Abstract
Alcohol problems may impede adaptive, proactive responses to disaster-related injury and loss, thus prolonging the adverse impact of disasters on mental health. Previous work suggests that veterans of the U.S. armed forces have a relatively high prevalence of alcohol misuse and other psychiatric disorders. This is the first study to estimate the impact of pre-disaster alcohol problems on post-disaster depressed mood among veterans, using data that were collected before and after the 1994 Northridge, California earthquake. We assessed the impact of alcohol problems on post-disaster depressed mood in an existing clinical cohort of veterans who experienced the 6.7-magnitude earthquake that struck Northridge in January 1994. One-to-three months after the disaster, interviewers contacted participants by telephone to administer a follow-up questionnaire based on a survey that had been done pre-earthquake. Post-earthquake data were obtained on 1144 male veterans for whom there were pre-earthquake data. We tested a predictive path model of the relationships between latent variables for pre-disaster alcohol problems, functional limitations, and depressed mood on latent variables representing post-disaster “quake impact” and depressive mood. Results showed that veterans who had more alcohol problems before the earthquake experienced more earthquake-related harms and severely depressed mood after the earthquake, compared with those who had fewer alcohol problems. Programs serving veterans with a high prevalence of alcohol problems should consider designing disaster response protocols to locate and assist these patients in the aftermath of disasters.
Keywords: alcohol, disasters, mental health, structural equation modeling, longitudinal studies
Human vulnerability to the harms resulting from earthquakes, large-scale industrial accidents, and other disasters depends not only on proximity to the source or physical nature of a hazard, but also on the pre-existing health and socioeconomic characteristics of the affected population (Enarson, 2007). Among veterans of the U.S. armed forces who depend on service providers in the Veterans Health Administration (VHA), combat-related disabilities, complex chronic medical conditions, and generally advanced age may amplify the risk of harm resulting from disasters. In January 1994, a 6.7-magnitude earthquake struck Northridge, California, a suburb approximately 25 miles north of downtown Los Angeles. Irreparable damage to the Sepulveda Veterans Health Administration Medical Center (VAMC) – situated within 2 miles of the quake’s epicenter – represented a loss of critical healthcare infrastructure for a large local population of predominantly older veterans with multiple chronic illnesses and varying degrees of functional impairment.
Alcohol misuse is often associated with impairments in physical, mental, and social functioning (Foster, Powell, Marshall, & Peters, 1999; Okoro et al., 2004; Stranges et al., 2006), and may increase the vulnerability of veterans to the harms of disasters and public health emergencies. Previous quantitative research on alcohol misuse and post-disaster mental health has generally not focused on veterans. Further, work in this area has rarely included any data collected pre-disaster, relying instead on participant recall of pre-disaster behavior (DiMaggio, Galea, & Guohua, 2009; Moore, Cunradi, & Ames, 2004; North, Ringwalt, Downs, Derzon, & Galvin, 2011). We know of two longitudinal disaster studies – both on the September 11 attacks – that included self-reported pre/post-disaster data on substance use and mental health symptoms. Exposure to the attacks for both study samples was relatively vicarious and remote, insofar as participants lived at great geographic distances from the epicenter of the disaster, in states outside of New York. Perrine and colleagues (Perrine, Schroder, Forester, McGonagle-Moulton, & Huessy, 2004) analyzed approximately 12 months of data on alcohol use and single-item measures of mood that were collected on a daily basis via interactive response devices from 84 Vermont residents, as part of a substance abuse study that had begun approximately one year before 9/11. Alcohol use increased significantly among women only on the day of the attacks; however, increases in global measures of stress, anger, and sadness persisted among both men and women for as long as 70 days. Similarly, an analysis of longitudinal questionnaire data collected from the faculty, staff, and students of a Midwestern university found that average alcohol use increased slightly among women, but not men, after 9/11 (Richman, Wislar, Flaherty, Fendrich, & Rospenda, 2004).
Only two studies using pre/post-disaster data have estimated the impact of disasters on the mental health of veterans (Dobalian et al., 2011; Rosenheck, 2002) despite the high prevalence of mental health problems among subgroups of this population, such as those of the post-Vietnam era (Norquist, Hough, Golding, & Escobar, 1990) and those exposed to combat (Autor, Duggan, & Lyle, 2011). Rosenheck (2002) analyzed administrative data from VHA facilities in New York and found negligible differences in the use of mental health and substance abuse services before and after the 9/11 attacks. By contrast, results from an analysis of longitudinal data collected from veterans living near the epicenter of the 1994 Northridge earthquake suggest that the disaster did indeed contribute to decrements in mental health (Dobalian et al., 2011). In additional to its longitudinal design and pre/post disaster measures, a major strength of the latter study was its use of validated survey instruments rather than administrative data; however, the analysis did not include measures of substance use.
Alcohol problems have often been conceptualized as self-medication for post-disaster symptoms of depression and anxiety (North, Ringwalt, Downs, Derzon, & Galvin, 2011); however, it is also possible that pre-disaster alcohol problems are a risk factor for post-disaster exacerbations of these disorders. To our knowledge, no prospective cohort studies have examined alcohol problems as an independent risk factor predicting post-disaster depressive symptoms in a clinical population of veterans. To address this gap in the relatively small empirical literature, we analyzed pre/post-disaster data collected from 1,144 veterans living in the vicinity of the epicenter of the 1994 Northridge earthquake.
Method
Participants and procedures
Before the Northridge earthquake of January 1994, the Primary Ambulatory Care and Education (PACE) program provided integrated care to more than 19,000 veterans from a catchment area around the Sepulveda VAMC, which was two miles from the epicenter of the earthquake. Immediately after the earthquake, PACE program evaluators developed a survey to assess the impact of the earthquake on veterans who received care at the Sepulveda location, and to disseminate information on how to obtain assistance from the VAMC or other agencies. The post-earthquake structured interview was conducted over the telephone with a sample of veterans who had participated in a clinic-based evaluation of the PACE program approximately 1.5 years before the earthquake (March-June 1992). As part of this pre-earthquake program evaluation, patients were approached consecutively at the check-in desks of the PACE program clinics at randomly selected days and times. Eligible individuals participated in a structured face-to-face interview about their service utilization, socio-demographic characteristics, and health status. The 1800 individuals who participated in the pre-earthquake program evaluation were a subgroup of approximately 11,000 patients who participated in the PACE program during 1992. Post-earthquake survey data were obtained on 1144 veterans (64% of the original sample). Participants were recruited for the pre-earthquake survey if they were English-speaking male veterans who had at least one prior Sepulveda VA clinic visit in the previous 12 months (Lee et al., 2002), excluding those who were hearing impaired, in acute distress, showed signs of memory loss at enrollment, or homeless.
Measures
The analysis included several pre-earthquake variables that address the concept of social vulnerability, i.e. the view that certain groups – such as the elderly, the poor, and those with functional limitations – have relatively fewer defenses against the harms of disasters (Enarson, 2007). Two pre-disaster socioeconomic status (SES) measures, education and income, were used as indicators of a latent variable, SES. Education was measured on a 1–13 scale ranging from 1=no formal school to 13=post-graduate work. Income was assessed as yearly household income (1=less than $15,000; 2=$15,000 to less than $30,000; 3=$30,000 or more). Age was also included as an observed variable. Marital status, ethnicity, and employment status were tested as possible predictors, but were not associated with any of the mediators or outcome variables, and were not retained in the final model.
Functional Limitations (pre-disaster) were assessed with the 13-item Beth Israel/UCLA Functional Status Questionnaire (FSQ), (Jeete et al., 1986) which measures activities of daily living and social activities (coefficient alpha =.95). Typical items included “moving out of a bed or chair,” and “walking several blocks.” Because using 13 indicators for 1 latent variable would have been cumbersome, items were combined at random into 4 parcels as indicators of a Functional Limitations latent variable. Parceling is acceptable, especially when coefficient alpha is high, as it was in this case (Yuan, Bentler, & Kano, 1997).
Alcohol Problems (pre-disaster) are a latent variable indicated by the following 5 yes/no items (coefficient alpha =.74), the first four of which comprise the CAGE screener (Ewing, 1984): (1) Do you ever feel the need to cut down on your drinking? (2) Does it make you mad when someone complains about your drinking? (3) Do you ever feel guilty about your drinking? (4) Do you ever take a morning eye-opener? and (5) During the past year, has a VA doctor, nurse, or other health care person told you that you should drink less?
Depressed Mood (pre-disaster) is a latent variable measured by the RAND Mental Health Index (MHI), a 5-item subscale (coefficient alpha =.87) of the RAND Short Form (SF)-36 questionnaire that assesses mood in the previous 4 weeks (Cuijpers, Smits, Donker, ten Have, & de Graaf, 2009; Rumpf, Meyer, Hapke, & John, 2001; Ware & Sherbourne, 1992). Scores range from 1 (all of the time) to 6 (none of the time) and were reverse-scored so that higher scores indicated more severe symptoms. Typical items included: “I was downhearted and blue,” and “I was a happy person.” This scale has demonstrated good psychometric properties in previous studies (Berwick et al., 1991; Friedman, Heisel, & Delavan, 2005; McCabe, Thomas, Brazier, & Coleman, 1996; Means-Christensen, Arnau, Tonidandel, Bramson, & Meagher 2005; van Leeuwen, van der Woude, & Post, 2012;).
The analysis included a measure of Quake Impact (post-disaster) to capture important global information on the effect of the earthquake on daily functioning and well-being, from the perspective of the patient. Quake Impact is a latent variable composed of 3 indicators. The first item assessed the degree to which “things had changed” for participants since the earthquake (1=not at all; 2=very little;3=somewhat;4=very much). The other 2 items were dichotomous (1=no, 2=yes) and assessed if participants had experienced earthquake-related pain for at least 2 days, or severe mental and emotional stress for 2 weeks or more (coefficient alpha =.57).
Depressed Mood (post-disaster outcome variable): Participants were administered the MHI again after the earthquake. Responses to the same 5 items were used as indicators of a post-disaster Depressed Mood latent variable (coefficient alpha =.86).
Statistical analyses
Data were analyzed with the EQS structural equation modeling (SEM) program (Bentler, 2006). Goodness-of-fit was assessed using the comparative fit index (CFI), the maximum likelihood chi-square (ML χ2), and the Root Mean Square Error of Approximation (RMSEA); CFI values of .95 or greater indicate good fit. Because the multivariate kurtosis estimate was high in these data (Mardia’s normalized estimate =113.14), we also report robust statistics: the Satorra-Bentler chi-square (S-B χ2) and the Robust CFI (RCFI), which correct for multivariate non-normality. The RMSEA is a measure of lack of fit per degrees of freedom controlling for sample size, with values less than .06 indicating good fit.
An initial confirmatory factor analysis (CFA) was performed with each hypothesized latent construct predicting its proposed manifest indicators. This analysis assessed the adequacy of the proposed factor structure and the relationships among the latent and single-item variables. Once the factor structure was confirmed, we tested a predictive latent variable path model in which age and SES predicted pre-disaster Alcohol Problems, Depressed Mood, and Functional Limitations. These latter three latent variables predicted Quake Impact, which in turn predicted post-disaster Depressed Mood. Due to stability effects, pre-disaster Depressed Mood was expected to predict post-disaster Depressed Mood. Nonsignificant paths and covariances were trimmed from the model. We allowed some correlated error residuals between similar items in Depressed Mood at the two time points (e.g. “I have been a very nervous person”) to account for stable response tendencies and improve model fit. We also examined indirect effects to assess the impact of the three intermediate predictors on post-disaster Depressed Mood as well as effects of demographics on Quake Impact.
Results
As shown in Table 1, the average age of participants was 60.8 years. The sample was 77% White, 7% African-American, 6% Hispanic, and 10% Native American, Asian, or other backgrounds. Twenty-seven percent had completed 12th grade, 20% had 2 years of college, 13% had completed 4 years of college, and 14% had not completed high school. Mean values for the Depressed Mood items were higher post-earthquake than they were pre-earthquake.
Table 1.
Summary statistics and factor loadings in confirmatory factor analysis for 1144 veterans (All factor loadings significant, p ≤.001.)
| Variables (range) | Mean | SD | Factor Loading |
|---|---|---|---|
| Demographics | |||
| Age (22–90 years) | 60.84 | 12.54 | ——— |
| SES | |||
| Education (range, 1–13 years) | 7.90 | 2.80 | .38 |
| Income (range, 1–3) | 1.51 | 0.69 | .53 |
| Pre-Earthquake | |||
| Depressed Mood a | |||
| Nervous | 2.19 | 1.36 | .71 |
| Calm b | 2.83 | 1.38 | .80 |
| Blue | 1.99 | 1.23 | .75 |
| Happy b | 2.60 | 1.36 | .74 |
| In the dumps | 1.51 | 1.02 | .67 |
| Alcohol Problems, past 12 months c | |||
| Feel the need to cut down on drinking | 0.11 | 0.32 | .72 |
| Make you mad if someone complains | 0.04 | 0.20 | .58 |
| Feel guilty about your drinking | 0.06 | 0.23 | .68 |
| Take a morning eye-opener | 0.04 | 0.19 | .50 |
| Health care person said should drink less | 0.06 | 0.24 | .57 |
| Functional Limitations (1–5) | |||
| Composite 1 | 1.46 | 0.61 | .90 |
| Composite 2 | 1.42 | 0.66 | .89 |
| Composite 3 | 1.42 | 0.68 | .84 |
| Composite 4 | 1.72 | 0.83 | .80 |
| Post-Earthquake | ——— | ||
| Quake Impact | |||
| Changes after earthquake (1–4) | 2.28 | 1.15 | .61 |
| Pain (1–2) | 1.13 | 0.33 | .39 |
| Severe stress for 2 weeks (1–2) | 1.27 | 0.44 | .70 |
| Depressed Mood (1–6) | |||
| Nervous | 2.47 | 1.63 | .81 |
| Calm a | 3.00 | 1.53 | .76 |
| Blue | 2.19 | 1.40 | .75 |
| Happy a | 2.76 | 1.40 | .71 |
| In the dumps | 1.67 | 1.20 | .65 |
Item scores range 1–6;
Reverse-scored in analysis.
Coded 0 = no, 1 = yes.
Confirmatory factor analysis
Table 1 reports the means, standard deviations, ranges, and factor loadings for each measured variable. All factor loadings were significant (p<.001). Fit indexes were very good: ML χ2 =674.17, 250 df; CFI =.95, RMSEA =.04; S-B χ2 =558.97, 250 df; Robust CFI =.95, RMSEA =.04.
Table 2 reports the bivariate correlations among constructs of the model. Older participants reported lower pre-disaster Depressed Mood, more Functional Limitations, less Quake Impact, and lower post-disaster Depressed Mood. Higher SES was associated with fewer Alcohol Problems, fewer Functional Limitations, and less severe Depressed Mood both pre- and post-earthquake. Alcohol Problems were associated with pre-disaster Depressed Mood, more Quake Impact and, as expected, greater post-disaster Depressed Mood. Functional Limitations were associated with more Quake Impact and more post-disaster Depressed Mood. Quake impact was highly associated with post-disaster Depressed Mood (.76).
Table 2.
Correlations among variables in the predictive model of post-earthquake Depressed Mood (n=1144)
| Variables | |||||||
|---|---|---|---|---|---|---|---|
| Pre-Earthquake | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
| 1. Age | -- | ||||||
| 2. SES | −.10a | -- | |||||
| 3. Depressed Mood | −.14c | −.21 c | -- | ||||
| 4. Alcohol Problems | −.11c | −.17c | .18 c | -- | |||
| 5. Functional Limitations | .10b | −.17 c | .31c | .04 | -- | ||
| Post-Earthquake | |||||||
| 6. Quake Impact | −.21c | −.06 | .34c | .17c | .22c | -- | |
| 7. Depressed Mood | −.12c | −.16 b | .61c | .16c | .25c | .76c | -- |
p<.05.
p<.01.
p < 001.
Mediated path model
The final predictive SEM is presented in Figure 1. As with the CFA model, fit indexes were acceptable: ML χ2 =709.06, 256 df; CFI =.95, RMSEA =.04; S-B χ2 =574.49, 256 df; RCFI =.95, RMSEA =.04. Age and SES significantly predicted pre-disaster Alcohol Problems, Depressed Mood, and Functional Limitations – all three of which, in turn, predicted Quake Impact. Post-disaster Depressed Mood was predicted by pre-disaster Depressed Mood as expected, and by Quake Impact. Notably, the coefficient for the predictive path from Quake Impact to post-disaster Depressed Mood was larger than the stability coefficient from the pre-disaster Depressed Mood (.62 vs. .40). Through the three intermediate health variables, there were significant effects of lower SES and younger age on greater Quake Impact (p<.001 for both). Through Quake Impact, post-disaster Depressed Mood were indirectly influenced by pre-disaster Depressed Mood (p<.001), younger age (p<.001), lower SES (p<.001), Alcohol Problems (p<.01), and Functional Limitations (p<.01). The model explained 71% of the variance in post-disaster Depressed Mood.
Figure 1.
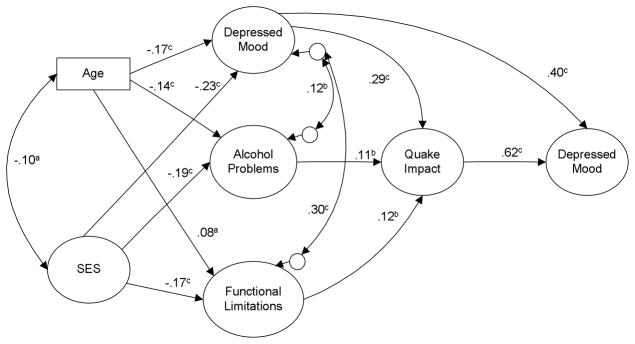
Structural equation model with significant regression paths assessing impact of pre-disaster characteristics and earthquake-related variables on post-disaster depressed mood at follow-up (N = 1144 veterans). Large circles represent latent variables; rectangles represent single items. Single-headed arrows represent regression coefficients; two-headed arrows represent correlations. Regression coefficients are standardized (a = p<.05, b = p<.01, c = p<.001).
Discussion
This study estimated the prospective association of Alcohol Problems with post-disaster Depressed Mood, as mediated by the impact of the Northridge earthquake, in a clinical cohort of U.S. veterans. The key finding is consistent with those of a previous analysis of longitudinal data showing increases in global, single-item ratings of stress, anger, and sadness among 84 problem drinkers several weeks after 9/11 (Perrine et al., 2004). With the substantially larger sample size in the current study, SEM allowed us to examine relationships among both pre- and post-disaster variables. Mediated through Quake Impact, Alcohol Problems were associated with post-disaster Depressed Mood, over and above their association with pre-disaster Depressed Mood and the stability of Depressed Mood over time.
Affecting virtually every organ system in the body, Alcohol Problems could increase the risks of post-disaster Quake Impact and Depressed Mood in a number of ways. Chronic alcohol abuse impairs cognitive functioning and psychomotor skills that would be critical in emergency situations (Brick, 2008), interfering with the ability to assess danger accurately, evacuate built structures expeditiously, and access needed recovery assistance. The generalized skeletal fragility seen in some people with alcohol dependence, particularly the elderly, may also increase the risk of injuries in the wake of a major disaster such as an earthquake (NIAAA, 2000). Further, Alcohol Problems could impede adaptive, proactive responses to injury and loss, potentially exacerbating and prolonging the adverse impact of the earthquake on Depressed Mood. These relationships between pre-disaster Alcohol Problems and post-disaster Quake Impact and Depressed Mood should be noted by VHA service providers and administrators who are charged with emergency management responsibilities. Just as they would for any other chronically ill patient group, VHA personnel whose caseloads include a high prevalence of clients with alcohol problems should consider creating disaster response protocols for locating and assisting these patients in the aftermath of disasters.
Through their association with pre-disaster Alcohol Problems, Functional Limitations and Depressed Mood, there were significant indirect effects of age and SES on Quake Impact and post-disaster Depressed Mood. These relationships have not been described in previous longitudinal work on substance abuse and disasters. In their study of the impact of 9/11, Richman and colleagues (Richman et al., 2004) included age and education in their multivariate analyses, but did not provide results for these variables in their report; the other two longitudinal analyses of pre/post-disaster measures of which we are aware did not include adjustments for demographic or socioeconomic characteristics (Perrine et al., 2004; Rosenheck, 2002). In the current sample, higher SES was negatively associated with the pre-disaster variables on Alcohol Problems, Depressed Mood, and Functional Limitations, perhaps reflecting a greater capacity and set of socioeconomic resources for coping with the physical and mental toll of military service (Autor et al., 2011). Older age had a negative association with Alcohol Problems and pre-disaster Depressed Mood. Previous work has reported that post-Vietnam era veterans – but not older Vietnam, Korean, and World War II veterans – had a higher lifetime prevalence of substance use and other psychiatric disorders than did age-matched non-veteran men (Norquist et al., 1990). The association of younger age with Alcohol Problems and Depressed Mood may reflect differences between those who were drafted into the military (i.e. Vietnam and before) versus those who self-selected for service after the U.S. moved to an all volunteer force in 1973 (Rosenheck, 2006). Alternatively, the negative association between older age and Alcohol Problems is consistent with a “maturing out” (Dawson et al., 2005) hypothesis that the responsibilities of civilian work and family roles (which generally increase with age) entail a decrease in problematic alcohol use.
The impact of disasters on people with pre-existing functional limitations has received little attention in previous research. In a cross-sectional study of individuals who sought mental health treatment after the 1995 Oklahoma City bombing, a functional impairment measure asking participants if they “had a lot of trouble doing things” was associated with alcohol use (Pfefferbaum & Doughty, 2001). Alcohol Problems were not associated with Functional Limitations in the current sample, probably because these limitations were more common among older veterans (who had fewer Alcohol Problems). The finding that age predicted Quake Impact through Alcohol Problems is relevant for developing disaster response interventions, because assistance that targets veterans on the basis of age rather than alcohol problems is likely to be implemented more readily in the aftermath of a disaster.
This study has several limitations. Although the CAGE Alcohol Problems questionnaire has been widely used by others (Ewing, 1984), it is important to note that the measure did not have the rigor of a diagnosis; however, isolated symptoms or subsyndromal conditions are often clinically relevant, particularly if a person’s cognitive or functional status is already compromised due to other comorbid medical problems (Kavanagh & Connolly, 2009). The low alpha for the Quake Impact items is a concern. This measure was developed for an extremely time-sensitive needs assessment, in the aftermath of one of the most costly natural disasters in U.S. history. Because of the emergent nature of the context in which the survey was implemented, we do not have previous information on the validity of the items. Future work to further evaluate the psychometric properties of the Quake Impact measure is needed. The prospective study design lends credibility to the hypothesis that Alcohol Problems influenced post-disaster Depressed Mood, but there is still the possibility of reciprocity among measures taken at the same time point. Pre-disaster, the characteristics represented by Alcohol Problems, Depressed Mood, and Functional Limitations may have affected the earning power or educational potential of participants (as represented by the SES variable). Post-disaster, it is possible that there were participants whose reports of Quake Impact were unduly influenced by the greater Depressed Mood they were experiencing at the time. A final limitation is that this sample did not include women, who now represent approximately 8% of the veteran population (U.S. Department of Veterans Affairs, 2012). Most population prevalence studies have shown greater use of alcohol by men than women (Wilsnack, Vogeltanz, Wilsnack, & Harris, 2000). Although having a sample consisting entirely of men might be advantageous for studying alcohol abuse symptoms, future disaster research on veterans should include more women.
The association between Alcohol Problems and Quake Impact was significant, but of considerably lower magnitude that the association between pre- and post-disaster Depressed Mood. Nevertheless, these findings on the prospective association of Alcohol Problems with Quake Impact and Depressed Mood suggest a number of directions for future work in this area, particularly to identify the mechanisms by which alcohol would have such effects. Opportunities to conduct prospective cohort studies with pre/post-disaster measures are admittedly rare; however, the VHA continuously stores longitudinal data on utilization and various clinical parameters that may permit retrospective cohort studies of the impacts of disasters. A core mission of the VHA concerns disaster and emergency response for veterans and the general population, and states that the VHA will provide support to communities following major disasters (Bascetta, 2001). In fact, the VHA has directly provided care for veterans — and sometimes non-veterans — during every presidentially declared national disaster since 1992. The development and evaluation of emergency and disaster response protocols are a key focus of the Veterans Emergency Management Evaluation Center (VEMEC). The extensive administrative and clinical data system that the VHA maintains in providing care for veterans could conceivably function as a population-based registry in the event of a disaster. Using diagnostic, geographic (home residence), and demographic data fields, subgroups of veterans with special needs living in close proximity to hazardous areas could be identified and contacted as appropriate for post-disaster needs assessments. Given the medical and social challenges faced by many U.S. veterans on a daily basis, research and evaluation to improve the responsiveness of disaster relief services for this population are crucial.
Acknowledgments
Support for this research was provided by the Department of Veterans Affairs, Veterans Health Administration, Office of Public Health and Environmental Hazards and the Department of Veterans Affairs, Western Region and grant P01-DA01070-37 from the National Institute on Drug Abuse.
Contributor Information
Kevin C. Heslin, Veterans Emergency Management Evaluation Center, 16111 Plummer St. (152), North Hills, CA 91343-2036
Judith A. Stein, Department of Psychology, University of California, Los Angeles
Aram Dobalian, Veterans Emergency Management Evaluation Center, Veterans Health Administration, North Hills, CA, USA.
Barbara Simon, Center for the Study of Healthcare Provider Behavior, Veterans Health Administration, North Hills, CA, USA.
Andrew B. Lanto, Center for the Study of Healthcare Provider Behavior, Veterans Health Administration, North Hills, CA, USA
Elizabeth M. Yano, Center for the Study of Healthcare Provider Behavior, Veterans Health Administration, North Hills, CA, USA
Lisa V. Rubenstein, Center for the Study of Healthcare Provider Behavior, Veterans Health Administration, North Hills, CA, USA
References
- Autor DH, Duggan MG, Lyle DS. Battle scars? The puzzling decline in employment and rise in disability receipt among Vietnam era veterans. American Economic Review. 2011;101:339–344. [Google Scholar]
- Bentler PM. EQS 6 structural equations program manual. Encino, CA: Multivariate Software, Inc; 2006. [Google Scholar]
- Berwick DM, Murphy JM, Goldman PA, Ware JE, Jr, Barsky AJ, Weinstein MC. Performance of a five-item mental health screening test. Medical Care. 199;29(2):169–76. doi: 10.1097/00005650-199102000-00008. [DOI] [PubMed] [Google Scholar]
- Brick J. Medical consequences of acute and chronic alcohol abuse. In: Brick J, editor. Handbook of the Medical Consequences of Alcohol and Drug Abuse. New York: Routledge; 2008. pp. 9–56. [Google Scholar]
- Cuijpers P, Smits N, Donker T, ten Have M, de Graaf R. Screening for mood and anxiety disorders with the five-item, the three-item, and the two-item Mental Health Inventory. Psychiatry Research. 2009;168:250–255. doi: 10.1016/j.psychres.2008.05.012. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, Chou PS, Huang B, Ruan WJ. Recovery from DSM-IV alcohol dependence: United States, 2001–2022. Addiction. 2005;100:281–292. doi: 10.1111/j.1360-0443.2004.00964.x. [DOI] [PubMed] [Google Scholar]
- DiMaggio C, Galea S, Guohua L. Substance use and misuse in the aftermath of terrorism. A Bayesian meta-analysis. Addiction. 2009;104:894–904. doi: 10.1111/j.1360-0443.2009.02526.x. [DOI] [PubMed] [Google Scholar]
- Dobalian A, Stein JA, Heslin KC, Riopelle D, Venkatesh B, Lanto AB, Simon B, Yano EM, Rubenstein LV. Impact of the Northridge Earthquake on the mental health of Veterans: Results from a panel study. Disaster Medicine and Public Health Preparedness. 2011;5:S220–S226. doi: 10.1001/dmp.2011.60. [DOI] [PubMed] [Google Scholar]
- Enarson E. Identifying and addressing social vulnerabilities. In: Waugh WL, Tierney K, editors. Emergency Management: Principles and Practice for Local Government. Washington, DC: ICMA Press; 2007. pp. 257–278. [Google Scholar]
- Ewing JA. Detecting alcoholism: The CAGE questionnaire. Journal of the American Medical Association. 1984;252:1905–7. doi: 10.1001/jama.252.14.1905. [DOI] [PubMed] [Google Scholar]
- Foster JH, Powell JE, Marshall EJ, Peters TJ. Quality of life in alcohol- dependent subjects – a review. Quality of Life Research. 1999;8:255–261. doi: 10.1023/a:1008802711478. [DOI] [PubMed] [Google Scholar]
- Friedman B, Heisel M, Delavan R. Validity of the SF-36 five-item Mental Health Index for major depression in functionally impaired, community-dwelling elderly patients. Journal of the American Geriatric Society. 2005 Nov;53(11):1978–85. doi: 10.1111/j.1532-5415.2005.00469.x. [DOI] [PubMed] [Google Scholar]
- Jette AM, Davies AR, Cleary PD, Calkins DR, Rubenstein LV, Rink A, Kosecoff J, Young RT, Brook RH, Delbanco TL. The Functional Status Questionnaire: reliability and validity when used in primary care. Journal of General Internal Medicine. 1986;1:143–149. doi: 10.1007/BF02602324. [DOI] [PubMed] [Google Scholar]
- Kavanagh DJ, Connolly JM. Assessment of co-occurring addictive and other mental disorders. In: Miller Peter M., editor. Evidence-based Addiction Treatment. Academic Press; 2009. pp. 89–117. [Google Scholar]
- Lee ML, Yano EM, Wang M, Simon BF, Rubenstein LV. What patient population does visit-based sampling in primary care settings represent? Medical Care. 2002;40:761–770. doi: 10.1097/00005650-200209000-00006. [DOI] [PubMed] [Google Scholar]
- McCabe CJ, Thomas KJ, Brazier JE, Coleman P. Measuring the mental health status of a population: a comparison of the GHQ-12 and the SF-36 (MHI-5) British Journal of Psychiatry. 1996;69:516–21. doi: 10.1192/bjp.169.4.516. [DOI] [PubMed] [Google Scholar]
- Means-Christensen AJ, Arnau RC, Tonidandel AM, Bramson R, Meagher MW. An efficient method of identifying major depression and panic disorder in primary care. Journal of Behavioral Medicine. 2005;28:565–72. doi: 10.1007/s10865-005-9023-6. Epub 2005 Oct 25. [DOI] [PubMed] [Google Scholar]
- Moore RS, Cunradi CB, Ames GM. Did substance abuse change after September 11th? An analysis of a military cohort. Military Medicine. 2004;169:829–32. doi: 10.7205/milmed.169.10.829. [DOI] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. NIH Publication No 97–4017. Bethesda, MD: NIAAA; 2000. Tenth Special Report to the U.S. Congress on Alcohol and Health. [Google Scholar]
- Norquist GS, Hough RL, Golding JM, Escobar JI. Psychiatric disorder in male veterans and nonveterans. Journal of Nervous and Mental Disease. 1990;178(5):328–335. doi: 10.1097/00005053-199005000-00009. [DOI] [PubMed] [Google Scholar]
- North CS, Ringwalt CL, Downs D, Derzon J, Galvin D. Postdisaster course of alcohol use disorders in systematically studied survivors of 10 disasters. Archives of General Psychiatry. 2011;68:173–180. doi: 10.1001/archgenpsychiatry.2010.131. [DOI] [PubMed] [Google Scholar]
- Okoro CA, Brewer RD, Naimi TS, Moriarty DG, Giles WH, Mokdad AH. Binge drinking and health-related quality of life: Do popular perceptions match reality? American Journal of Preventive Medicine. 2004;26:230–233. doi: 10.1016/j.amepre.2003.10.022. [DOI] [PubMed] [Google Scholar]
- Perrine MWB, Schroder KEE, Forester R, McGonagle-Moulton P, Huessy F. The impact of the September 11, 2001, terrorist attacks on alcohol consumption and distress: Reactions to a national trauma 300 miles from ground zero. Journal of Studies on Alcohol and Drugs. 2004;6:5–15. doi: 10.15288/jsa.2004.65.5. [DOI] [PubMed] [Google Scholar]
- Pfefferbaum B, Doughty DE. Increased alcohol use in a treatment sample of Oklahoma City bombing victims. Psychiatry. 2001;64:296–303. doi: 10.1521/psyc.64.4.296.18598. [DOI] [PubMed] [Google Scholar]
- Richman JA, Wislar JS, Flaherty JA, Fendrich M, Rospenda KM. Effects on alcohol use and anxiety of the September 11, 2001, attacks and chronic work stressors: a longitudinal cohort study. American Journal of Public Health. 2004;94:2010–5. doi: 10.2105/ajph.94.11.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenheck R. Reactions to the events of September 11. New England Journal of Medicine. 2002;346:629–30. doi: 10.1056/NEJM200202213460819. [DOI] [PubMed] [Google Scholar]
- Rosenheck R. Institute of Medicine. Committee on Crossing the Quality Chasm: Adaptation to Mental Health and Addictive Disorders. Washington, DC: National Academies Press; 2006. Mental health and substance-use health services for veterans: Experience with performance evaluation in the Department of Veterans Affairs; pp. 423–482. Improving the quality of health care for mental and substance use conditions. [Google Scholar]
- Rumpf HJ, Meyer C, Hapke U, John U. Screening for mental health: validity of the MHI-5 using DSM-IV Axis I psychiatric disorders as gold standard. Psychiatry Research. 2001;105:243–253. doi: 10.1016/s0165-1781(01)00329-8. [DOI] [PubMed] [Google Scholar]
- Stranges S, Notaro J, Freudenheim JL, Calogero RM, Muti P, Farinaro E, Russell M, Nochajski TH, Trevisan M. Alcohol drinking pattern and subjective health in a population-based study. Addiction. 2006;101:1265–1276. doi: 10.1111/j.1360-0443.2006.01517.x. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Veterans Affairs. [Accessed February 6, 2012];Center for Women Veterans: Statistics. Women Veterans Population http://www.va.gov/womenvet/statistics.asp.
- van Leeuwen CM, van der Woude LH, Post MW. Validity of the mental health subscale of the SF-36 in persons with spinal cord injury. Spinal Cord. 2012 Apr 10; doi: 10.1038/sc.2012.33. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Medical Care. 1992;30:473–483. [PubMed] [Google Scholar]
- Wilsnack RW, Vogeltanz ND, Wilsnack SC, Harris TR. Gender differences in alcohol consumption and adverse drinking consequences: cross-cultural patterns. Addiction. 2000;95:251–265. doi: 10.1046/j.1360-0443.2000.95225112.x. [DOI] [PubMed] [Google Scholar]
- Yarnold PR, Bryant FB, Repasy AB, Martin GJ. The factor structure and cross-sectional distributional properties of the Beth Israel/UCLA Functional Status Questionnaire. Journal of Behavioral Medicine. 1991;14:141–153. doi: 10.1007/BF00846176. [DOI] [PubMed] [Google Scholar]
- Yuan KH, Bentler PM, Kano Y. On averaging variables in a confirmatory factor analysis model. Behaviormetrika. 1997;24:71–83. [Google Scholar]


