Abstract
Purpose
Recent initiatives by major funding agencies have emphasized translational and personalized approaches (e.g., genetic testing) to health research and health management. While such directives are appropriate, and will likely produce tangible health benefits, we seek to highlight a confluence of several lines of research showing relations between the personality dimension of conscientiousness and a variety of health-related outcomes.
Methods
Using a modified health process model, we review the compelling evidence linking conscientiousness to health and disease processes, including longevity, diseases, morbidity-related risk factors, health-related psycho-physiological mechanisms, health-related behaviors, and social environmental factors related to health.
Conclusion
We argue the accumulated evidence supports greater integration of conscientiousness into public health, epidemiological, and medical research, with the ultimate aim of understanding how facilitating more optimal trait standing might foster better health.
Keywords: Conscientiousness, health, public health
Introduction
In contrast to personality traits, it is widely accepted that social environmental factors, such as socioeconomic status (SES), are significant epidemiological factors that contribute to an understanding of health and longevity (1). One of the primary reasons for the lack of attention paid to personality traits, such as conscientiousness, had been the absence of a widely accepted organizing taxonomy, which, in earlier research, resulted in a confusing proliferation of constructs. However, more than two decades of research have led to a substantially improved depiction of the structure of personality traits, providing an organization based on five broad dimensions labeled the “Big Five” (Extraversion, Agreeableness, Conscientiousness, Emotional Stability, and Openness to Experience; 2). Using this system, researchers have investigated relations between the Big Five and health-related outcomes and have provided evidence for the health-related influences of these traits and their facets.
In the present article, we focus on conscientiousness and argue that sufficient evidence has accumulated to warrant considering this trait domain a consequential epidemiological factor. Conscientiousness is defined as the relatively stable pattern of individual differences in the tendencies to follow socially prescribed norms for impulse control, to be goal-directed, planful, to delay gratification, and to follow norms and rules (3). This definition is meant to be inclusive, representing normal and abnormal trait variation (i.e., disordered levels of trait expression), which is consistent with the dimensional assessment of personality traits planned for the 2013 release of the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5; see www.dsm5.org), a point we cover in further detail below.
Table 1 provides an overview of the range of attributes identified by structural research as being key facets of conscientiousness (4-11). These facets range from the prototypical lay definition of conscientiousness as being reliable (i.e., responsibility) to forms of conscientiousness more closely aligned with being organized (i.e., orderliness) or self-disciplined (i.e., industriousness). As we discuss in subsequent sections, the importance of considering facets of conscientiousness lies in the variable strength of their associations with health-related outcomes. That is, not all facets predict alike.
Table 1.
Example Scales and Representative Descriptors for Conscientiousness-related Facets
| Conscientiousness-related Facets | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Orderliness | Industriousness | Self-Control | Responsibility | Traditionalism | Decisiveness | Formality | Punctuality | Persistence | |
| Example Scales | AB5C Orderliness CCS Orderliness NEO-PI-R Order |
AB5C Purposefulness CCS Industriousness NEO Achievement striving |
AB5C Cautiousness CCS Self-control MPQ Control |
CCS Responsibility CPI Responsibility JPI Responsibility |
CCS Traditionalism MPQ Traditionalism |
Roberts et al. (2004) | Roberts et al. (2004) | Roberts et al. (2004) | Peabody & De Raad (2002) |
| Representative Descriptors | Disorganized(r) Orderly Neat Sloppy (r) |
Hard-working Industrious Lazy (r) |
Careful Cautious Reckless (r) |
Reliable Responsible Unreliable (r) |
Conventional Traditional Untraditional (r) |
Deliberate Firm Inconsistent (r) |
Formal Informal (r) Prim |
Punctual Unpunctual (r) |
Determined Persistent |
Note. AB5C = abridged Big Five dimensional circumplex; CCS = Chernyshenko conscientiousness scales; NEO-PI-R = NEO-personality inventory-revised; MPQ = multidimensional personality questionnaire; CPI = California psychological inventory; JPI = Jackson personality inventory; (r) = reverse scored.
To make the case that conscientiousness should be considered a candidate epidemiological variable, we describe the multiple pathways by which conscientiousness is associated with health. Specifically, we review relations between conscientiousness and mortality, diseases, morbidity-related risk factors, health-related psychophysiological mechanisms, and health-related behaviors, as well as relations to social environmental factors known to contribute to health and longevity. In addition, we present an investigative framework for the continued integration of conscientiousness into epidemiological, public health, and medical research, with the long-term goal of examining how self-directed or managed programs designed to increase conscientiousness might contribute to short- and long-term improvements in health status.
Locating conscientiousness among health processes
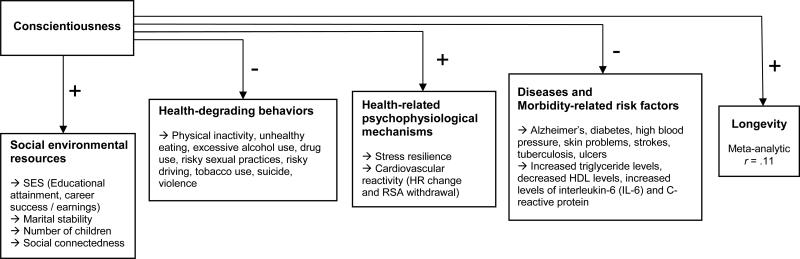
Characterizing the full extent of the relationship between conscientiousness and health requires, at the very least, identifying a model of health and disease processes that is amenable to the inclusion of personality traits. While a complete survey of health process models is beyond the intention of the current work, it is important to note these models vary greatly in their emphases on psychobiological (e.g., stress reaction), psychosocial (e.g., SES), social cognitive (e.g., self-efficacy), and temporal contributions (e.g., early, mid-, and late-life predictors and markers) to a variety of health-related outcomes, ranging from diabetes, to exercise regimen adherence, to smoking cessation, to death itself (cf. 12-16). For the purposes of the review herein, we use a modified version of Adler and Matthews's (1) health process model as an organizing framework (see Figure 1).
Figure 1.
Schematic representation of conscientiousness-health relations, modified from Adler and Matthews's (1994) health process model (+ sign indicates positive association, – sign indicates negative association; SES = socioeconomic status; HR = heart rate; RSA = respiratory sinus arrhythmia; HDL = high-density lipoprotein).
Although not exhaustive in its depiction of the health process, the model does include a specific locus for personality traits and other individual difference factors. Moreover, its generic structure allows for easier modification than other models that were not designed to be general health process frameworks (e.g., transtheoretical model of change; 15), or likewise, models that explicitly prescribe certain variables of interest and delineate pathways and directionality among them (e.g., Reserve Capacity Model; 14). Our re-specification of this model includes the final distal outcome of longevity, as well as an additional pathway from conscientiousness to longevity. Our goal in the following sections is not to render definitive judgments for all possible relations, but to provide an overview of which conscientiousness-health relations are well characterized. Using Figure 1 as an organizing framework, we start our review from the most distal outcome—longevity.
Longevity
Although it is not a prerequisite for consideration as a consequential epidemiological factor, the health-related relevance of any class of psychological constructs, such as personality traits, is greatly enhanced by its association with longevity. Across a variety of samples, using both observer and self-reports, conscientiousness has repeatedly shown significant relations with longevity/mortality. In a sample of cognitively gifted Californians, Friedman and colleagues (17) found that children who were rated by their parents and teachers as being more conscientious tended to live longer, even when controlling for gender and SES. Other research has shown that people suffering from renal deficiency tend to live longer if they are more conscientious (18). Wilson et al. (19) found conscientiousness was associated with longevity in a sample of Catholic clergy members, even when conscientiousness was assessed in old age. Conscientiousness also was shown to be associated with longevity in a heterogeneous sample of older community members living on the East Coast and in the Midwest (20).
Kern and Friedman (21) meta-analyzed these results and others and, across 20 independent samples, produced the most robust estimate to date of the relationship between conscientiousness and longevity (r = .11, 95% CI = .05-.17). Recent research continues to bolster this meta-analytic finding, showing that a representative sample of Scottish youth who were rated as more dependable in childhood lived longer than their peers, even when controlling for intelligence (22), and that, in a large sample of adults in their mid-70s, lower levels of conscientiousness predicted increased risk of mortality 6.5 years later (23).
The consistent positive association between conscientiousness and longevity is impressive considering the diverse samples and assessment methods used across these studies. An earlier meta-analysis of studies linking conscientiousness to mortality showed the effect of conscientiousness on mortality to be three times the size of the effect of socioeconomic status (24). The relationship between conscientiousness and longevity allows for a consideration of direct and indirect pathways to mortality via diseases, morbidity-related risk factors, health-related psychophysiological mechanisms, health-related behaviors, and social environmental factors—pathways we describe in the following sections.
Diseases
In a large nationally representative sample, Goodwin and Friedman (25) found lower conscientiousness to be associated with many of the actual causes of mortality and indicators of pathology, including diabetes, high blood pressure, skin problems, strokes, ulcers, and tuberculosis. Recent research also has linked low conscientiousness to the mismanagement of glycemic control in Type 1 diabetes patients (26). In addition, low conscientiousness predicts increased medical illness burden in older adults as rated by physicians (27).
Conscientiousness also has been shown to be associated with Alzheimer's disease and related cognitive deficits across several studies, suggesting an additional pathway via deteriorating cognition that conscientiousness might affect health. In a longitudinal study of Catholic clergy, higher levels of conscientiousness were associated with a reduced likelihood of Alzheimer's disease diagnosis twelve years later (28). More recently, the finding was replicated in a 6-year prospective longitudinal study on a more representative sample of individuals older than age 72 participating in a clinical trial of Gingko supplementation (29). Related findings from a sample including individuals with mild cognitive impairment (often a marker for the onset of Alzheimer's disease) showed those with reduced cognition were more likely to rate themselves and be rated by others as being less conscientious (30). In addition, low levels of conscientiousness have demonstrated associations with attentional deficits commonly linked to Alzheimer's-related dementia (31). The Alzheimer's-related findings indicate cognitive functioning and capacity could serve an intermediate role in the relationship between conscientiousness and longevity. Supporting this argument is a recent study showing that cognitive function partially mediates the relation between conscientiousness and mortality (32).
However, more research is needed to clarify possible reciprocal relations between declines in cognitive functioning and lower levels of conscientiousness. It may be the case that lower levels of conscientiousness earlier in life may contribute to mild cognitive decline later in life and that the development of symptoms of declining cognitive function then contributes to deficits in facets of conscientiousness related to planning and cognitive control (e.g., orderliness and self-control). In other words, low conscientiousness might confer increased risk for cognitive decline via cumulative lifestyle effects. In turn, the subsequent pathology of mild cognitive decline could contribute to further reductions in facets of conscientiousness whose expression is more strongly tied to diminished levels of attentional control.
Taken together, the above disease-related findings suggest low conscientiousness is a potential phenotypic marker for an increased risk of a variety of pathologies. To be sure, the research described above represents the vanguard of conscientiousness-disease investigations. A great deal more work is required before a complete account of this pathway can be described.
Morbidity-related risk factors
Research has linked conscientiousness to a variety of physiological markers known to be risk factors for poor health. In a study using a population-based sample from Sardinia, Italy, Sutin and colleagues (33, 34) found low levels of conscientiousness to be associated with increased triglyceride levels (which, in turn, contribute to atherosclerosis), decreased high-density lipoprotein levels (the “good” cholesterol carrier that can move cholesterol from arteries to the liver where it can be reused or excreted), and increased levels of interleukin-6 (IL-6) and C-reactive protein (markers of chronic inflammation). Providing some support for an indirect pathway from conscientiousness through health-related behaviors to disease, Sutin et al. (34) found the relationship between an impulsivity facet of conscientiousness and IL-6 was partially mediated by cigarette smoking. Recent research replicated these findings in a more rigorous, 20-year prospective longitudinal study. Low self-control (a facet of conscientiousness) at age 10 was found to predict a composite measure of metabolic factors, such as high blood pressure and low high-density lipoprotein, as well as elevated levels of C-reactive protein at age 32, even when controlling for IQ and socioeconomic status (35).
As is evident from the mediated path found by Sutin and colleagues, the conscientiousness-morbidity pathway is sure to benefit from a combined account of intermediate factors, such as psychophysiological mechanisms, health-related behaviors, and social environmental factors.
Health-related psychophysiological mechanisms
Recent research suggests conscientiousness is associated with another key health-related factor: Stress. The experience of stress and psychophysiological reactions to it are associated with a broad swath of health problems, including cardiovascular disease (36). Higher levels of conscientiousness are associated with a reduced exposure to stress (37, 38). In addition, higher levels of conscientiousness are associated with an increased appraisal of coping abilities, as well as higher levels of control in the context of a stressor (39). Moreover, conscientious individuals tend to find stressful situations less demanding than less conscientious individuals. Similarly, in stressful contexts, higher levels of conscientiousness are associated with using more adaptive coping strategies, such as instrumental problem solving and effective cognitive restructuring (40).
Other recent studies have examined the relationship between conscientiousness-related traits and cardiovascular reactivity during challenging and stressful laboratory tasks. Using mental arithmetic, reaction time, and speech preparation/delivery tasks, Heponiemi et al. (41) found individuals scoring higher on a measure of impulsive sensation-seeking showed increased heart rate reactivity and greater respiratory sinus arrhythmia withdrawal (an indicator of parasympathetic regulation of heart rate) compared to individuals scoring lower on impulsive sensation-seeking. Related work by Allen, Hogan, and Laird (42) using a speech preparation task showed a measure of impulsiveness to negatively predict heart rate reactivity (i.e., impulsive individuals showed less heart rate change during speech preparation). More work is required to definitively discern the underlying patterns of effects between conscientiousness-related traits and cardiovascular reactivity, especially given the variety of possible task and trait measurement options.
Although implied by the above findings, little research has examined the mediating role of stress in the relationship between conscientiousness and health-related outcomes. In a one-year longitudinal study of HIV-infected individuals, stress was found to mediate the relationship between conscientiousness and disease progression (43). As suggested by these preliminary findings, the intervening role of stress in the relationship between conscientiousness and health-related outcomes warrants additional attention.
Health-degrading behaviors
The leading behavioral contributors to mortality in the United States are tobacco use, poor diet and physical inactivity, excessive alcohol use, risky driving/accidents, shootings, risky sexual behavior, and illicit drug use (44). These behaviors are relevant to health and longevity through their relations to cardiovascular disease, cancer, accidental deaths, and diabetes, among other causes of death. In a meta-analytic review of 194 relevant studies, conscientiousness was found to be associated with all of the leading behavioral contributors to mortality, operationalized as physical activity, unhealthy eating, excessive alcohol use, drug use, risky sexual practices, risky driving, tobacco use, suicide, and violence (45). Three points about this research merit emphasis: The effects of conscientiousness-related traits were consistent across health-related behaviors; the effect sizes were as large as or larger than many other risk factors for health (46); and the amount of data synthesized provides increased confidence in the nature of the findings.
Social environmental resources associated with health
Social environmental factors are context-dependent experiences that can diminish health (e.g., stressful events or life circumstances) or promote health (e.g., strong social connections; 1). For example, one distinctly stressful social environmental factor, poverty (low SES), is related to poor health outcomes for both men and women (47, 48). Recent research shows conscientiousness predicts health status, in part, through its relationship with educational attainment, a common indicator of SES (49). Moreover, stressful experiences within marriage, such as divorce, are linked to poor health outcomes and decreased longevity (50). Conversely, having greater levels of social connection, such as having more children, belonging to clubs, churches, and other organizations, is linked to positive health outcomes and increased longevity (51, 52). Conscientiousness predicts these social environmental factors via its relations to education (53), career success and earnings (54), greater marital stability (55), and belonging to more organizations in adulthood (56). In turn, having better social support in adulthood is a contributing factor to increased longevity (52). Recently, these findings have been extended to show that spouses’ levels of conscientiousness predict their partners’ health outcomes above and beyond their self-ratings of conscientiousness (57). The above findings indicate that conscientious individuals tend to inhabit social environmental niches that promote better health and increased longevity.
To date, the empirical evidence is consistent with the argument that conscientiousness deserves greater attention in epidemiological, public health, and medical research. Simply stated, scores on measures of conscientiousness-related traits predict many of the disease-related outcomes and biomarkers, health-related behaviors, social environmental factors, and psychophysiological mechanisms (though the evidence for these is equivocal) known to contribute to health processes. While complex biological and environmental processes contribute to an individual's standing on conscientiousness at a given time, assessing it is a straightforward endeavor, with reliability and predictive utility among the features and benefits of measurement. Despite being a marker of health and longevity and easily assessed, most of the research to date linking conscientiousness to health has not been embedded in large-scale epidemiological, public health, or medical studies, an issue we turn to next.
Integrating conscientiousness into public health, epidemiological, and medical research
As a complement to the continuation of the specific lines of research described above future research investigating the role of conscientiousness in the health process should emphasize three related goals (see Table 2): 1) identify the earliest pathways by which conscientiousness contributes to health-protective levels of psychophysiological mechanisms and biomarkers; 2) investigate the co-development of conscientiousness and health-related behaviors throughout the life course; and 3) examine the dynamic system of genetic, neurological, physiological, cognitive-motivational, and social environmental factors that contributes to change in the expression of conscientiousness, and evaluate that system's utility for personalized health-related interventions and public health initiatives.
Table 2.
Research Aims and Venues for Conscientiousness-Health Investigations
| Aims |
| • Identify early pathways from conscientiousness to health protection |
| • Investigate life course co-development of conscientiousness and health-related behaviors |
| • Examine dynamic system of conscientiousness and health-related interventions |
| Venues |
| • Electronic health/medical records, forthcoming psychodiagnostic protocols (i.e., DSM-5) |
| • Inclusion in large ongoing panel studies (e.g., Nurses’ Health Studies) |
| • Initiatives at NIH (e.g., NIH Toolbox), CDC, private, and non-profit research organizations |
The importance of identifying the earliest pathways by which conscientiousness affects health status is highlighted by past and ongoing research showing that childhood measures of conscientiousness or its analogues predict an entire range of health outcomes in adulthood (35, 53). For example, measures of childhood conscientiousness predicted higher educational attainment in young adulthood, which, in turn, predicted better health in mid-life (53). These findings suggest individual differences in conscientiousness start to have effects on adult health outcomes quite early in life. The fact that individual differences in childhood conscientiousness affect adult health outcomes invites research questions concerning the social environmental, health behavioral, and physiological mechanisms that are responsible for these predictive effects. It also highlights the importance of early interventions to prevent the problematic effects of low conscientiousness or to change levels of conscientiousness early in life to promote health (See the third goal below.).
Addressing the co-development of conscientiousness and health-related behaviors also is critical because it can point to ways to intervene and potentially inoculate against the effects of low conscientiousness. Most people increase in conscientiousness with age (58). Moreover, people who increase in conscientiousness and its associated components also show increases in health behaviors and health (35, 55, 59). Conversely, people who partake in deleterious health behaviors, such as alcohol and drug abuse, tend not to increase in conscientiousness over time and with age (55, 60, 61). These findings provide evidence for the temporal interplay between health-related behaviors and conscientiousness, such that engaging in some health-related behaviors actually affects change in conscientiousness. Recent research shows some of the cross-temporal relations between conscientiousness and substance-use behaviors, for example, are related to investment in normative roles, such as being a college student, suggesting a role for social identity in explaining the patterns of co-development between conscientiousness and health-related behaviors (62). Identifying additional mediating factors (e.g., behavioral self-efficacy, likelihood of behavioral goal attainment; 63, 64) and moderating factors (e.g., daily hassles; 65) is a key task for cross-sectional and longitudinal personality-health-behavior research and personality science, in general (66).
The third goal of examining the dynamic system of genetic, physiological, neurological, cognitive-motivational, and social environmental factors that inform the dynamic expression of conscientiousness is especially relevant to identifying preventative pathways. As should be evident from the above review, conscientiousness is a health- and mortality-predictive phenotype with established relations to a host of social environmental factors. As such, it represents a strong candidate for molecular genetics and sociogenomic research (67, 68), including examinations of gene-environment and gene-gene correlations and interactions, and gene expression patterns. To date, many of the research findings for the genetic markers of conscientiousness-related traits have been inconclusive, often producing very weak or null effects, or have been hindered by technical, logistical, and/or financial challenges, including the difficulty of sorting through the plethora of candidate genes identified from genomewide linkage analysis, whole-genome, and animal studies (69-72). However, in the long term, recent advances in molecular genetic epidemiology as well as the burgeoning field of genomics (73) should allow for more robust and feasible identification of genetic markers and the physiological systems they inform.
New venues for studying and utilizing the growing science surrounding conscientiousness and health are the settings where individuals are most likely to interface with the public health and medical systems; that is, in encounters with physicians, mental health providers, and other healthcare professionals. In addition to the direct and indirect effects of conscientiousness on health described above, conscientiousness also contributes to better adherence to medical recommendations (7), one of the most pernicious issues in health care settings. Folding the assessment of conscientiousness into medical settings will require a more enterprising perspective on the part of hospitals, clinics, and individual physicians and clinicians.
In medical settings, a ready medium for such assessment is the patient history protocol or, part of the initial clinical medical history and physical examination obtained from a patient. A very brief measure of conscientiousness could be incorporated into this ubiquitous component of medical record keeping. Such an assessment could easily be embedded into electronic health records or electronic medical records. This form of integration is particularly useful because individual physicians and/or researchers would be able to readily track changes in health and conscientiousness in specific patients or groups of patients over time. To the extent that electronic health and/or medical records are interoperable (i.e., available between various providers), this information could provide a small increment in pre-encounter understanding when a patient is referred to (or seeks out) care elsewhere. This information can be used to flag patients who might benefit from increased or more elaborate compliance instructions/aids/reminders. In addition, because conscientiousness is relatively stable (not to be confused with immutable, as noted below), it does not require frequent assessment (e.g., once every 8-12 months would be adequate, but ultimately, frequency of assessment would be determined by the length of the interval between contacts with healthcare settings and/or the need to track progress of trait modification).
In regard to mental health settings, the planned 2013 release of the DSM-5 will be a widely adopted medium that is slated to include five broad personality trait domains and related facets, including a broad trait domain related to conscientiousness (disinhibition versus compulsivity). The proposed facets of disinhibition versus compulsivity include distractibility, impulsivity, irresponsibility, rigid perfectionism, and risk taking. Field research is currently being conducted to evaluate the psychometric properties and diagnostic and predictive utility of these scales, including their correspondence with Big Five measures of normal personality traits. To the extent disinhibition versus compulsivity and its facets are retained in the final release of DSM-5, new versions of commonly used psychodiagnostic interviews and related materials will likely include measures of these traits and facets. Once the ongoing field research is compiled, a more accurate account of the concordance between these domains and existing personality trait measures will reveal which scale(s) are useful proxies for conscientiousness-related traits. Thereafter, clinicians and other mental health professionals will have a select group of built-in conscientiousness-related scales at their disposal. Not only will DSM-5 represent a shift in the assessment of psychopathology, it will represent a wholesale broadening of the assessment of dimensional personality traits.
Changing conscientiousness to improve health status
In the past decade, personality research has provided evidence for two patterns of trait development relevant to health status: Consistency and change. A large-scale meta-analysis of longitudinal studies showed individuals tend to exhibit relatively high levels of rank-order consistency for conscientiousness, especially over shorter spans of time (i.e., over time, the most conscientious person at one time point is likely to be among the most conscientiousness at a later time point; 74). Results from another large-scale meta-analysis of longitudinal studies showed there to be normative patterns of mean-level change in conscientiousness across the life course, with the largest mean-level increase in conscientiousness occurring in early adulthood and smaller mean-level increases found in later life (58). Taken together, these findings show that personality traits do change and change throughout the life course.
The fact that traits, such as conscientiousness, can change invites the real possibility that they could be directly modified through intervention. To the extent an individual is observed to have reduced standing on conscientiousness with concomitant reduced health status, then a further consideration of how one might purposefully change conscientiousness to improve health status becomes possible.
There is a converging set of research findings demonstrating the changeability of personality traits through direct intervention. To date, the best evidence personality traits can be changed comes from intervention studies of psychotherapy and/or medication. In one of the earliest meta-analytic reviews on the topic, moderate-sized changes in personality trait measures were attributed to individual-based psychotherapy techniques (75). More recent studies show therapy is associated with changes in personality traits. For example, after a 20-week cognitive behavior therapy intervention designed to treat depression, patients changed on a number of personality traits, most notably extraversion and neuroticism (76). Similarly, individuals with generalized social phobia treated with a combination of either tianeptine or fluoxetine (the active drug in Prozac) and therapy showed significant positive increase in all Big Five personality traits (77). In addition, other forms of interventions, such as training programs, appear to change personality traits. For example, mindfulness meditation training in medical students contributed to changes in conscientiousness, agreeableness, empathy, and emotional stability (78).
Taken together, the above findings suggest therapeutic (including pharmacological) and training interventions are strong candidate modes of purposeful trait modification. However, none of these studies (or their respective manipulations) was designed with deliberate trait change as a primary (or explicit) goal. Recently, one such deliberate approach to modifying standing on conscientiousness was explored using a case example of a client involved in substance abuse relapse prevention (79). The proposed approach uses expectancy value theory (80) as a conceptual model for the targets of conscientiousness-related change (i.e., the value of related characteristics and behaviors, such as being self-controlled and reliable; beliefs about engagement in behaviors relevant to one's identity; and the level of self-efficacy regarding one's ability to enact such behaviors) and Behavioral Activation (81) as the therapeutic mode of implementing the change (i.e., tracking behavior, developing goals, planning new/modified behaviors, adjusting values, and being diligent/effortful) to foster on-going modification of behavioral aspects of conscientiousness that contributes to long-term dispositional changes. Such an approach is not meant to be a catch-all, but rather serves as a cogent example of the possibilities for more deliberate and targeted trait interventions that are informed by personality theory and therapeutic approaches.
Indeed, while there are likely to be many viable theory-practice combinations, a complementary framework that captures shared processes amid the disparate conceptual models and applied intervention techniques could serve the purpose of providing a common reference point for a consideration of deliberate trait change in the service of improving health status. One such possibility is a bi-phasic model of trait modification. Models of motivation and behavioral change, as well as behavior change research findings, suggest stages (such as those of the transtheoretical model) can be useful for defining groups for tailored interventions, but that the change process is better conceptualized as occurring in one of two contiguous and continuous phases – motivational and volitional (82-85). The motivational phase of change involves creating awareness of the possibility and need for change, its associated benefits (or risks of inaction), as well as planning how change(s) might be implemented. The volitional phase of change involves the enaction and perpetuation of the plans and goals developed during the motivational phase. While a complete elaboration of the components of such a bi-phasic model is beyond the scope of the current work, the intent of the model is to provide a framework by which researchers and clinicians can locate an individual's progress along dimensions of change and select among several phase-relevant conceptual targets of change and specific modes of change to design and implement trait-modification interventions.
Conscientiously assessing conscientiousness
There are many valid, brief, and cost-free assessment instruments available for measuring conscientiousness, many of which do not use conscientiousness as a label or organizing framework. Although it is always preferable to have the research context and goals guide the selection of an assessment instrument, we recognize that ease and speed of assessment can make the difference between exclusion and inclusion of measures, especially in large-scale studies where depth of coverage must often be sacrificed for breadth of coverage. Ease and speed of delivery also are essential in medical or clinical settings where research goals are tangential or incidental to the tasks of medical or mental health screening or obtaining a medical history. In time-intensive large-scale studies or brief clinical encounters, economy of assessment is critical, even at the expense of some reduction in the psychometric properties of the assessment instrument.
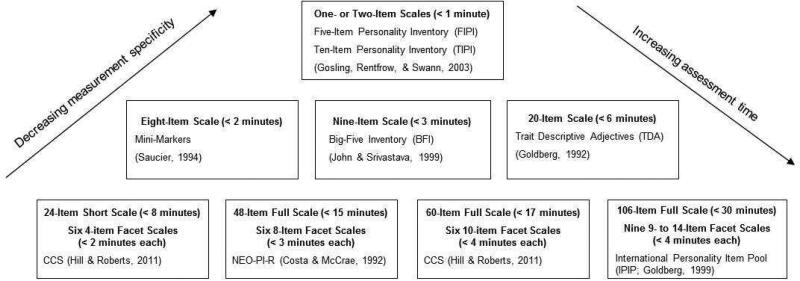
Although a complete review of the advantages and disadvantages of the many instrument possibilities is beyond the reach of this discussion, Figure 2 provides a brief overview of primarily cost-free and publicly available assessment options for conscientiousness (this depiction excludes measures currently being developed for DSM-5). At the top of Figure 2 are examples of the most brief and general of the instruments (i.e., the Five-Item Personality Inventory and the Ten-Item Personality Inventory; 86), followed by examples of instruments with increasing levels of coverage, specificity, and assessment time (Big-Five Inventory, 87; Trait Descriptive Adjectives, 88; Mini-Markers, 89; Chernyshenko Conscientiousness Scales, 7; NEO-Personality Inventory-Revised , 4; International Personality Item Pool, 5). The list is not exhaustive and, most notably, does not include personality trait instruments constructed prior to the formulation of the Big Five dimensions of normal personality trait variation (e.g., California Psychological Inventory, 6; Multidimensional Personality Questionnaire, 11). These omissions should not be taken to mean that such instruments are antiquated or inadequate. In many cases, these instruments include scales that map neatly onto one or more facets of the lower-order structure of conscientiousness.
Figure 2.
Overview of select conscientiousness-related instruments (CCS = Chernyshenko Conscientiousness Scales; NEO-PI-R = NEO-Personality Inventory-Revised). With the exception of the NEO-PI-R, all the instruments are free and publicly available. Although all of the items of the Chernyshenko Conscientiousness Scales are available in the referenced citation, interested readers should contact the corresponding author for the specific items used in the short version of the scales.
While it would be easy to simply select an instrument based on the time available for assessment, such an approach would likely be to the detriment of the larger research enterprise. Specifically, the instrument features of coverage and specificity require careful consideration and should be guided by past research, a priori models of conscientiousness-health relations, or pilot data. For example, based on a six-factor lower-order structure of conscientiousness, meta-analytic work showed that not all facets of conscientiousness are similarly predictive of a given health-related behavior (45). Whereas excessive alcohol consumption was most strongly predicted by the facet of self-control and only weakly predicted by the facet of industriousness, the opposite pattern held true for the health-related behavior of physical inactivity. The lesson from these findings is that—for either behavior—a full-coverage measure of conscientiousness is probably not required, nor would a broad instrument necessarily be of greatest value. Rather, the best measure could be as brief as a broad coverage mid-range instrument, but would have to be selected from a measure that has high specificity and coverage across several facets (e.g., NEO-Personality Inventory-Revised; 4). The differential selection of conscientiousness-related measures certainly requires additional planning and reviewing legwork, but the benefits of an on-target assessment are more than worth the effort.
In spite of what might appear to be unbridled enthusiasm for conscientiousness, we recognize it is not a panacea. Moreover, it is not the only personality trait to have shown relations with important health-related outcomes. Neuroticism also has shown robust relations with many of the outcomes reviewed herein, including mortality (57, 90, 91). The argument for conscientiousness is not intended to exclude neuroticism or other traits (e.g., hostility, optimism), but is meant to draw attention to its role in the health process. The accumulating evidence suggests the assessment of conscientiousness represents an opportunity to augment the best practices of public health, epidemiological, and medical research. We believe that the inclusion of conscientiousness in the health process can help complement and inform recent mandates for translational research and personalized medicine.
Acknowledgements
Preparation of this article was supported, in part, by National Institute on Alcohol Abuse and Alcoholism grant R00 AA017877 to T. Bogg, and National Institute on Aging grant R01 AG21178 to B. W. Roberts.
Footnotes
Conflict of Interest Statement
The authors have no conflicts of interest to disclose.
Contributor Information
Tim Bogg, Department of Psychology, Wayne State University, Detroit, MI 48202.
Brent W. Roberts, Department of Psychology, University of Illinois at Urbana-Champaign, Champaign, IL 61820
References
- 1.Adler N, Matthews K. Health Psychology: Why do some people get sick and some stay well? Annu Rev Psychol. 1994;45:229–259. doi: 10.1146/annurev.ps.45.020194.001305. [DOI] [PubMed] [Google Scholar]
- 2.Goldberg LR. The structure of phenotypic personality traits. Am Psychol. 1993;48:26–34. doi: 10.1037//0003-066x.48.1.26. [DOI] [PubMed] [Google Scholar]
- 3.Roberts BW, Jackson JJ, Fayard JV, Edmonds G. Conscientiousness. In: Leary M, Hoyle R, editors. Handbook of individual differences in social behavior. Guilford; New York, NY: 2009. pp. 369–381. [Google Scholar]
- 4.Costa PT, McCrae RR. Revised NEO Personality Inventory (NEO-PI-R) and NEO Five-Factor Inventory (NEO-FFI) manual. Psychological Assessment Resources; Odessa, FL: 1992. [Google Scholar]
- 5.Goldberg LR. A broad-bandwidth, public-domain, personality inventory measuring the lower-level facets of several five-factor models. In: Mervielde I, Deary I, De Fruyt F, Ostendorf F, editors. Personality psychology in Europe. Vol. 7. Tilburg University Press; Tilburg, The Netherlands: 1999. pp. 7–28. [Google Scholar]
- 6.Gough HG. Manual for the California Psychological Inventory. Consulting Psychologists Press; Palo Alto, CA: 1969. [Google Scholar]
- 7.Hill P, Roberts BW. The role of adherence in the relationship between conscientiousness and perceived health. Health Psychol. 2011;30:797–804. doi: 10.1037/a0023860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jackson DN. Jackson Personality Inventory manual. Research Psychologists Press; Port Huron, MI: 1976. [Google Scholar]
- 9.Peabody D, De Raad B. The substantive nature of psycholexical personality factors: A comparison across languages. J Pers Soc Psychol. 2002;83:983–997. doi: 10.1037//0022-3514.83.4.983. [DOI] [PubMed] [Google Scholar]
- 10.Roberts BW, Bogg T, Walton KE, Chernyshenko OS, Stark SE. A lexical investigation of the lower-order structure of conscientiousness. J Res Pers. 2004;38:164–178. [Google Scholar]
- 11.Tellegen A. Brief manual of the Multidimensional Personality Questionnaire. University of Minnesota; 1982. Unpublished manuscript. [Google Scholar]
- 12.Ajzen I, Fishbein M. Understanding attitudes and predicting social behavior. Prentice-Hall; Englewood Cliffs, NJ: 1980. [Google Scholar]
- 13.Contrada RJ, Leventhal H, O'Leary A. Personality and Health. In: Pervin LA, editor. Handbook of personality: Theory and research. Guilford; New York: 1990. pp. 638–669. [Google Scholar]
- 14.Gallo LC, Matthews KA. Understanding the association between socioeconomic status and physical health: do negative emotions play a role? Psychol Bull. 2003;129:10–51. doi: 10.1037/0033-2909.129.1.10. [DOI] [PubMed] [Google Scholar]
- 15.Prochaska JO, DiClemente CC. The transtheoretical approach: Crossing traditional boundaries of change. Dorsey Press; Homewood, IL: 1984. [Google Scholar]
- 16.Repetti RL, Taylor SE, Seeman TE. Risky families: Family social environments and the mental and physical health of offspring. Psychol Bull. 2002;128:330–366. [PubMed] [Google Scholar]
- 17.Friedman HS, Tucker JS, Tomlinson-Keasey C, et al. Does childhood personality predict longevity? J Pers Soc Psychol. 1993;65:176–185. doi: 10.1037//0022-3514.65.1.176. [DOI] [PubMed] [Google Scholar]
- 18.Christensen AJ, Moran PJ, Johnston DW, et al. Psychological aspects of end-stage renal disease. In: Johnston D, Johnston M, editors. Health psychology: Comprehensive clinical psychology. Vol. 8. Elsevier Science Publishers; Amsterdam, Netherlands: 2001. pp. 321–338. [Google Scholar]
- 19.Wilson RS, de Leon CFM, Bienias JL, et al. Personality and mortality in old age. J Gerontol B- Psychol. 2004;59B:110–116. doi: 10.1093/geronb/59.3.p110. [DOI] [PubMed] [Google Scholar]
- 20.Weiss A, Costa PT. Domain and facet personality predictors of all-cause mortality among medicare patients aged 65 to 100. Psychosom Med. 2005;67:715–723. doi: 10.1097/01.psy.0000181272.58103.18. [DOI] [PubMed] [Google Scholar]
- 21.Kern ML, Friedman HS. Do conscientious individuals live longer? A quantitative review. Health Psychol. 2008;27:505–512. doi: 10.1037/0278-6133.27.5.505. [DOI] [PubMed] [Google Scholar]
- 22.Deary IJ, Batty GD, Pattie A, Gale CR. More intelligent, more dependable children live longer. Psychol Sci. 2008;19:874–880. doi: 10.1111/j.1467-9280.2008.02171.x. [DOI] [PubMed] [Google Scholar]
- 23.Fry PS, Debats DL. Perfectionism and the five-factor personality traits as predictors of mortality in older adults. J Health Psychol. 2009;14:513–524. doi: 10.1177/1359105309103571. [DOI] [PubMed] [Google Scholar]
- 24.Roberts BW, Kuncel NR, Shiner R, et al. The power of personality: the comparative validity of personality traits, socioeconomic status, and cognitive ability for predicting important life outcomes. Perspect Psychol Sci. 2007;2:313–345. doi: 10.1111/j.1745-6916.2007.00047.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Goodwin RD, Friedman HS. Health status and the Five-Factor personality traits in a nationally representative sample. J Health Psychol. 2006;11:643–654. doi: 10.1177/1359105306066610. [DOI] [PubMed] [Google Scholar]
- 26.Vollrath ME, Landolt MA, Gnehm HE, et al. Child and parental personality are associated with glycaemic control in Type 1 diabetes. Diabet Med. 2007;249:1028–33. doi: 10.1111/j.1464-5491.2007.02215.x. [DOI] [PubMed] [Google Scholar]
- 27.Chapman BP, Lyness JM, Duberstein P. Personality and medical illness burden among older adults in primary care. Psychosom Med. 2007;69:277–282. doi: 10.1097/PSY.0b013e3180313975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wilson RS, Schneider JA, Arnold SE, et al. Conscientiousness and the incidence of Alzheimer disease and mild cognitive impairment. Arch Gen Psychiat. 2007;64:1204–1212. doi: 10.1001/archpsyc.64.10.1204. [DOI] [PubMed] [Google Scholar]
- 29.Jerant A, Chapman B, Duberstein P, Robbins J. Personality and medication non-adherence among older adults enrolled in a six-year trial. Brit J Health Psych. 2011;16:151–169. doi: 10.1348/135910710X524219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Duchek JM, Balota DA, Storandt M, Larsen R. The power of personality in discriminating between healthy aging and early-stage Alzheimer's disease. J Gerontol B- Psychol. 2007;62B:353–361. doi: 10.1093/geronb/62.6.p353. [DOI] [PubMed] [Google Scholar]
- 31.Tse CS, Balota DA, Yap MJ, Duchek JM. Effects of healthy aging and early stage dementia of the Alzheimer's type on components of response time distributions in three attention tasks. Neuropsychol. 2010;24:300–315. doi: 10.1037/a0018274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hill PL, Turiano NA, Hurd MD, Mroczek DK. Conscientiousness and longevity: An examination of possible mediators. Health Psychol. 2011;30:536–541. doi: 10.1037/a0023859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sutin AR, Terracciano A, Deiana B, et al. Cholesterol, triglycerides, and the Five-Factor Model of personality. Biol Psychol. 2010;84:86–191. doi: 10.1016/j.biopsycho.2010.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sutin AR, Terracciano A, Deiana B, et al. High neuroticism and low conscientiousness are associated with interleukin-6. Psychol Med. 2010;40:1485–1493. doi: 10.1017/S0033291709992029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Moffitt TE, Arseneault L, Belsky D, Dickson N, et al. A gradient of childhood self-control predicts health, wealth, and public safety. P Natl Acad Sci USA. 2010;2011;108:2693–2698. doi: 10.1073/pnas.1010076108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hamer M, Malan L. Psychophysiological risk markers of cardiovascular disease. Neurosci Biobehav R. 2010;2010;35:76–83. doi: 10.1016/j.neubiorev.2009.11.004. [DOI] [PubMed] [Google Scholar]
- 37.Lee-Baggeley D, Preece M, DeLongis A. Coping with interpersonal stress: Role of Big Five traits. J Pers. 2005;74:9–46. doi: 10.1111/j.1467-6494.2005.00345.x. [DOI] [PubMed] [Google Scholar]
- 38.Vollrath M. Personality and hassles among university students: A three-year longitudinal study. Eur J Psychol. 2000;14:199–215. [Google Scholar]
- 39.Penley JA, Tomaka J. Associations among the Big Five, emotional responses, and coping with acute stress. Pers Indiv Differ. 2002;32:1215–1228. [Google Scholar]
- 40.Connor-Smith JK, Flachsbart C. Relations between personality and coping: A meta-analysis. J Pers Soc Psychol. 2007;93:1080–1107. doi: 10.1037/0022-3514.93.6.1080. [DOI] [PubMed] [Google Scholar]
- 41.Heponiemi T, Keltikangas-Jarvinen L, Kettunen J, Puttonen S. BIS–BAS sensitivity and cardiac autonomic stress profiles. Psychophysiology. 2004;41:37–45. doi: 10.1111/1469-8986.00118. [DOI] [PubMed] [Google Scholar]
- 42.Allen MT, Hogan AM, Laird LK. The relationships of impulsivity and cardiovascular responses: The role of gender and task type. Int J Psychophysiol. 2009;73:369–376. doi: 10.1016/j.ijpsycho.2009.05.014. [DOI] [PubMed] [Google Scholar]
- 43.O'Cleirigh C, Ironson G, Weiss A, Costa PT. Conscientiousness predicts disease progression (CD4 number and viral load) in people living with HIV. Health Psychol. 2007;26:473–480. doi: 10.1037/0278-6133.26.4.473. [DOI] [PubMed] [Google Scholar]
- 44.Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004;291:1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- 45.Bogg T, Roberts BW. Conscientiousness and health-related behaviors: a meta-analysis of the leading behavioral contributors to mortality. Psychol Bull. 2004;130:887–919. doi: 10.1037/0033-2909.130.6.887. [DOI] [PubMed] [Google Scholar]
- 46.Meyer GJ, Finn SE, Eyde LD, et al. Psychological testing and psychological assessment. Am Psychol. 2001;56:128–165. [PubMed] [Google Scholar]
- 47.Adler NE, Boyce T, Chesney MA, et al. Socioeconomic status and health: the challenge of the gradient. Am Psychol. 1994;49:15–24. doi: 10.1037//0003-066x.49.1.15. [DOI] [PubMed] [Google Scholar]
- 48.Ostrove JM, Adler NE, Kuppermann M, Washington AE. Objective and subjective assessments of socioeconomic status and their relationship to self-rated health in an ethnically diverse sample of pregnant women. Health Psychol. 2000;19:613–618. doi: 10.1037//0278-6133.19.6.613. [DOI] [PubMed] [Google Scholar]
- 49.Lodi-Smith J, Jackson J, Bogg T, et al. Mechanisms of health: education and health-related behaviours partially mediate the relationship between conscientiousness and self-reported physical health. Psychol Health. 2010;25:305–319. doi: 10.1080/08870440902736964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Tucker JS, Friedman HS, Wingard DL, Schwartz JE. Marital history at midlife as a predictor of longevity: alternative explanations to the protective effect of marriage. Health Psychol. 1996;15:94–101. doi: 10.1037//0278-6133.15.2.94. [DOI] [PubMed] [Google Scholar]
- 51.House JS, Landis KR, Umberson D. Social relationships and health. Science. 1988;241:540–545. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- 52.Tucker JS, Schwartz JE, Clark KM, Friedman HS. Age-related changes in the associations of social network ties with mortality risk. Psychol Aging. 1999;14:564–571. doi: 10.1037/0882-7974.14.4.564. [DOI] [PubMed] [Google Scholar]
- 53.Hampson SE, Goldberg LR, Vogt TM, Dubanoski JP. Mechanisms by which childhood personality traits influence adult health status: educational attainment and healthy behaviors. Health Psychol. 2007;26:121–125. doi: 10.1037/0278-6133.26.1.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Roberts BW, Caspi A, Moffitt TE. Work experiences and personality development in young adulthood. J Pers Soc Psychol. 2003;84:582–593. [PubMed] [Google Scholar]
- 55.Roberts BW, Bogg T. A longitudinal study of the relationships between conscientiousness and the social environmental factors and substance use behaviors that influence health. J Pers. 2004;72:325–353. doi: 10.1111/j.0022-3506.2004.00264.x. [DOI] [PubMed] [Google Scholar]
- 56.Lodi-Smith J, Roberts BW. Social investment and personality: a meta-analysis of the relationship of personality traits to investment in work, family, religion, and volunteerism. Pers Soc Psychol Rev. 2007;11:68–86. doi: 10.1177/1088868306294590. [DOI] [PubMed] [Google Scholar]
- 57.Roberts BW, Smith J, Jackson JJ, Edmonds G. Compensatory conscientiousness and health in older couples. Psychol Sci. 2009;20:553–559. doi: 10.1111/j.1467-9280.2009.02339.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Roberts BW, Walton KE, Viechtbauer W. Patterns of mean-level change in personality traits across the life course: a meta-analysis of longitudinal studies. Psychol Bull. 2006;132:1–25. doi: 10.1037/0033-2909.132.1.1. [DOI] [PubMed] [Google Scholar]
- 59.Welch D, Poulton R. Personality influences on change in smoking behavior. Health Psychol. 2009;28:292–299. doi: 10.1037/a0013471. [DOI] [PubMed] [Google Scholar]
- 60.Littlefield AK, Sher KJ, Wood PK. Is “maturing out” of problematic alcohol involvement related to personality change? J Abnorm Psychol. 2009;118:360–374. doi: 10.1037/a0015125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Littlefield AK, Sher KJ, Wood PK. A personality-based description of maturing out of alcohol problems: extension with a five-factor model and robustness to modeling challenges. Addict Beh. 2010;35:948–954. doi: 10.1016/j.addbeh.2010.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bogg T, Finn PR, Monsey KE. A year in the college life: Evidence for the social investment hypothesis via trait self-control and alcohol consumption. J Res Pers. 2012;46:694–699. doi: 10.1016/j.jrp.2012.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bogg T. Conscientiousness, the transtheoretical model of change, and exercise: A neo-socioanalytic integration of trait and social-cognitive frameworks in the prediction of behavior. J Pers. 2008;76:775–802. doi: 10.1111/j.1467-6494.2008.00504.x. [DOI] [PubMed] [Google Scholar]
- 64.Bogg T, Voss MW, Wood D, Roberts BW. A hierarchical investigation of personality and behavior: Examining neo-socioanalytic models of health-related outcomes. J Res Pers. 2008;42:183–207. [Google Scholar]
- 65.O'Connor DB, Conner MT, Jones FA, McMillan BRW, Ferguson E. Exploring the benefits of conscientiousness: An investigation of the role of daily stressors and health behaviors. Ann Behav Med. 2009;37:184–96. doi: 10.1007/s12160-009-9087-6. [DOI] [PubMed] [Google Scholar]
- 66.Hampson SE. Personality processes: Mechanisms by which personality traits “get outside the skin”. Annu Rev Psychol. 2012;63:315–339. doi: 10.1146/annurev-psych-120710-100419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Roberts BW, Jackson JJ. Sociogenomic personality psychology. J. Pers. 2008;76:1523–1544. doi: 10.1111/j.1467-6494.2008.00530.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Robinson GE, Grozinger CM, Whitfield CW. Sociogenomics: A social life in molecular terms. Nat Rev Genet. 2005;6:257–271. doi: 10.1038/nrg1575. [DOI] [PubMed] [Google Scholar]
- 69.Dragan WŁ, Oniszczenko W. An association between dopamine D4 receptor and transporter gene polymorphisms and personality traits, assessed using NEO-FFI in a Polish female population. Pers Indiv Differ. 2007;43:531–540. [Google Scholar]
- 70.Reif A, Jacob CP, Rujescu D, et al. Influence of functional variant of neuronal nitric oxide synthase on impulsive behaviors in humans. Arch Gen Psychiat. 2009;66:41–50. doi: 10.1001/archgenpsychiatry.2008.510. [DOI] [PubMed] [Google Scholar]
- 71.Tochigi M, Umekage T, Katoa C, et al. Serotonin 2A receptor gene polymorphism and personality traits: no evidence for significant association. Psychiatr Genet. 2005;15:67–69. doi: 10.1097/00041444-200503000-00011. [DOI] [PubMed] [Google Scholar]
- 72.Tochigi M, Otowa T, Hibin H, et al. Combined analysis of association between personality traits and three functional polymorphisms in the tyrosine hydroxylase, monoamine oxidase A, and catechol-O-methyltransferase genes. Neurosci Res. 2006;54:180–185. doi: 10.1016/j.neures.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 73.Cole AR, Astell A, Green C, Sutherland C. Molecular connexions between dementia and diabetes. Neurosci Biobehav Rev. 2007;31:1046–1063. doi: 10.1016/j.neubiorev.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 74.Roberts BW, DelVecchio WF. The rank-order consistency of personality traits from childhood to old age: A quantitative review of longitudinal studies. Psychol Bull. 2000;126:3–25. doi: 10.1037/0033-2909.126.1.3. [DOI] [PubMed] [Google Scholar]
- 75.Smith ML, Glass GV, Miller TI. The benefits of psychotherapy. Johns Hopkins University Press; Baltimore, MD: 1980. [Google Scholar]
- 76.Clark DM, Ehlers A, McManus F, Hackmann A, et al. Cognitive therapy versus fluoxetine in generalized social phobia: A randomized placebo-controlled trial. J Consult Clin Psychol. 2003;2003;71:1058–1067. doi: 10.1037/0022-006X.71.6.1058. [DOI] [PubMed] [Google Scholar]
- 77.De Fruyt F, Van Leeuwen KG, Bagby RM, Rolland JP, Rouillon F. Assessing and interpreting personality change and continuity in patients treated for major depression. Psychol Assess. 2006;18:71–80. doi: 10.1037/1040-3590.18.1.71. [DOI] [PubMed] [Google Scholar]
- 78.Krasner MS, Epstein RM, Beckman H, Suchman AL, Chapman B, et al. Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA. 2009;2009;302:1284–1293. doi: 10.1001/jama.2009.1384. [DOI] [PubMed] [Google Scholar]
- 79.Magidson J, Lejuez CW, Roberts BW. Theory-driven intervention for changing personality: Expectancy Value Theory, Behavioral Activation and conscientiousness. Dev Psychol. doi: 10.1037/a0030583. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Eccles J. Who am I and what am I going to do with my life? Personal and collective identities as motivators of action. Ed Psychol. 2009;44:78–89. [Google Scholar]
- 81.Dimidjian S, Barrera MR, Martell C, Muñoz RF, Lewinsohn PM. The origins and current status of behavioral activation treatments for depression. Annu Rev Clin Psychol. 2011;2011;7:1–38. doi: 10.1146/annurev-clinpsy-032210-104535. [DOI] [PubMed] [Google Scholar]
- 82.Armitage CJ. Is there utility in the transtheoretical model? Brit J Health Psychol. 2009;14:195–210. doi: 10.1348/135910708X368991. [DOI] [PubMed] [Google Scholar]
- 83.Heckhausen H. Motivation and action. Springer; Berlin: 1991. [Google Scholar]
- 84.Gollwitzer PM. Goal achievement: The role of intentions. Eur Rev Soc Psychol. 1993;1993;4:141–185. [Google Scholar]
- 85.Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. 2nd ed. Guilford Press; New York: 2002. [Google Scholar]
- 86.Gosling SD, Rentfrow PJ, Swann WB. A very brief measure of the Big-Five personality domains. J Res Pers. 2003;37:504–528. [Google Scholar]
- 87.John OP, Srivastava S. The Big Five trait taxonomy: history, measurement, and theoretical perspectives. In: Pervin LA, John OP, editors. Handbook of personality: Theory and Research. 2nd ed. The Guilford Press; New York: 1999. pp. 102–138. [Google Scholar]
- 88.Goldberg LR. The development of markers for the Big-five factor structure. J Pers Soc Psychol. 1992;59:1216–1229. doi: 10.1037//0022-3514.59.6.1216. [DOI] [PubMed] [Google Scholar]
- 89.Saucier G. Mini-Markers: A brief version of Goldberg's unipolar Big-Five markers. J Pers Assess. 1994;63:506–516. doi: 10.1207/s15327752jpa6303_8. [DOI] [PubMed] [Google Scholar]
- 90.Lahey BB. Public health significance of neuroticism. Am Psychol. 2009;64:241–256. doi: 10.1037/a0015309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Mroczek DK, Spiro A. Personality change influences mortality in older men. Psychol Sci. 2007;18:371–376. doi: 10.1111/j.1467-9280.2007.01907.x. [DOI] [PMC free article] [PubMed] [Google Scholar]