Abstract
Group B streptococci (GBS) birth canal colonisation in pregnant women and women of child-bearing age is well known. The recognition and incidence of infections caused by these organisms in non-pregnant and elderly adults are increasing. Clinical manifestations of GBS infections can range from simple skin and soft tissue infections to fatal meningitis in newborns. GBS as a cause of septic arthritis of the hip associated with pregnancy is previously unreported. We report a case of septic arthritis of the hip joint caused by GBS in a 30-year-old woman with a history of recent childbirth. Delay in recognition and lack of timely appropriate treatment of this condition henceforth led to severe destruction of the joint, requiring ultimate reconstruction of the joint with cemented total hip arthroplasty. This case report highlights the atypical presentation and rapidly destructive nature of this infection with catastrophic consequences.
Case presentation
A 30-year-old woman presented to her local accident and emergency (A&E) department with a 5-week history of worsening left hip pain. She gave a history of childbirth 2 days prior to the onset of pain. Delivery had been via the vaginal route with the legs positioned in stirrups. She had sustained a perineal tear which was repaired with multiple sutures. During the 5-week period of pain, she sought advice from her family doctor, but no further investigations were carried out and she was referred for physiotherapy. At this time, she did not show any typical signs of infection such as redness, swelling or fever. Having had no benefit from physiotherapy and deteriorating hip pain, she presented to the local A&E department. Her white blood cell (WBC) count and inflammatory markers including erythrocyte sedimentation rate (ESR) and C reactive protein (CRP) were markedly elevated. Her hip radiograph showed signs of joint destruction and chondrolysis (figure 1). She was provisionally diagnosed with septic arthritis of the left hip. She was referred to our unit for further management. She was transferred immediately and, on admission, she was found to have fever with severe restriction of hip movements. Treatment options were either open joint or arthroscopic debridement and lavage, urgently and in a timely manner. She underwent arthroscopic debridement of the hip joint by the senior author, who has a special interest in hip arthroscopy, at our institution the same day. Blood-stained turbid pus was aspirated on entering the left hip joint, which was sent for microbiology, and the tissue specimen was sent for histology. Arthroscopic findings revealed complete destruction of the acetabular cartilage down to the cortical bone and mixed lesions of destroyed and preserved areas on the femoral head.
Figure 1.
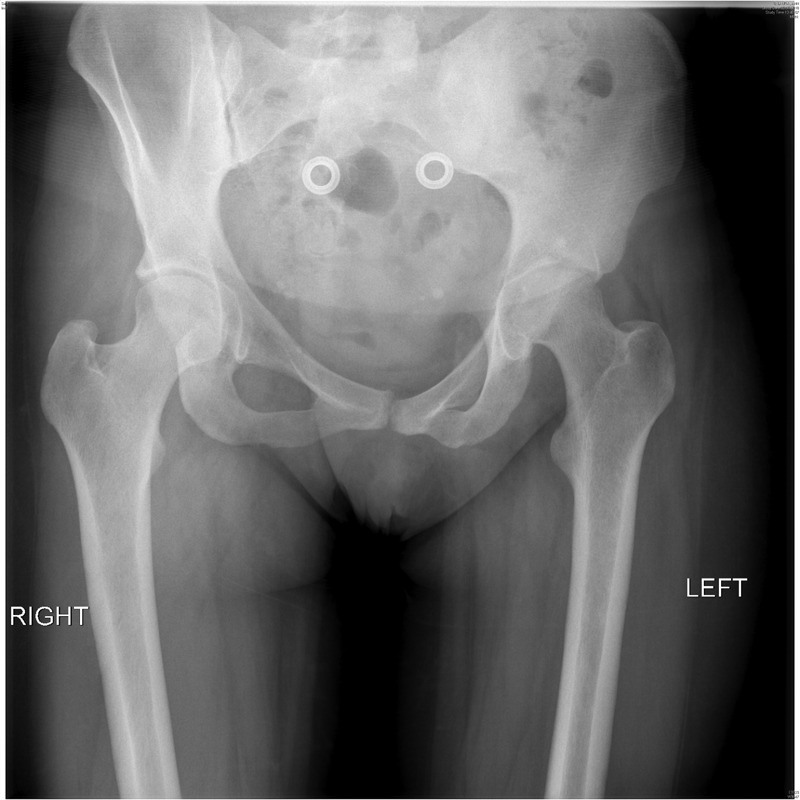
Pelvis radiograph at presentation. Left hip joint shows joint space reduction and evidence of chondrolysis.
Microscopic analysis of the obtained joint fluid showed Gram-positive cocci and markedly raised WBC count and red blood cell (RBC) count (ie, WBC 150/mm3, RBC >500). Culture of the aspirate grew group B streptococci (GBS), which was found to be sensitive to penicillin and erythromycin. Neonatal and gynaecological advice was sought immediately with regard to the screening mother and child for GBS. As the child had been fit and healthy since birth, no further action was deemed necessary. Vaginal swabs were advised from the mother, but these showed only heavy growth of commensal flora. Histological analysis showed fibrous tissue with numerous acute inflammatory cells compatible with septic arthritis.
The acute symptoms resolved significantly following surgery and a subsequent 2 weeks of intravenous antibiotics. She mobilised well, touch-weight bearing with adequate pain relief. She was advised touch-to-partial weight bearing in order to prevent further damage to the remaining articular cartilage. She was discharged home after conversion to oral antibiotics (amoxicillin and clindamycin), which were continued for 4 weeks. Repeat blood tests before discharge showed a downward trend with ESR at 84 and CRP at 34.
On outpatient review at 6 weeks, she was making good progress and mobilising with two crutches. She was wean off tramadol and was advised to full-weight bear as able and comfortable. Radiograph of her hip showed no further deterioration. Fortunately, she suffered no immediate or early complications.
She was seen again at 3 months postsurgery. Though she was not requiring painkillers, she was having difficulty in mobilising. Henceforth, she was unable to come off crutches. Blood tests were performed at this visit which showed a downward trend (ESR 17 and CRP 3).
At 4 months’ clinical follow-up, she complained of continued difficulty with mobilisation and reliance on crutches. Her pain was tolerable; however, her function was very poor. Her other concern was not being able to interact with her growing child. At this stage, along with her family, she expressed a strong desire to undergo hip replacement with the expectation of pain relief, improved mobility and better quality of life. Blood tests done on this visit showed ESR and CRP within normal limits (ESR 9 and CRP 2). Radiograph showed further deterioration (figure 2).
Figure 2.
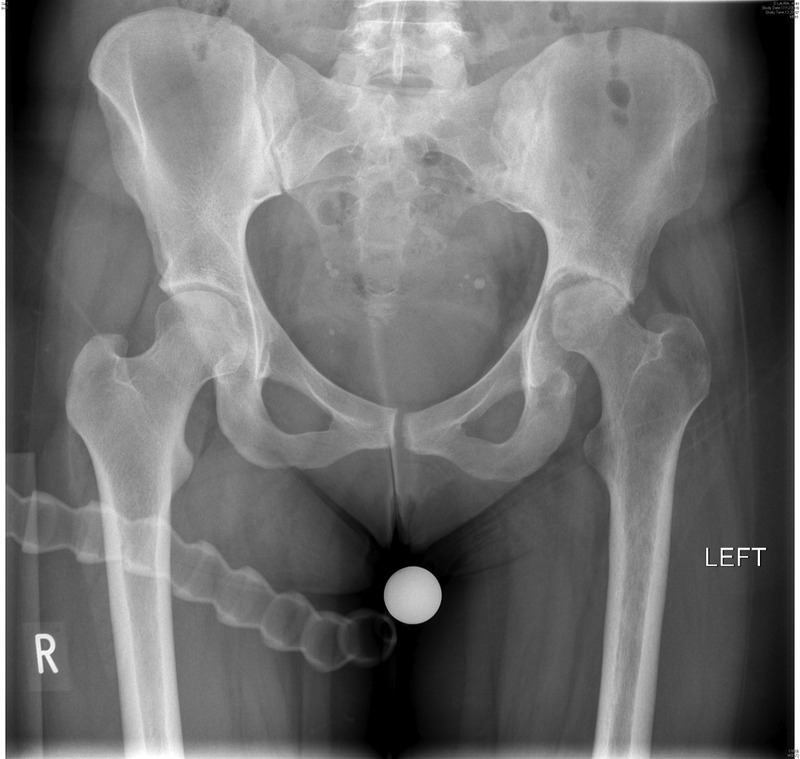
Preoperative pelvis radiograph at 4 months follow-up showed significant joint destruction with loss of substance and proximal migration of the femoral head.
After 6 months, she underwent a WBC bone scan which showed no evidence of infection.
Investigations
Haematology—full blood count/ESR
Biochemistry—CRP
Plain radiographs
Bone scan.
Treatment
Total hip replacement
She subsequently underwent cemented left total hip replacement with impaction bone grafting using fresh-frozen femoral allograft. The procedure was performed through posterior approach in the lateral position. The femoral head was found to have undergone significant destruction and the acetabulum was expanded and filled with dense fibrous tissue. The acetabular bone loss was such that impaction bone grafting was required to reconstruct the defects.
The acetabulum was reconstructed with a cross-linked ultra-high-molecular weight polyethylene socket (Marathon; XL-UHMWPE) and femur with C -Stem–AMT stem (12/14 taper: DePuy International Ltd, Leeds, UK). Both the components were fixed in using bone cement laden with gentamicin 1 g per 40 g cement). A 28 mm ceramic head was used to achieve ceramic on polyethylene-bearing surfaces (figure 3).
Figure 3.
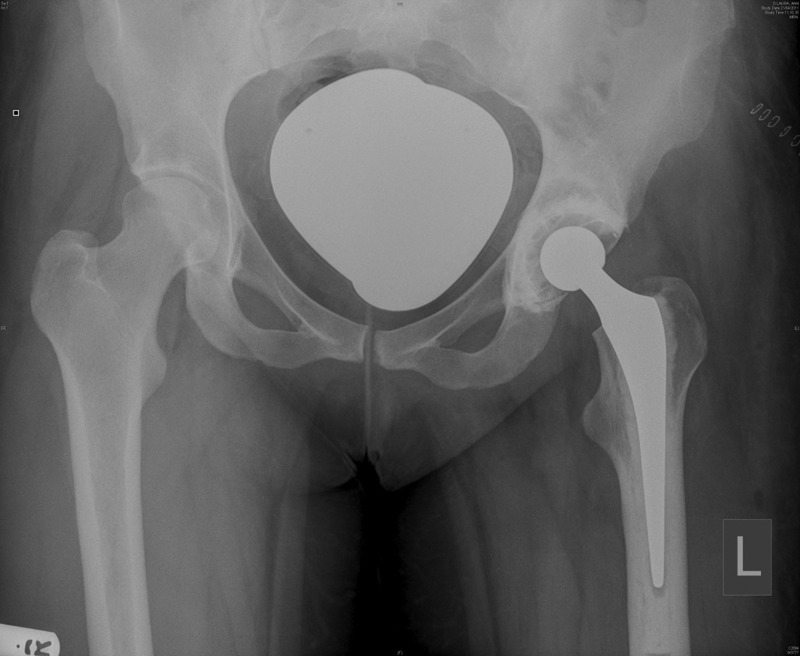
Postoperative radiograph showing cemented total hip replacement with impaction bone grafting to the acetabulum. Bearing surface 28 mm ceramic head on the polyethylene socket.
She was discharged home after 3–4 days of routine hospital stay with full weight bearing as tolerated without any immediate complication. She had a routine three doses of cefuroxime postoperatively.
She was seen in the follow-up clinic post hip replacement at 6 weeks and 3 months and was doing very well. She reported no pain and had better mobility and quality of life. We gauged this by the patient's reported outcome measures. We used the University of California Los Angeles (UCLA) activity scale and Oxford hip score (OHS) as outcome measurement tools. Her preoperative UCLA score was 3 and OHS was 29. At 6 weeks, her UCLA score improved to 6 and OHS improved to 46. She was clinically followed up at 18 months. She reported no problems and was delighted with the outcome overall.
Urgent—Arthroscopic debridement and lavage.
Definitive—Cemented total hip replacement.
Outcome and follow-up
Very good.
18 months—the patient was delighted with the outcome.
Discussion
Septic arthritis due to GBS is not a common diagnosis. To our knowledge, infection of the hip joint by this organism with such devastating consequences necessitating total hip replacement has not been reported previously. GBS is mainly known for colonisation and bacteraemia in newborns,4 pregnant women and the elderly and in immunocompromised adults. In the USA, 2 out of every 1000 newborns are affected by GBS sepsis.1 In an effort to decrease the incidence of neonatal GBS infection, the Centers for Disease Control and Prevention have established guidelines for screening and treatment during pregnancy. No such screening programmes currently exist in the UK.2
This report highlights that GBS septic arthritis can be associated with childbirth in healthy adults. The clinical presentation can be subtle and the patient may not be unwell, but the sequel can be quite devastating5. In the case presented here, we hypothesise the following sequence of events: perineal tear in an area of GBS colonisation led to bacteraemia, which led to septic arthritis of the hip joint with rapid destruction of the joint due to delay in diagnosis.
If the joint is destroyed to the point where it is not possible to salvage and hip replacement is required, then a cemented type of total hip replacement should be considered as this allows the addition of extra antibiotics to the cement.
Learning points.
This case report highlights that the maternal consequences of group B streptococci (GBS) infection can be serious and life-changing.
Though muscular aches and joint pains are common in pregnancy, there should be a high index of suspicion for GBS septic arthritis, especially in cases of persistent symptoms.
Such cases with strong clinical suspicion should be thoroughly investigated and referred early to the specialist's centre for specialist intervention if required.
Clear guidelines for screening GBS carriers should be formulated and treated accordingly.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Quinlan J, Hill D, Maxwell B, et al. The necessity of both anorectal and vaginal cultures for group B streptococcus screening during pregnancy. J Fam Pract 2000;49:447–8 [PubMed] [Google Scholar]
- 2. http://www.rcog.org.uk/womens-health/clinical-guidance/preventing-group-b-streptococcus-gbs-infection-newborn-babies (accessed 14 Jan 2013)
- 3.Laster A, Michels M. Group B streptococcal arthritis in adults. Am J Med 1984;76:910–5 [DOI] [PubMed] [Google Scholar]
- 4.Straus C, Caplanne D, Bergemer A, et al. Destructive polyarthritis due to a group B streptococcus. Revue Rheumatisme 1997;64:339–41 [PubMed] [Google Scholar]


