Abstract
A 39-year-old male patient underwent uncomplicated deep anterior lamellar keratoplasty due to keratoconus. On day 5 after surgery, small whitish infiltrates developed in the corneal interface. The diagnosis of fungal keratitis was made when the culture medium of the graft grew Candida after the surgical intervention. Despite intensive antimycotic treatment and irrigation of the interface, the infiltrates persisted and eventually enlarged. Therefore, revision surgery with penetrating keratoplasty was performed. Microbiological analysis showed Candida orthopsilosis in the culture of the excised graft button. Histopathological staining of the excised graft showed periodic acid–Schiff-positive and Grocott methenamine silver-positive clusters of yeast between Descemet's membrane and the deep corneal stroma with focal perforations through Descemet's membrane. The treatment of mycotic keratitis caused by C orthopsilosis is challenging. Antimycotic treatment was unsuccessful in this case. Progression of the keratitis and perforation of Descemet's membrane suggest that early surgical intervention by penetrating keratoplasty is required.
Background
Deep anterior lamellar keratoplasty (DALK) has become an important alternative to conventional penetrating keratoplasty for disorders of the corneal stroma, mainly keratoconus and scars.1 The main advantage of this technique is the preservation of the host's endothelium and thereby a reduced risk of immunological graft rejections. Because keratoconus is the most common reason for corneal transplantation in young patients, the decreased frequency of graft rejections is of high clinical relevance. Furthermore, in contrast to penetrating keratoplasty, DALK is no ‘open-sky surgery’ and has a lower risk of intraoperative expulsive haemorrhage and intraocular infection. However, there is a small risk of interface complications, especially contamination by microorganisms and infection also due to temporary postsurgical immunosuppression by corticosteroids. Until now only a few cases of fungal interface infections after DALK have been reported.2–6 In posterior lamellar keratoplasties a fungal interface infection can occur as well.7 Furthermore, fungal interface keratitis has been described after refractive surgery, such as excimer photorefractive keratectomy and laser in situ keratomileusis.8 9 Fungal keratitis in corneas without previous surgery occurs predominantly in patients with immunosuppression—for example, in patients with AIDS, and during chemotherapy in patients with cancer or prolonged treatment with corticosteroids.
We report a case of severe fungal interface keratitis after DALK by a microorganism which until now was not known to cause infection after DALK—namely, Candida orthopsilosis, and describe its clinical, microbiological, and histological characteristics.
Case presentation
A 39-year-old man with keratoconus and a best corrected visual acuity of 20/20 in the right eye and 20/200 in the left eye underwent uncomplicated DALK on the left eye. The corneal graft was received from a certified eye bank and had been stored in culture medium containing penicillin (10 000 U), streptomycin (10 000 µg/ml) and amphotericin B (250 µg/ml). After transplantation the medium was sent for culture. The postoperative treatment included topical antibiotics (ofloxacin), miotics (pilocarpine) and topical steroids (prednisolone acetate 1% five times a day) as well as systemic corticosteroids (prednisolone 150 mg/day), which were reduced daily by 20 mg. Five days after surgery, small whitish retrocorneal precipitates at the level of Descemet's membrane became visible at slit lamp examination (figure 1A) and in slit-lamp-adapted optical coherence tomography (SL-OCT) scans (figure 1B, BD 900, SL-OCT, Heidelberg Engineering, Heidelberg, Germany). One day later microbiological analysis of the culture medium showed the growth of yeast. All steroids were discontinued and voriconazole eye drops were given. Since the morphological appearance did not show improvement despite hourly administration of topical voriconazole, interface irrigation with amphotericin B (0.5 mg/ml) and voriconazole (0.25 mg/ml) was performed on day 13 after DALK. After this, the patient was treated with voriconazole eye drops hourly and systemic voriconazole (400 mg by mouth, twice a day) for 4 weeks. After reduction of the antimycotic treatment dexamethasone eye drops were given five times a day. After a 2-month period of stability, sudden deterioration was noticed (figure 2).
Figure 1.

(A) The cornea 12 days after deep anterior lamellar keratoplasty (DALK): whitish, round, retrocorneal infiltrates. (B) Slit-lamp-adapted optical coherence tomography scan with retrocorneal lesions of high reflectivity (day 12 after DALK).
Figure 2.

The cornea 2 months after deep anterior lamellar keratoplasty: increase of the whitish, round, confluent infiltrates.
Treatment
Because of a remarkable increase of the number and size of the infiltrates (figure 2), we decided to perform a penetrating keratoplasty. During surgery, voriconazole (0.25 mg/ml) and amphotericin B (0.5 mg/ml) were applied intracamerally. Microscopic assessment of the excised corneal button disclosed yeast structures. The culture showed C orthopsilosis. Resistance analysis showed sensitivity to voriconazole, fluconazole and amphotericin B.
The postoperative treatment included systemic voriconazole 4 mg/kg intravenously for 2 weeks, voriconazole eye drops five times a day and ofloxacin eye drops.
Differential diagnosis
The diagnosis is mycotic interface keratitis after DALK. The differential diagnosis includes the disorders:
Other types of infectious keratitis, especially due to bacteria. However, the clinical appearance of the infiltrates with white, round lesions with satellites was typical for a mycotic keratitis.
Immunological graft rejection. However, since the endothelium is preserved in DALK, a graft rejection is not very likely in this case.
Epithelial invasion into the interface. This differential diagnosis is unlikely because epithelial invasion usually starts from the periphery (interface between donor rim and host) and spreads to the centre of the cornea.
Investigations
Microbiology
Microscopic assessment of the excised corneal button disclosed yeast structures. The culture showed C orthopsilosis. Protruding remnants of the host's corneal rim, which were also excised during penetrating keratoplasty because of suspicious infection, were cultured and also showed growth of C orthopsilosis. The resistance analysis showed sensitivity to voriconazole, fluconazole and amphotericin B.
Histopathology
Histopathological investigation showed round and oval-shaped structures between Descemet's membrane and the deep corneal stroma which spread into the deep collagenous layers of the stroma (figure 3A). The yeast-like structures were Grocott-positive (Grocott methenamine silver stain) and were assembled in clusters with bulging of Descemet's membrane towards the anterior chamber. At two locations, Descemet's membrane showed perforations by the microorganisms with aggregation of inflammatory cells on the retrocorneal side (figure 3B).
Figure 3.
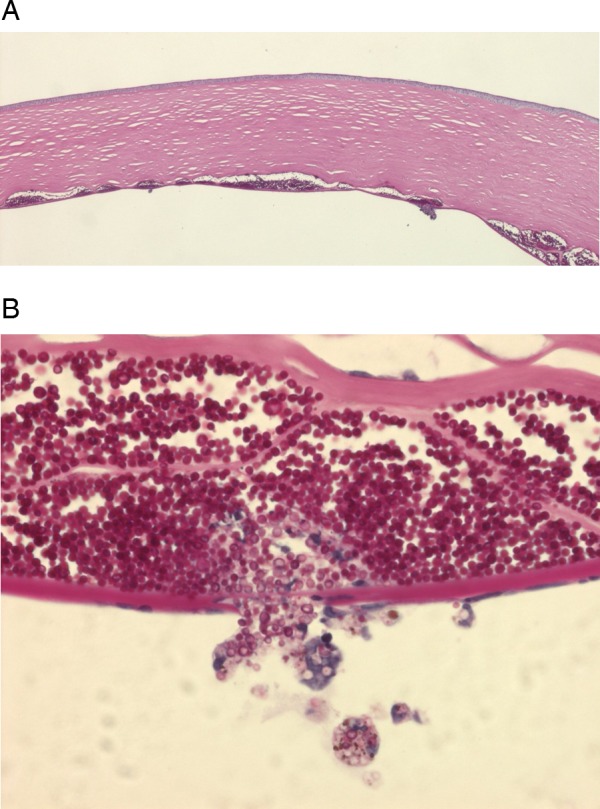
Periodic acid–Schiff staining of the excised corneal button. (A) Clusters of yeasts in the interface between the stroma and Descemet's membrane. (B) Cluster of yeasts with perforation of Descemet's membrane.
Outcome and follow-up
The patient was discharged without signs of recurrence of the fungal interface keratitis with a visual acuity of 10/200. The patient was followed up weekly. No signs of recurrence were seen and there was continuous improvement of visual acuity to 60/200 at the visit 6 months after penetrating keratoplasty (figure 4).
Figure 4.

The cornea 6 months after penetrating keratoplasty: no evidence of recurrence of the fungal keratitis.
Discussion
C orthopsilosis is a new subspecies of Candida which has been characterised in the past few years and has replaced Candida parapsilosis II because of new insights into Candida genetics.10 Fungal keratitis by Candida parapsilosis has been described in case series by Sun et al11 and Bourcier et al.12 In the reported cases of interface keratitis after DALK by Candida albicans and Candida glabrata, the first signs of fungal keratitis were noticed after intervals of between 28 days and 4 months.2–4 6 In our case, fungal keratitis by C orthopsilosis became manifest already on day 5 after DALK, indicating a higher pathogenicity of this species.
Kanavi et al2 reported an interface keratitis after DALK by C glabrata. The authors tried to repeat DALK but during irrigation of the interface, Descemet's membrane ruptured and they had to convert the operation into penetrating keratoplasty. Fontana et al also tried to perform lamellar revision surgery in a patient with interface keratitis due to C albicans. After revision surgery, the keratitis worsened and the surgeon was forced to perform a full-thickness keratoplasty.3
Our case clearly shows the ability of aggressive Candida subspecies to perforate Descemet's membrane. Therefore, we highly recommend penetrating keratoplasty in cases of interface keratitis due to Candida species in order to avoid persistence of fungal remnants on Descemet's membrane. Interface irrigation can be of use to reduce the infiltrates and to allow microbiological analysis, if the fungus was not cultured from the corneoscleral donor rim.
Local and systemic antimycotic treatment should be continued after revision surgery for two reasons: (1) possible fungal invasion of the anterior chamber, and (2) possible fungal infiltrates in the adjacent corneal rim of the host. It is debatable whether antifungal treatment should be started when a positive result of the culture of the corneoscleral rim becomes apparent or if it is sufficient to monitor the patient at short intervals and treat after occurrence of clinical signs of fungal keratitis. Kitzmann et al7 recommend prophylactic local and systemic treatment in all patients with positive corneoscleral rim cultures. Because of the considerable side effects of systemic antimycotic treatment—for example, nephrotoxicity due to amphotericin B or hepatotoxicity due to voriconazole, the administration of antimycotic drugs in the presence of a positive culture result and the absence of clinical signs should be considered carefully.13
Learning points.
Fungal keratitis after deep anterior lamellar keratoplasty may have a serious clinical course.
Candida orthopsilosis is a recently classified Candida species with increasing clinical importance.
Perforation of Descemet's membrane can occur in eyes with a fungal interface keratitis. Therefore, penetrating keratoplasty instead of lamellar revision keratoplasty is recommended in this case.
Acknowledgments
We thank Carmen Hofmann-Rummelt for the excellent histopathological stainings.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Anwar M, Teichmann KD. Big-bubble technique to bare Descemet's membrane in anterior lamellar keratoplasty. J Cataract Refract Surg 2002;28:398–403 [DOI] [PubMed] [Google Scholar]
- 2.Kanavi MR, Foroutan AR, Kamel MR, et al. Candida interface keratitis after deep anterior lamellar keratoplasty: clinical, microbiologic, histopathologic, and confocal microscopic reports. Cornea 2007;26:913–16 [DOI] [PubMed] [Google Scholar]
- 3.Fontana L, Parente G, Di Pede B, et al. Candida albicans interface infection after deep anterior lamellar keratoplasty. Cornea 2007;26:883–5 [DOI] [PubMed] [Google Scholar]
- 4.Bahadir AE, Bozkurt TK, Kutan SA, et al. Candida interface keratitis following deep anterior lamellar keratoplasty. Int Ophthalmol 2012;32:383–6 [DOI] [PubMed] [Google Scholar]
- 5.Fintelmann RE, Gilmer W, Bloomer MM, et al. Recurrent Lecythophora mutabilis keratitis and endophthalmitis after deep anterior lamellar keratoplasty. Arch Ophthalmol 2011;129:108–10 [DOI] [PubMed] [Google Scholar]
- 6.Sedaghat MR, Hosseinpoor SS. Candida albicans interface infection after deep anterior lamellar keratoplasty. Indian J Ophthalmol 2012;60:328–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kitzmann AS, Wagoner MD, Syed NA, et al. Donor-related Candida keratitis after Descemet stripping automated endothelial keratoplasty. Cornea 2009;28:825–8 [DOI] [PubMed] [Google Scholar]
- 8.Dunphy D, Andrews D, Seamone C, et al. Fungal keratitis following excimer laser photorefractive keratectomy. Can J Ophthalmol 1999;34:286–9 [PubMed] [Google Scholar]
- 9.Muallem MS, Alfonso EC, Romano AC, et al. Bilateral candida parapsilosis interface keratitis after laser in situ keratomileusis. J Cataract Refract Surg 2003;29:2022–5 [DOI] [PubMed] [Google Scholar]
- 10.Tavanti A, Davidson AD, Gow NAR, et al. Candida orthopsilosis and Candida metapsilosis spp. nov. To replace Candida parapsilosis Groups II and III. Journal of Clinical Microbiology 2005;43:284–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sun RL, Jones DB, Wilhelmus KR. Clinical characteristics and outcome of Candida keratitis. Am J Ophthalmol 2007;143:1043–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bourcier T, Touzeau O, Thomas F, et al. Candida parapsilosis keratitis. Cornea 2003;22:51–5 [DOI] [PubMed] [Google Scholar]
- 13.Boucher HW, Groll AH, Chiou CC, et al. Newer systemic antifungal agents: pharmacokinetics, safetey and efficacy. Drugs 2004;64:1997–2020 [DOI] [PubMed] [Google Scholar]


