Abstract
Calculi in the cystic duct remnant are one of the causes of postcholecystectomy syndrome. A 36-year-old woman presented thrice to the casualty department with right upper quadrant pain at an interval of 2 months every time. Ultrasound and CT scan of the abdomen was normal except for echoes in the gallbladder region may be clips. She was treated conservatively and discharged the first two times. The second time, the MR cholangiopancreatography was normal. She had undergone endoscopic retrograde cholangiopancreatography with sphincterotomy with stent in situ outside elsewhere before presenting to us for the third time, which was removed after 6-weeks. The third time, she was taken up for laparoscopic stump exploration, which revealed a stone, which was the cause of her pain. To conclude, stump stone can be a possibility of post cholecystectomy syndrome even after 6 years, and surgeons should be aware of it.
Background
The recurrence of symptoms similar to those before the procedure of cholecystectomy is called postcholecystectomy syndrome. It occurs in 10–40% of patients anywhere between 2 days and 25 years.1–4 The causes include strictures, retained calculi, dropped calculi, tumours, sphincter of Oddi dysfunction and calculi in the cystic duct remnant. The incidence of cystic duct remnant stone after cholecystectomy is less than 2.5%.2,5 Very few case reports and series have been published on this stump stone. Most of the patients presented less than 2 years after cholecystectomy, and most of them were diagnosed before reoperation. In this report, we present how a patient with post cholecystectomy syndromes presented with a stump stone after a long gap of 6 years, and even the best of investigations could not diagnose till reoperation and explain how it was tackled laparoscopically.
Case presentation
A 36-year-old female patient presented with right upper quadrant pain to the casualty department. She had a history of cholecystectomy 6 years back. Examination did not reveal anything except for mild tenderness in the right hypochondrium.
Investigations
Liver function tests and other biological parameters were within normal limits. Ultrasonography was normal except for the hyperechoic region in the gallbladder fossa, probably clips. A straight x-ray abdomen revealed that the calcified area in the gallbladder region might be due to clips. A CT scan of the abdomen also revealed a calcified area in the gallbladder region, probably clips. She was treated conservatively and discharged after her pain subsided. She again came with the same complaints 2 months later. This time, in addition to ultrasound, she was subjected to MRCP, which revealed no abnormality with normal calibre common bile duct.
Treatment
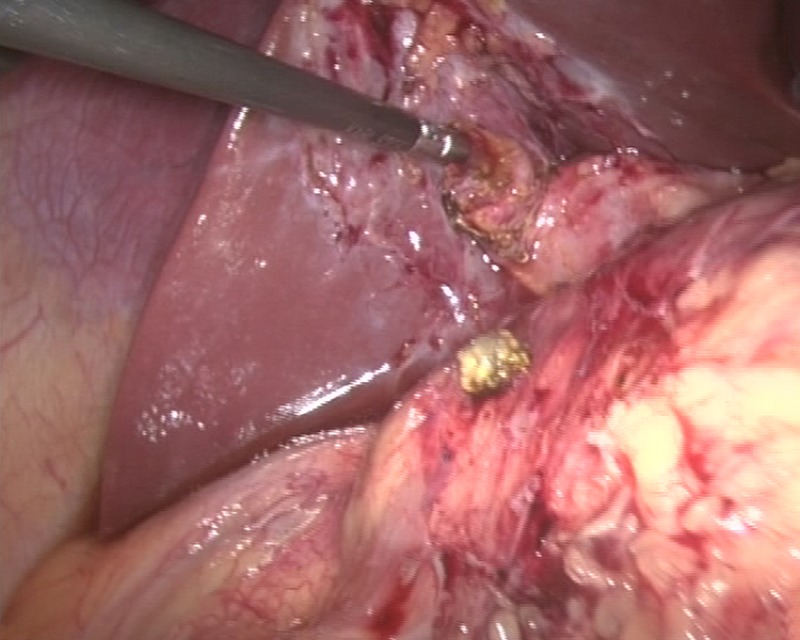
She, however, had undergone endoscopic retrograde cholangiopancreatography (ERCP) with papillotomy and stenting outside elsewhere before presenting to us for the third time, which was removed after 6-weeks. She was fine for another 2-weeks before she was again admitted with the same complaints for the third time. This time, she was planned for diagnostic laparoscopy and reoperation. During laparoscopy, the cystic duct stump was seen to be a bit bulgy, with clips in situ (figure 1). With the idea of performing intraoperative cholangiogram through a cystic duct stump, a small incision was made over the cystic duct stump below the clips, which revealed biliary sludge. In order to clear the sludge, an incision was extended which revealed a calculus at the stump, the hidden culprit of all this drama, which was removed using a blunt grasper (figures 2 and 3). Then, after excising the stump circumferentially, it was closed with intracorporeal suturing with 2–0 vicryl (figure 4).
Figure 1.
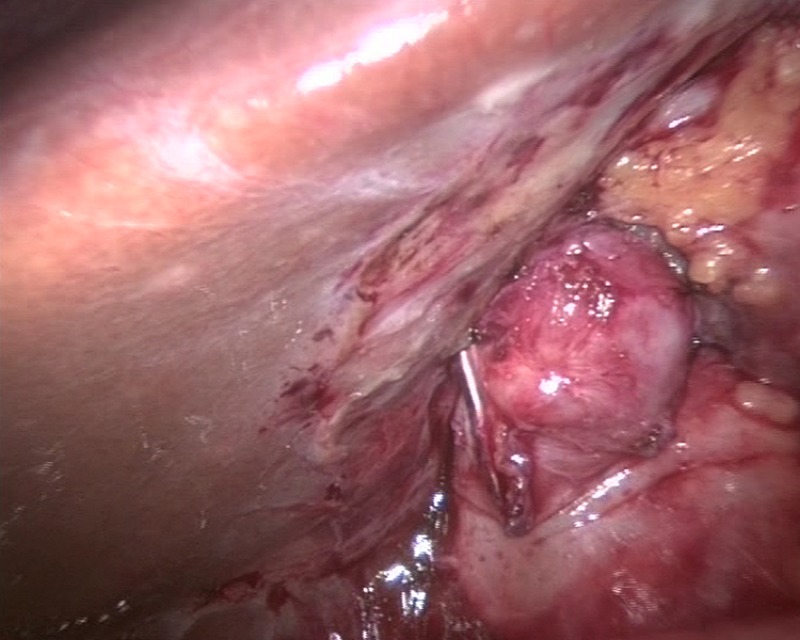
Cystic duct stump with clips in situ.
Figure 2.

Removal of stone using a blunt grasper.
Figure 3.
Stone retrieved from a cystic duct stump.
Figure 4.
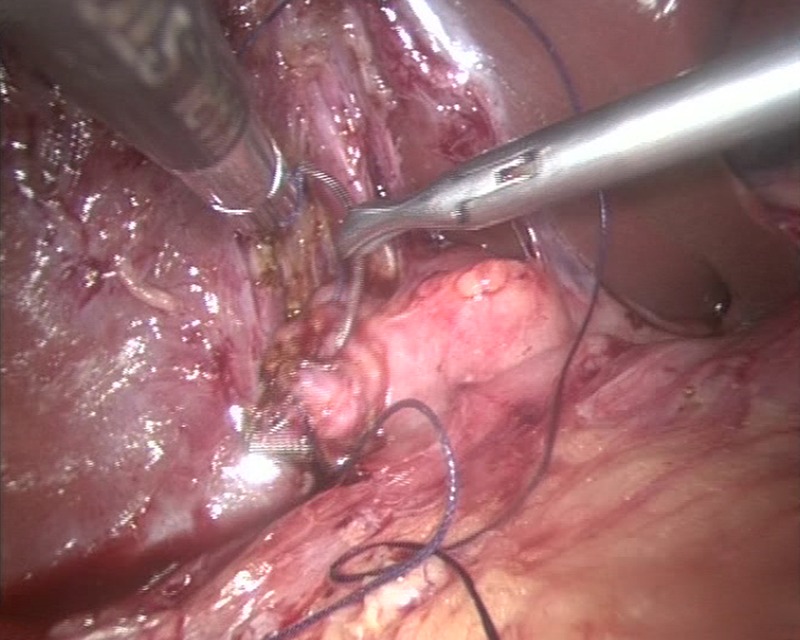
Closure of stump with 2–0 vicryl.
Outcome and follow-up
She recovered very well. The postoperative period was uneventful.
Discussion
Laparoscopic cholecystectomy provides total relief of presurgical symptoms in up to 85% of patients.6 Five per cent of patients may have symptoms similar to the presurgical state, known as the postcholecystectomy syndrome.6 The causes include strictures, retained calculi, dropped calculi, tumours, sphincter of Oddi dysfunction and calculi in the cystic duct remnant.
A stump longer than 1 cm is called a cystic duct remnant. It is more common after laparoscopic cholecystectomy than open because in open surgery the cystic duct is ligated and cut as close to the common bile duct as possible, whereas in laparoscopic cholecystectomy, it is cut closer to the gallbladder to avoid iatrogenic injury to the common bile duct, leaving a longer remnant.
Remnant cystic duct stones are uncommon with an incidence of less than 2.5%.2,5 In 1912, Florcken7 described the first case of a cystic duct remnant containing stones. Rogy et al5 found only 8 who had a stone in the cystic duct or gallbladder remnant in a series of 322 patients. Zhou et al2 found 4 who had a stone in the cystic duct remnant in a series of 371 patients. The presence of stones in a cystic duct or retained gallbladder remnant is a rare cause of postcholecystectomy syndrome, and suspicion is required to make the diagnosis.8–10
In 16% of patients, the cause of postcholecystectomy syndrome was a cystic duct stump stone, as reported by Rozses et al,6 and Bodvall and Overgaard11 found that a cystic duct remnant larger than 1 cm was present in 67% of patients with common bile duct stones.
Walsh et al8 said that the retained gallbladder and cystic duct calculi can be prevented by the accurate identification of the gallbladder cystic duct junction at cholecystectomy in their review of seven cases.
Cystic duct remnant stones are difficult to diagnose. Ultrasonography may occasionally suggest cystic duct stones by showing an acoustic shadow. Walsh et al8 found that ERCP correctly diagnosed the retained stone in only four out of six patients; MRCP was normal and was performed on one patient. Hassan and Vilmann 12 reported that ERCP and MRCP failed to identify two out of three cases of the stump stone. Therefore, determining the accuracy of ERCP and MRCP in detecting cystic duct remnant stones is also difficult. In our case too ultrasonography, ERCP and MRCP failed to identify the stump stone, making diagnosis difficult.
ERCP with basket is the first line of treatment for stump stones. However, its limitations are more to do with the proximal position of the stone in the cystic duct, stone impaction and the smaller diameter of the cystic duct. When ERCP fails, extracorporeal shock-wave lithotripsy (ESWL) with fragmentation of stones and basketting them out, endoscopic biliary laser lithotripsy and repeat laparoscopic cholecystectomy are the other modalities of treatment. The cystic duct remnant and the Calot triangle are surrounded by inflamed scar tissue, after incomplete cholecystectomy, which makes laparoscopic reoperation difficult.13 However, with the increasing experience of surgeons and advances in surgical techniques, repeat cholecystectomy is safe and feasible laparoscopically.
Learning point.
Stump stones are rare and there can be a possibility of postcholecystectomy syndromes even after 6 years; surgeons should be aware of them even though they are difficult for diagnosis, even with the best of investigations. It can be effectively managed laparoscopically by experienced hands .
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Lehman GA, Sherman S. Sphincter of Oddi dysfunction (postcholecystectomy syndrome). In: Yamada T. ed Textbook of gastroenterology. 2nd edn Philadelphia: Lippincott, 1995:2251–62 [Google Scholar]
- 2.Zhou PH, Liu FL, Yao LQ, et al. Endoscopic diagnosis and treatment of post-cholecystectomy syndrome. Hepatobiliary Pancreat Dis Int 2003;2:117–20 [PubMed] [Google Scholar]
- 3.Mergener K, Clavien PA, Branch MS, et al. A stone in a grossly dilated cystic duct stump: a rare cause of postcholecystectomy pain. Am J Gastroenterol 1999;94:229–31 [DOI] [PubMed] [Google Scholar]
- 4.Goenka MK, Kochhar R, Nagi B, et al. Endoscopic retrograde cholangiopancreatography in postcholecystectomy syndrome. J Assoc Physicians India 1996;44:119–22 [PubMed] [Google Scholar]
- 5.Rogy MA, Függer R, Herbst F, et al. Reoperation after cholecystectomy. The role of the cystic duct stump. HPB Surg 1991;4:129–34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rozsos I, Magyarodi Z, Orban P. Cystic duct syndrome and minimally invasive surgery. Orv Hetil 1997;138:2397–401 [PubMed] [Google Scholar]
- 7.Flörcken H. Gallenblasenregeneration mit steinrecidiv nach cholecystectomie. Deutsch Z Chir 1912;113:604 [Google Scholar]
- 8.Walsh RM, Ponsky JL, Dumot J. Retained gallbladder/cystic duct remnant calculi as a cause of postcholecystectomy pain. Surg Endosc 2002;16:981–4 [DOI] [PubMed] [Google Scholar]
- 9.Tantia O, Jain M, Khanna S, et al. Post cholecystectomy syndrome: role of cystic duct stump and re-intervention by laparoscopic surgery. J Minim Access Surg 2008;4:71–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Palanivelu C, Rangarajan M, Jategaonkar PA, et al. Laparoscopic management of remnant cystic duct calculi: a retrospective study. Ann R Coll Surg Engl 2009;91:25–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bodvall B, Overgaard B. CF duct remnant after cholecystectomy: incidence studied by cholegraphy in 500 cases, and significance in 103 reoperations. Ann Surg 1966;163:382–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hassan H, Vilmann P. Insufficient cholecystectomy diagnosed by endoscopic ultrasonography. Endoscopy 2004;36:236–8 [DOI] [PubMed] [Google Scholar]
- 13.Rozsos I, Magyaródi Z, Orbán P. Cystic duct syndrome and minimally invasive surgery. (Hungarian). Orv Hetil 1997;138:2397–401 [PubMed] [Google Scholar]


