Abstract
Ewing's sarcoma, a highly malignant bone tumour, typically affects the pelvis and the long bones of the lower extremities in children and young adults and primary involvement of the skull is rare. Here, we present a case of primary Ewing's sarcoma of the skull with localised swelling in a young adult that involved the frontoparietal region of the skull and was very aggressive in nature. Even with aggressive surgery, the patient had multiple recurrences within 1 month of surgery and ultimately the patient died.
Background
Primary Ewing's sarcoma arising from the skull is very rare.1 2 Only about 1–6% arises in the cranium.1 3 4 Most of the times, this condition has a fatal outcome, although the prognosis of Ewing's sarcoma is improving with radiotherapy and chemotherapy following surgery.1 2 We present a case of primary Ewing's sarcoma in a young adult. -Ray of the skull showed osteolytic lesion of the frontoparietal bones. CT and MRI scan revealed the extracranial and intracranial involvement of the lesion. MRI further showed intradural extension of the lesion. Even after aggressive surgery, there were multiple recurrences and the patient died eventually. The relevant literature is briefly reviewed.
Case presentation
An 18-year-old right-handed boy presented with a rapidly enlarging, paramedian swelling in the frontoparietal region for a duration of 3 months.
On local examination, a non-tender, firm swelling measuring 25 cm×20 cm was noted over the frontoparietal region which was not compressible and fixed to the scalp and underlying bone (figure 1). The patient had no focal neurological deficit.
Figure 1.

Oblique view of the patient showing a large swelling in the frontoparietal region.
Investigations
x-Ray of the skull showed osteolytic changes in the frontoparietal bones (figure 2).
Figure 2.

x-Ray of the skull showing osteolytic areas (black arrow) and a soft tissue opacity overlying the osteolytic area (white arrow).
CT of the brain showed a large enhancing extra-axial lesion in the frontoparietal region with both intracranial and extracranial components and areas of calcification (figure 3).
Figure 3.
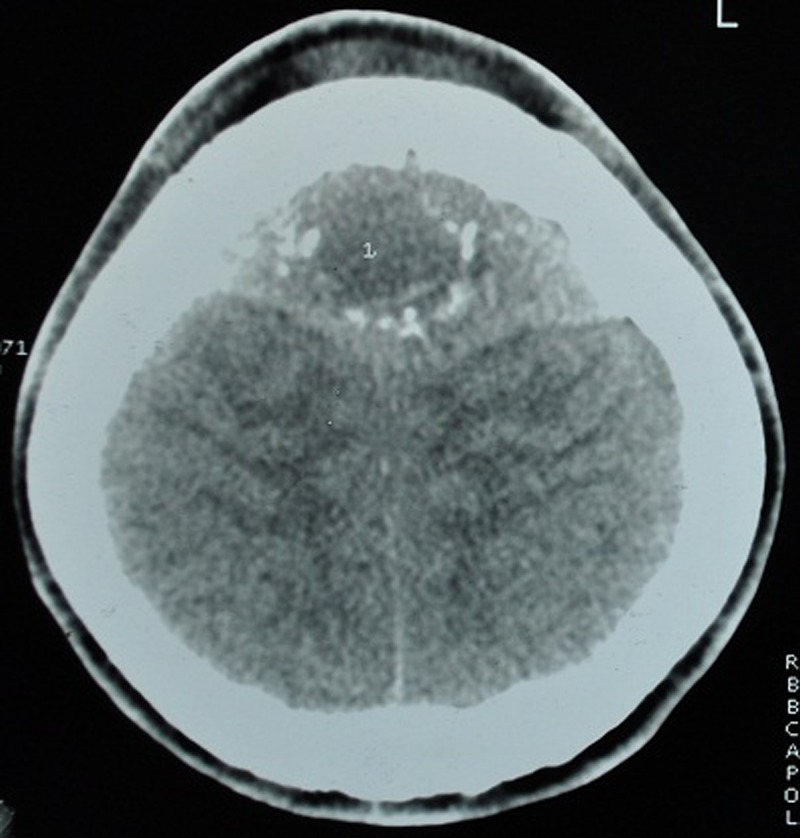
Non-enhanced CT scan of the brain showing areas of calcification.
MRI of the brain revealed a large lobulated extra-axial lesion in the frontoparietal region (more to the left) with extracranial extension through the parietal bone by a narrow pedicle. The lesion was hypointense in T1-weighted image (T1WI) with strong heterogeneous contrast enhancement and of mixed intensity in T2WI. A mushrooming growth from the lesion into the left parietal region was also noted. The lesion was associated with mild perilesional oedema along with mild effacement of the left lateral ventricle and compression of the superior sagittal sinus (figure 4).
Figure 4.
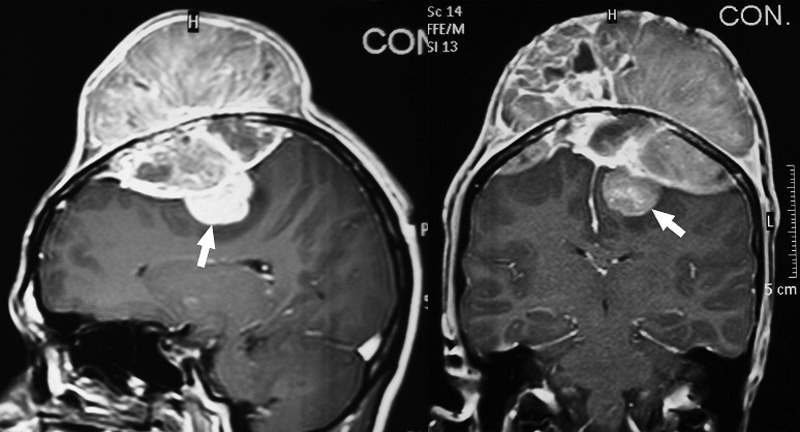
Contrast-enhanced MRI of the brain showing heterogeneously enhancing lesion with both intracranial and extracranial components and the intradural portion (white arrow).
MR venogram revealed obliteration of the superior sagittal sinus and large venous channels arising from the extracranial portion of the tumour draining into the superior sagittal sinus (figure 5).
Figure 5.
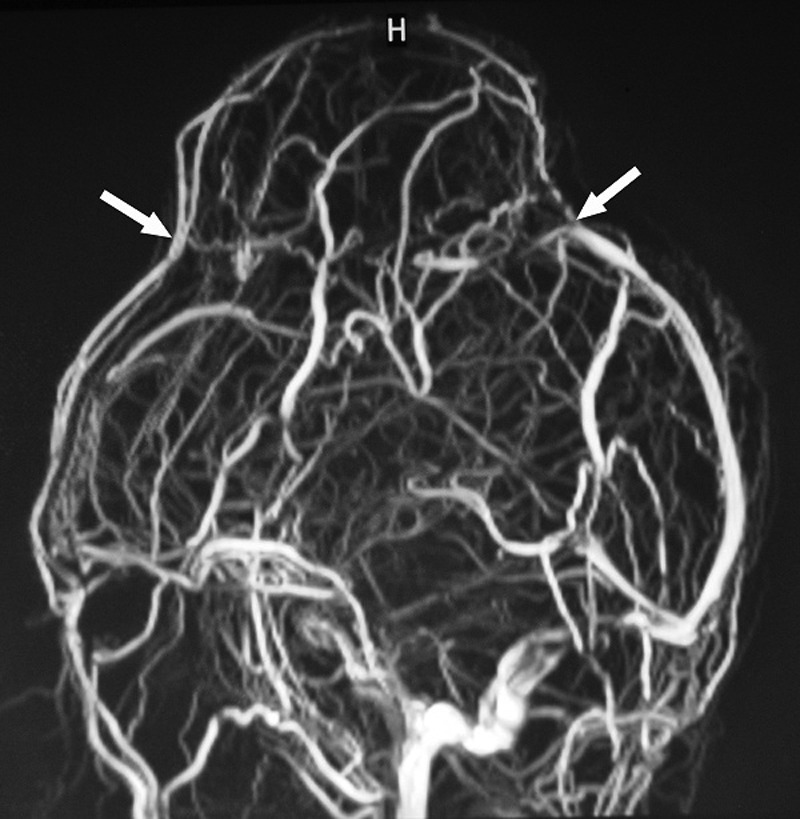
MR venogram (MRV) showing obliteration of the superior sagittal sinus (between the two white arrows) and large venous channels arising from the extracranial portion of the tumour draining into the superior sagittal sinus.
Differential diagnosis
Eosinophilic granuloma, pleomorphic undifferentiated sarcoma.
Treatment
A bifrontoparietal craniotomy and gross total removal of the tumour with duroplasty and cranioplasty was performed. The overlying scalp was found to be free, the bone was eroded and the tumour was found to be mostly extradural and firmly adherent to the dura. A small portion of the tumour was intradural on the left parasagittal region (figure 6).
Figure 6.
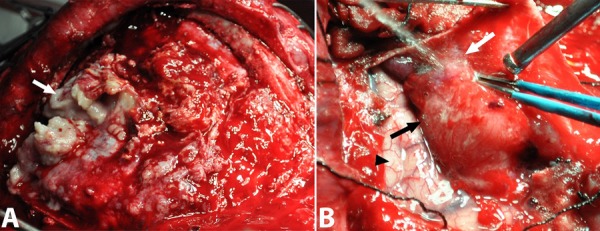
Intraoperative picture showing the extradural component of the tumour (white arrow in A) and the intradural component (black arrow) of the tumour which is densely adherent to the dura (white arrow in B). Normal brain parenchyma is shown (black arrow-head).
Outcome and follow-up
The postoperative period was uneventful. Contrast-enhanced CT on the first postoperative day revealed no residual tumour (figure 7). The histopathology report was suggestive of Ewing's sarcoma (figure 8) and the patient was discharged and advised for radiochemotherapy. The patient who came from a very low socioeconomic background could not afford chemotherapy due to financial constraints as there is no provision of free adjuvant therapy from the Government health system.
Figure 7.
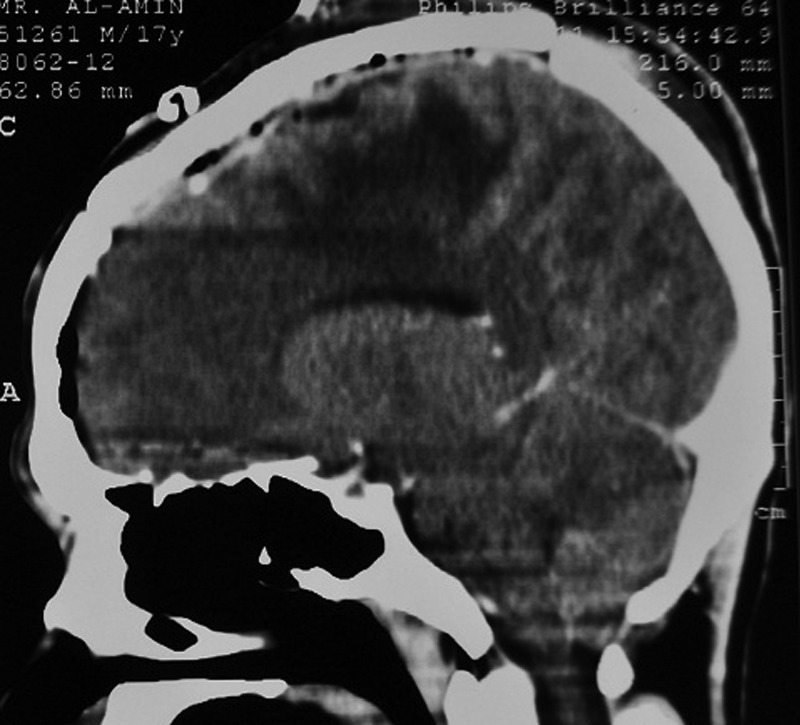
Contrast-enhanced CT of the brain (sagittal section) performed on the first postoperative day showing no residual tumour.
Figure 8.
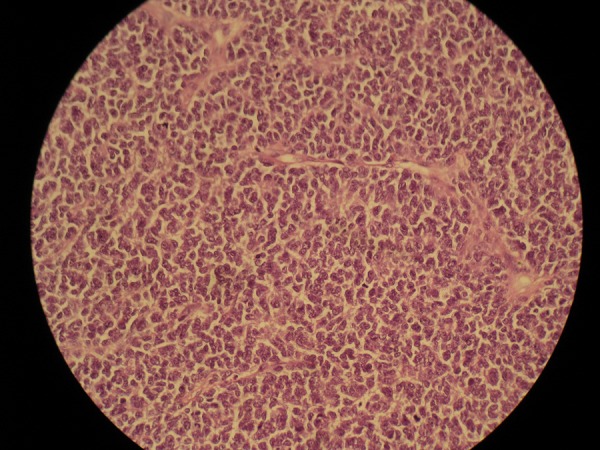
Histopathological image showing a malignant neoplasm composed of small round cells arranged in sheets and nests with intervening dense fibrous stroma.
He came back within a period of 1 month after surgery, before the start of the scheduled radiotherapy, with new swellings in the left parietooccipital and left frontal region. Subsequently, the patient developed painful proptosis of the right eye. A contrast-enhanced CT scan (figure 9) showed multiple contrast-enhancing lesions in the left frontal, left parieto-occipital and the right orbit.
Figure 9.
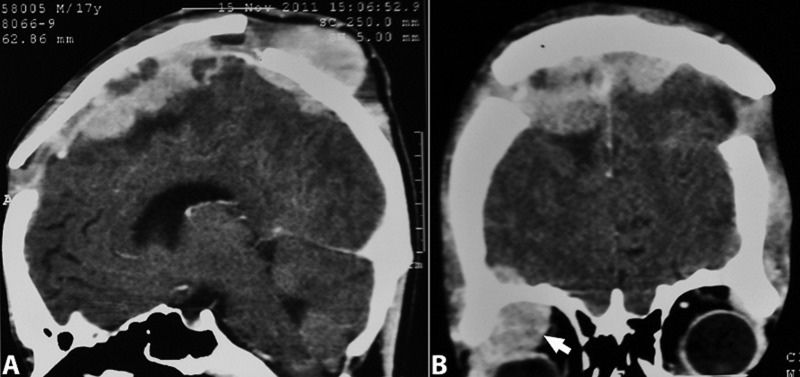
Contrast-enhanced CT of the brain showing multiple recurrences including in the right orbit (white arrow).
Discussion
Ewing's sarcoma is a highly malignant bone tumour that typically affects the pelvis and the long bones of the lower extremities in children and young adults.5 6 It is the second most common malignant bone tumour in childhood (after osteosarcoma).7 Although, primary involvement of the skull is rare representing approximately 1% of all Ewing's sarcomas, metastases to the cranium are not infrequent.3 5–11 The frontal and parietal convexities are relatively common sites.4 8–11 Ewing's sarcoma typically grows extradurally and often reaches a very large size before dural invasion or clinical detection, or both.4 6 12
Symptoms tend to develop as a result of dural invasion, hydrocephalus or raised intracranial pressure. Headaches and scalp swelling are the most common symptoms, and papilloedema is the most common sign.5 13 14 The duration of symptoms before presentation ranges from 2 weeks to 2 years.15 16 Men are affected more than women by a ratio of 1.8 : 1.6 7 Approximately 90% of cases occur in the first two decades of life with the peak incidence being between 5 and 13 years.6 8–11
Our patient was in his second decade and the duration of his symptom was short and except for scalp swelling he had no other symptoms.
Ewing's sarcoma can be considered as an undifferentiated form of peripheral primitive neuroectodermal tumour.12 Histologically, these tumours are characterised by sheets of small round blue cells with an increased nucleus-to-cytoplasm ratio.5 6 12 13 Pseudorosettes may be present, but sheets of cells are more characteristic.6 9 Mitoses are common. Bony spicules may be present, and CD99 and vimentin may be expressed.2 5 6 12 13
The histopathology in our patient revealed a malignant neoplasm composed of small round cells arranged in sheets and nests with intervening dense fibrous stroma.
Plain radiographs of the skull may reveal layering of bone in an ‘onion peel’ arrangement, with layers of bone mottling and erosion, as well as new bone formation.5 6 9 This distinctive periosteal reaction and calcification may also be noted on CT.7 12 In some cases, the tumour will simply be manifested as a lytic lesion on plain radiographs and CT.6 7 Bone healing after chemotherapy is better demonstrated in CT scans.8 MRI may show heterogeneous signal characteristics and avid contrast enhancement of any associated soft tissue component.5 7 13 Ewing's sarcoma exhibits increased radioisotope uptake in nuclear bone scanning images suggesting an ossification process.8 Scintigraphy is particularly helpful in detecting the presence of any extracranial lesions.6–8 17
Plain radiograph in our patient revealed areas of bony erosions but no new bone formation or an onion peel arrangement was seen. The CT scan showed areas of calcification and bony erosions. MRI showed heterogeneous contrast-enhancing lesion in the frontoparietal region with both intracranial and extracranial extensions. It also revealed a small intradural part.
Surgical resection plays an important role in the management of cranial Ewing's sarcoma.2 6 7 13 15 Excision of the tumour should be as radical as possible to minimise tumour mass and increase the effectiveness of adjuvant therapy.8 The dura should be inspected for tumour infiltration, and if infiltration is noted, the dura should be resected as well.6 Local recurrence after resection has been reported.6 13 We did a gross total resection of the tumour along with excision of the involved dura and bone.
Adjuvant therapy after resection, including radiotherapy and chemotherapy, is essential.5 7 The recommended radiotherapeutic method is supervoltage radiation, because it is better tolerated and causes less destruction to normal tissue compared with other forms of radiotherapy.8 Adjunctive chemotherapy with a combination of vincristine, cyclophosphamide, cisplatin, etoposide, dactinomycin and doxorubicin has raised the overall 5-year survival rate from 5–10% to 50–60%.7 12
Various factors indicate a good outcome for patients with cranial Ewing's sarcoma: duration of symptoms for a period of longer than 6 months; absence of fever or systemic symptoms; peripheral localisation of the tumour and absence of metastases; initial lactate dehydrogenase levels of <170 IU/l; leucocyte count of <7000/dl; and lymphocyte count of <2000/dl).10 14 15
Recurrence of Ewing's sarcoma of bone in general is most common within 2 years of initial diagnosis (approximately 80%). Higher rates of local failure are seen in patients older than 14 years who have tumours more than 8 cm in length. Time to recurrence has been considered the most important prognostic factor.11
Although improved by treatment regimens, the prognosis for many patients with Ewing's sarcoma continues to be poor because of early metastasis to the lungs and to other bones. This early metastasis is less common in cases of primary Ewing's sarcoma, and thus primary Ewing's skull tumours are considered to carry a better prognosis.5 7 13 15 Contrary to the literature, this patient carried a dismal outcome.
Learning points.
Primary Ewing's sarcoma of the skull is a rare entity.
Most of the times Ewing's sarcoma is fatal.
Timely surgical intervention followed by radiotherapy and chemotherapy can give a good disease free survival. Although inappropriate adjunctive therapy causes recurrence.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Agrawal A, Dulani R, Mahadevan A, et al. Primary Ewing's sarcoma of the frontal bone with intracranial extension. J Cancer Res Ther (Case Rep) 2009;5:208–9 [DOI] [PubMed] [Google Scholar]
- 2.Bhatoe HS, Deshpande GU. Primary cranial Ewing's sarcoma. Br J Neurosurg (Case Rep Rev) 1998;12:165–9 [DOI] [PubMed] [Google Scholar]
- 3.Kobayashi H, Terasaka S, Yamaguchi S, et al. Primary Ewing's sarcoma: peripheral primitive neuroectodermal tumour of the jugular foramen. Acta Neurochir (Case Reports) 2008;150:817–21 [DOI] [PubMed] [Google Scholar]
- 4.Pfeiffer J, Boedeker CC, Ridder GJ. Primary Ewing sarcoma of the petrous temporal bone: an exceptional cause of facial palsy and deafness in a nursling. Head Neck (Case Rep) 2006;28:955–9 [DOI] [PubMed] [Google Scholar]
- 5.Garg A, Ahmad FU, Suri A, et al. Primary Ewing's sarcoma of the occipital bone presenting as hydrocephalus and blindness. Pediatr Neurosurg (Case Rep) 2007;43:170–3 [DOI] [PubMed] [Google Scholar]
- 6.Desai KI, Nadkarni TD, Goel A, et al. Primary Ewing's sarcoma of the cranium. Neurosurgery (Review) 2000;46:62–8; discussion 8–9 [PubMed] [Google Scholar]
- 7.Li WY, Brock P, Saunders DE. Imaging characteristics of primary cranial Ewing sarcoma. Pediatr Radiol (Case Reports) 2005;35:612–18 [DOI] [PubMed] [Google Scholar]
- 8.Balasubramaniam S, Nadkarni T, Menon R, et al. Primary Ewing's sarcoma of the petroclival bone. J Clin Neurosci (Case Rep) 2008;15:712–14 [DOI] [PubMed] [Google Scholar]
- 9.Desai K, Goel A, Nadkarni TD. Primary petrous bone Ewing's sarcoma. Br J Neurosurg (Case Reports Review) 2000;14:143–5 [DOI] [PubMed] [Google Scholar]
- 10.Erol FS, Ozveren MF, Ozercan IH, et al. Primary Ewing's sarcoma of the occipital bone—case report. Neurol Med Chir (Case Rep) 2001;41:206–9 [DOI] [PubMed] [Google Scholar]
- 11.Salunke PS, Gupta K, Malik V, et al. Primary Ewing's sarcoma of cranial bones: analysis of ten patients. Acta Neurochir (Case Rep) 2011;153:1477–85 [DOI] [PubMed] [Google Scholar]
- 12.Carlotti CG, Jr, Drake JM, Hladky JP, et al. Primary Ewing's sarcoma of the skull in children. Utility of molecular diagnostics, surgery and adjuvant therapies. Pediatr Neurosurg (Case Rep) 1999;31:307–15 [DOI] [PubMed] [Google Scholar]
- 13.Yasuda T, Inagaki T, Yamanouchi Y, et al. A case of primary Ewing's sarcoma of the occipital bone presenting with obstructive hydrocephalus. Childs Nerv Syst (Case Rep Comp Study Rev) 2003;19:792–9 [DOI] [PubMed] [Google Scholar]
- 14.Mishra HB, Haran RP, Joseph T, et al. Primary Ewing's sarcoma of the skull. A report of two cases. Br J Neurosurg (Case Rep) 1993;7:683–6 [DOI] [PubMed] [Google Scholar]
- 15.Kuzeyli K, Akturk F, Reis A, et al. Primary Ewing's sarcoma of the temporal bone with intracranial, extracranial and intraorbital extension. Case report. Neurosurg Rev (Case Rep) 1997;20:132–4 [DOI] [PubMed] [Google Scholar]
- 16.Sharma RR, Netalkar A, Lad SD. Primary Ewing's sarcoma of the greater wing of the sphenoid bone. Br J Neurosurg (Case Rep Rev) 2000;14:53–6 [DOI] [PubMed] [Google Scholar]
- 17.Varan A, Caner H, Saglam S, et al. Primary Ewing's sarcoma of the sphenoid bone: a rare presentation. Pediatr Radiol (Case Rep) 1998;28:311. [DOI] [PubMed] [Google Scholar]


