm). There was no intervention effect on expectations regarding control of cancer or control of symptoms.
Overall, the magnitude of the significant differences between the control and intervention arms was generally modest, ranging from 0.15 to 0.42 standard deviations of the variables measured. Because the observed differences were modest, we conducted post hoc exploratory analyses. These analyses revealed that among patients with greater than high school education, the CONNECT intervention was associated with increased satisfaction with discussion about prognosis/diagnosis (interaction p<0.05), support/community services (interaction p<0.001), and overall communication (interaction p<0.05). Likewise, patients with lower baseline quality of life on SF-12 who were assigned to the intervention arms had greater satisfaction with communication about prognosis/diagnosis (interaction p<0.05), quality of life (interaction p<0.05), format of communication (interaction p<0.05), and overall communication (interaction p<0.05).
Consistent with the findings regarding satisfaction with communication, exploratory analyses suggested a benefit from CONNECT in reducing decisional conflict at the 3-month follow up among patients reporting lower quality of life at baseline (Table 3). It should be noted that completion of 3-month follow up surveys was associated with higher education level, partnered status, better physical functioning, and non-African American race (all p < 0.05).
Table 3.
Exploratory Subgroup Analysis
| Variable | Control Mean (SD) |
Intervention Mean (SD) |
Difference from regression (95% CI) |
P-value from regression |
|---|---|---|---|---|
|
3-month Decisional Conflict Uncertainty Scale
|
Interaction p<0.05 |
|||
| Physical Function <= 50, worse function | 31.8 (25.0) |
27.5 (23.2) |
−4.4 (−11.2, 2.5) |
NS |
| Physical Function > 50, better function | 20.3 (21.0) |
26.8 (22.5) |
6.2 (0.2, 12.1) |
p<0.05 |
|
3-month Decisional Conflict Values Clarification Scale
|
Interaction p<0.05 |
|||
| General Health <= 50, worse function | 23.2 (17.4) |
19.3 (15.3) |
−4.2 (−8.4, −0.1) |
p<0.05 |
| General Health > 50, better function | 17.8 (15.8) |
19.1 (15.9) |
1.5 (−3.2, 6.1) |
NS |
|
3-month Decisional Conflict Values Clarification Scale |
Interaction p<0.05 |
|||
| Physical Function <= 50, worse function | 25.1 (17.0) |
19.3 (16.8) |
−5.8 (−10.9, −0.7) |
p<0.05 |
| –Physical Function > 50, better function | 16.8 (15.9) |
19.2 (14.1) |
2.2 (−2.6, 6.9) |
NS |
|
3-month Decisional Conflict Support Scale
|
Interaction p<0.01 |
|||
| Physical Function <= 50, worse function | 20.8 (14.4) |
16.0 (15.2) |
−4.8 (−10.1, 0.4) |
p<0.10 |
| Physical Function > 50, better function | 13.0 (14.1) |
17.4 (14.7) |
4.1 (0.3, 8.0) |
p<0.05 |
The p-values related to the subgroup effects reflect the within-subgroup treatment effect. The p-values related to the interaction term reflect whether the treatment effects differ by subgroups. NS = p value > 0.10
Covariates in subgroup (interaction) regressions include patient sex, arm indicator, subgroup indicator, and the interaction term of arm indicator times subgroup indicator.
Discussion
The web-based intervention (CONNECT) described in this report was designed to improve communication between cancer patients and their oncologists in order to optimize patient decision making. This study demonstrates that internet-basedCST results in improved satisfaction with the format of oncologist communication and discussion regarding quality of life. In addition, patients reported that the intervention made their treatment decisions easier to reach and helped them to be more satisfied with treatment decisions.
We 4, 11, 13 and others23, 24 reported that patients with advanced cancer tend to place a high value on quality of life. Among 328 patients considering participation in a phase I trial, 95% indicated that quality of life was at least as important as length of life.4, 13 In a publication of baseline data for patients in the experimental arms of the current randomized study,13 we reported that 27% preferred quality of life, 18% preferred length of life, and 55% placed an equal value of quality and length of life. Patients who preferred length of life desired a more supportive communication style from their oncologists. It is notable that the CONNECT intervention was most effective in improving satisfaction with communication regarding social and quality of life issues.
We conducted exploratory analyses to determine if there might be definable patient groups most likely to benefit from CONNECT. These exploratory subgroup analyses suggest that education level and physical functioning moderated the effect of CONNECT on patient satisfaction with communication. Specifically, the intervention appeared most effective among patients with higher educational level and poorer physical functioning. Although the skills training text was presented at a 7th grade reading level, it is conceivable that web-based interventions, in particular those that require reading, are best suited to those with more education. The results concerning poorer physical functioning are consistent with research suggesting that patients with more health concerns participate more in medical consultations.25 Here, patients with lower physical functioning may have been more interested in issues related to quality of life, and hence, were more likely to benefit from communication skills training in terms of satisfaction with relevant aspects of communication. Although we hypothesized that a physician summary would help focus communication format and content, a theory-guided patient cognitive-affective summary profile provided to the physician before the consultation did not affect study outcomes. This result is consistent with other findings suggesting that physician communication behavior change requires more extensive and sustained intervention than was possible in the present context.26–28 It is also plausible that physicians did not read the summaries before the patient visit, hence undercutting this aspect of the intervention. Concern has been raised about high expectations of benefit from treatment that cancer patients typically express.29, 30 We hypothesized that improved communication would result in lower expectations of benefit and severe side effects with treatment.4 Although we did not find that CONNECT lowered expectations of benefit from cancer treatments, patients in the intervention arms did report lower estimates of side effects (p=0.017 with experimental therapy, p=0.06 with standard therapy). The intervention may have improved a key aspect of cognitive–affective function, the confidence of patients to communicate concerns about side effects of treatment, resulting in greater discussion about this topic and perhaps reassurance that side effects would be manageable. Planned analysis of audio taped consultations will help elucidate the nature and implications of these findings.
Although the patients randomized to CONNECT reported that their treatment decisions were easier to reach and they were more satisfied with their treatment decisions, the intervention did not affect decisional conflict for the overall population. Insights into this finding are provided by our conceptual approach that emphasizes the unique cognitive-affective profiles of patient psychosocial subtypes. This approach is supported by our exploratory interaction analyses, which suggest that identifiable patient subgroups were more likely to benefit from CONNECT in terms of decision making. Patients with worse baseline quality of life appeared to benefit in specific decisional conflict domains; conversely, decisional conflict was increased by communication skills training in those patients who had better quality of life. Perhaps communication skills training is more likely to benefit those patients who are more focused on their quality of life, as this is a topic not commonly discussed with oncologists.4, 31, 32
The results of this study must be interpreted in the context of several potential limitations. The study sample was ethnically and racially homogeneous, predominantly drawn from large cancer centers. In addition, many eligible patients declined participation. Further study in other populations and community settings would aid in generalizability. As a web-based intervention, access was restricted to patients who either had personal internet access or were able to arrive early for their medical appointment. In an effort to maximize eligibility, CONNECT was developed for use with dial-up internet connections and did not require high speed internet access. As broadband internet access becomes more widely available, future interventions can be developed with more advanced video and interactive capabilities. Finally, it is plausible that patients randomized to the control condition explored the NCI website extensively, obtaining information about doctor-patient communication, and thus reducing the differences between study arms.
In conclusion, web-based communication skills training delivered before the initial oncology consultation can increase satisfaction with oncologist communication, influence expectations of benefit and toxicity from treatment, and improve treatment decision making. If the results of exploratory interaction analyses involving patient characteristics are confirmed, this would suggest avenues for future research with tailoring of communication aids such as CONNECT to the needs of individual patients.
Acknowledgments
Supported by R01 CA082085, P30 CA06927, and P30 CA43703 from the National Cancer Institute.
Footnotes
There are no financial disclosures from any of the authors.
References
- 1.Chan A, Woodruff RK. Communicating with patients with advanced cancer. J Palliat Care. 1997;13(3):29–33. [PubMed] [Google Scholar]
- 2.McCool J, Morris J. Focus of doctor-patient communication in follow-up consultations for patients treated surgically for colorectal cancer. J Manag Med. 1999;13(2–3):169–77. doi: 10.1108/02689239910292062. [DOI] [PubMed] [Google Scholar]
- 3.Quirt CF, Mackillop WJ, Ginsburg AD, et al. Do doctors know when their patients don't? A survey of doctor-patient communication in lung cancer. Lung Cancer. 1997;18(1):1–20. doi: 10.1016/s0169-5002(97)00048-2. [DOI] [PubMed] [Google Scholar]
- 4.Meropol NJ, Weinfurt KP, Burnett CB, et al. Perceptions of patients and physicians regarding phase I cancer clinical trials: implications for physician-patient communication. J Clin Oncol. 2003;21(13):2589–2596. doi: 10.1200/JCO.2003.10.072. [DOI] [PubMed] [Google Scholar]
- 5.Cheng JD, Hitt J, Koczwara B, et al. Impact of quality of life on patient expectations regarding phase I clinical trials. J Clin Oncol. 2000;18(2):421–428. doi: 10.1200/JCO.2000.18.2.421. [DOI] [PubMed] [Google Scholar]
- 6.Daugherty C, Ratain MJ, Grochowski E, et al. Perceptions of cancer patients and their physicians involved in phase I trials. J Clin Oncol. 1995;13(5):1062–1072. doi: 10.1200/JCO.1995.13.5.1062. [DOI] [PubMed] [Google Scholar]
- 7.Weinfurt KP, Sulmasy DP, Schulman KA, Meropol NJ. Patient expectations of benefit from phase I clinical trials: linguistic considerations in diagnosing a therapeutic misconception. Theor Med Bioeth. 2003;24(4):329–344. doi: 10.1023/a:1026072409595. [DOI] [PubMed] [Google Scholar]
- 8.Miller SM. Monitoring versus blunting styles of coping with cancer influence the information patients want and need about their disease. Implications for cancer screening and management. Cancer. 1995;76(2):167–177. doi: 10.1002/1097-0142(19950715)76:2<167::aid-cncr2820760203>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 9.Miller SM, Fang CY, Diefenbach MA, Bales CB. Tailoring psychosocial interventions to the individual's health information-processing style: The influence of monitoring versus blunting in cancer risk and disease. In: Baum A, Andersen BL, editors. Psychosocial interventions for cancer. Washington, DC: American Psychological Association; 2001. pp. 343–362. [Google Scholar]
- 10.Cegala DJ, McClure L, Marinelli TM, Post DM. The effects of communication skills training on patients' participation during medical interviews. Patient Educ Couns. 2000;41(2):209–222. doi: 10.1016/s0738-3991(00)00093-8. [DOI] [PubMed] [Google Scholar]
- 11.Cegala DJ, Post DM, McClure L. The effects of patient communication skills training on the discourse of older patients during a primary care interview. J Am Geriatr Soc. 2001;49(11):1505–1511. doi: 10.1046/j.1532-5415.2001.4911244.x. [DOI] [PubMed] [Google Scholar]
- 12.Fleisher L, Buzaglo J, Collins M, et al. Using health communication best practices to develop a web-based provider-patient communication aid: the CONNECT study. Patient Educ Couns. 2008;71(3):378–387. doi: 10.1016/j.pec.2008.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Meropol NJ, Egleston BL, Buzaglo JS, et al. Cancer patient preferences for quality and length of life. Cancer. 2008;113(12):3459–3466. doi: 10.1002/cncr.23968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Horowitz M, Wilner N, Alvarez W. Impact of Event Scale: a measure of subjective stress. Psychosom Med. 1979;41(3):209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Degner LF, Sloan JA. Decision making during serious illness: what role do patients really want to play? J Clin Epidemiol. 1992;45(9):941–950. doi: 10.1016/0895-4356(92)90110-9. [DOI] [PubMed] [Google Scholar]
- 16.Degner LF, Sloan JA, Venkatesh P. The Control Preferences Scale. Can J Nurs Res. 1997;29(3):21–43. [PubMed] [Google Scholar]
- 17.Gaskin DJ, Kong J, Meropol NJ, Yabroff KR, Weaver C, Schulman KA. Treatment choices by seriously ill patients: the Health Stock Risk Adjustment model. Med Decis Making. 1998;18(1):84–94. doi: 10.1177/0272989X9801800116. [DOI] [PubMed] [Google Scholar]
- 18.Gaskin DJ, Weinfurt KP, Castel LD, et al. An exploration of relative health stock in advanced cancer patients. Med Decis Making. 2004;24(6):614–624. doi: 10.1177/0272989X04271041. [DOI] [PubMed] [Google Scholar]
- 19.Buzaglo JS, Millard JL, Ridgway CG, et al. An Internet method to assess cancer patient information needs and enhance doctor-patient communication: a pilot study. J Cancer Educ. 2007;22(4):233–240. doi: 10.1007/BF03174122. [DOI] [PubMed] [Google Scholar]
- 20.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Medical Care. 1996;34(3):220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 21.O'Connor AM. Validation of a decisional conflict scale. Med Decis Making. 1995;15(1):25–30. doi: 10.1177/0272989X9501500105. [DOI] [PubMed] [Google Scholar]
- 22.Williams RL. A note on robust variance estimation for cluster-correlated data. Biometrics. 2000;56(2):645–666. doi: 10.1111/j.0006-341x.2000.00645.x. [DOI] [PubMed] [Google Scholar]
- 23.MacNeil B, Weichselbaum R, Pauker S. Speech and survival: tradeoffs between quality and quantity of life in laryngeal cancer. N Engl J Med. 1981;305(17):982–987. doi: 10.1056/NEJM198110223051704. [DOI] [PubMed] [Google Scholar]
- 24.Voogt E, van der Heide A, Rietjens J, et al. Attitudes of Patients with Incurable Cancer Toward Medical Treatment in the Last Phase of Life. Journal of Clinical Oncology. 2005;23(9):2012–2019. doi: 10.1200/JCO.2005.07.104. [DOI] [PubMed] [Google Scholar]
- 25.Cegala DJ. An exploration of factors promoting patient participation in primary care medical interviews. Health Commun. 2011;26(5):427–436. doi: 10.1080/10410236.2011.552482. [DOI] [PubMed] [Google Scholar]
- 26.Levinson W, Roter D. The effects of two continuing medical education programs on communication skills of practicing primary care physicians. J Gen Intern Med. 1993;8(6):318–324. doi: 10.1007/BF02600146. [DOI] [PubMed] [Google Scholar]
- 27.Fleissig A, Jenkins V, Fallowfield L. Results of an intervention study to improve communication about randomised clinical trials of cancer therapy. European Journal of Cancer. 2001;37:322–331. doi: 10.1016/s0959-8049(00)00415-9. [DOI] [PubMed] [Google Scholar]
- 28.Davis D, Thomson M, Oxman A, Haynes R. Changing Physician Performance: a Systematic Review of the Effect of Continuing Medical Education Strategies. JAMA. 1995;274(9):700–705. doi: 10.1001/jama.274.9.700. [DOI] [PubMed] [Google Scholar]
- 29.Horng S, Grady C. Misunderstanding in clinical research: distinguishing therapeutic misconception, therapeutic misestimation, and therapeutic optimism. IRB. 2003;25:6–11. [PubMed] [Google Scholar]
- 30.Weinfurt KP. Discursive versus information-processing perspectives on a bioethical problem: the case of 'unrealistic' expectations. Theory Psychol. 2004;14:191–203. [Google Scholar]
- 31.Street RL, Jr, Gordon HS, Ward MM, Krupat E, Kravitz RL. Patient participation in medical consultations: why some patients are more involved than others. Med Care. 2005;43(10):960–969. doi: 10.1097/01.mlr.0000178172.40344.70. [DOI] [PubMed] [Google Scholar]
- 32.Street RL, Jr, Richardson MN, Cox V, Suarez-Almazor ME. (Mis)understanding in patient-health care provider communication about total knee replacement. Arthritis Rheum. 2009;61(1):100–107. doi: 10.1002/art.24371. [DOI] [PubMed] [Google Scholar]