Abstract
Objective
To investigate the changes of ankle strength and range of motion with aging and which of the ankle strength and range of motion are contributed to balance.
Methods
Sixty healthy people (24 men and 36 women) have undergone tests for ankle strength and range of motion, using Biodex System 4 Pro; a one-leg balance, including postural sway and stability index using a Balance System; in which data were collected in a self-reported Desmond fall risk questionnaire.
Results
Participants are classified into 3 groups by age (group 1, 20-40 years; group 2, 40-65 years; group 3, over 65 years). Stability index and postural sway is significantly increased with aging. Ankle plantarflexor strength and ankle eversion range of motion is significantly decreased with aging. Pearson's correlation revealed that ankle plantarflexor strength is significantly correlated with anterior/posterior sway, and ankle eversion range of motion is significantly correlated with medial/lateral sway in the aged group (over 65 years).
Conclusion
Stability, ankle plantarflexor strength, and eversion range of motion is declined with aging. In addition, strength of ankle plantarflexor and eversion range of motion is significantly correlated with balance stability. Further studies are needed for programs to improve the strength of plantarflexor, and range of motion of eversion of the ankle are beneficial in improving balance, stability, and prevention of falling in the elderly.
Keywords: Balance, Ankle strength, Ankle range of motion, Aging, Fall risk
INTRODUCTION
The population of people age 65 and above is rising dramatically in modern society. Facing an unprecedented pace of population aging, there is a growing concern about life quality for the elderly. Nearly one-third of the elderly people living in a community fall each year and the fallen rates are rising with age [1]. Falls are a major public health problem in aging adults. Falls and fall-related injuries are a major cause of morbidity and mortality in the elderly. Related injuries, such as fractures, can have a detrimental effect on daily function and independent ambulation in later life. In addition, fear of falling can limit physical and social activities; consequentially, lowering quality of life. Most falls in elderly people are associated with multiple risk factors, such as weakness of muscles, reducing balance control, gait disorder, number of medications and environmental factors [1,2].
The maintenance of balance is a complex phenomenon that is influenced by multiple neural and musculoskeletal factors [3]. Balance is maintained through a complex process involving sensory detection of body motions, integration of sensorimotor information within the central nervous system, and execution of appropriate musculoskeletal responses [4]. Maintaining balance, which is the ability to maintain an upright position during quiet standing, is necessary for successful performance of daily life tasks [5]. However, the ability of postural control is declining according to aging [6]. Colledge et al. [7] demonstrated that postural sway increased linearly with age, but was not affected by gender at any age.
Adequate postural control depends on the integration of vestibular, visual, and somatosensory information of the body motion. Advancing age accompanied with a generalized reduction of the vision and vestibular function. Moreover, Lord et al. [5] reported that deterioration of postural stability related to aging is associated with reduced sensation in the lower limbs as measured by joint position, tactile, and vibration sensitivities. It not only affects sensorimotor functions, but also muscle strength and joint movement associated with declining in age [8]. Bennell and Goldie [9] demonstrated that particular range of motion (ROM) of the ankle is an important risk factor of reducing postural stability. Grimston et al. [8] and Vandervoort et al. [10] reported that an average decrement of ankle joint ROM was greater in females than males with aging. However, available literature on relationships between ankle strength and ROM variables, and balance is limited in a population of Korean adults.
The aim of this study is to investigate the changes in strength and ROM of ankle with aging and to identify the ankle strength and ROM that significantly contribute to balance. In addition, we tried to identify which ankle strength and ROM that could be specifically targeted as part of an intervention program to improve balance and prevent falls in the elderly group over the age of 65.
MATERIALS AND METHODS
Subjects
Participants for this study were recruited as part of a randomized controlled trial, made up of 60 healthy subjects between 20-74 years of age composed of 24 males and 36 females. People who have neurologic disease, musculoskeletal problem, visual problem or vestibular disease were excluded. Participants were classified into 3 groups (group 1, 20-40 years; group 2, 40-65 years; group 3, over 65 years) with 20 subjects to evaluate the changes in ankle strength, ROM, and balance according to aging. The mean age of group 1 was 27.3±3.7 years, group 2 was 49.8±9.6 years, and group 3 was 70.4±8.2 years (Table 1).
Table 1.
General characteristics of subjects
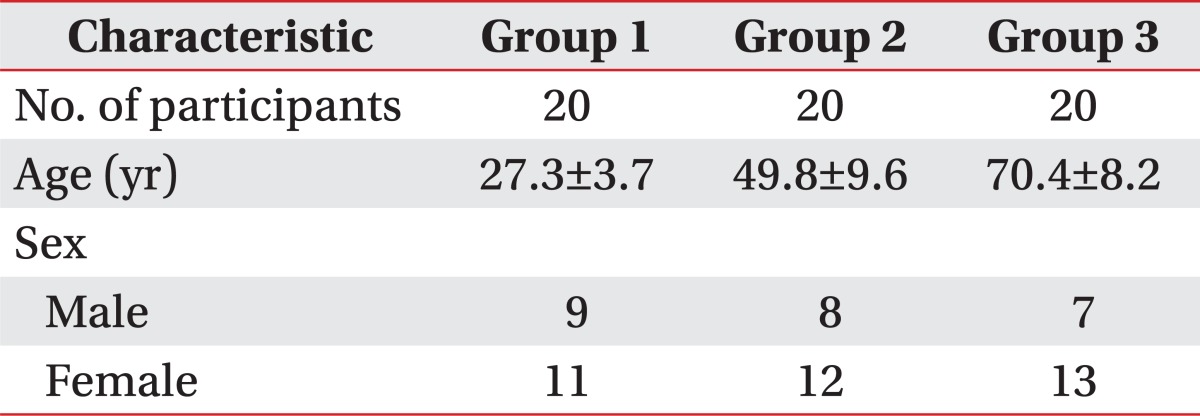
Each group is divided by age: group 1, 20-40 years; group 2, 41-65 years; group 3, >65 years. Compared among the groups by one-way analysis of variance.
Methods
Biodex System 4 Pro (Biodex Medical System, Shirley, NY, USA) was used to measure ankle strength and ROM. Ankle muscles responsible for dorsiflexion, plantarflexion, inversion, eversion were assessed and maximal ankle passive ROM of dorsiflexion, plantarflexion, inversion, and eversion were measured. Ankle strength and ROM were assessed with the participant seated in 90 degrees knee flexion, ankle in neutral position, while keeping the back straight on a chair with a Velcro strap attached to a strain gauge placed around the lower leg and foot. Ankle axis was on the same line as equipment axis, and the handles were held by both hands (Fig. 1). Before testing, all participants had done a stretching exercise for 5 minutes, prior to performing strength and ROM practices 5 times. Visual biofeedback was applied during repeated practice session. Ankle strength was recorded in Newton meters (Nm) of isometric power of both ankles. Each ankle strength exercises were assessed 5 times. Each subject was encouraged to contract fast and to hold each contraction for 5 seconds, and they were given 5 seconds of rest in between trials. The mean value of maximal strength in isometric contraction is assessed. Ankle joint ROM of both sides were measured one time and recorded in degrees at maximal range of passive movement. Each ankle of dominant and nondominant sides was used as independent variables.
Fig. 1.

Isometric strength of ankle dorsiflexor, plantarflexor, everter, and inverter are measured by Biodex System 4 Pro.
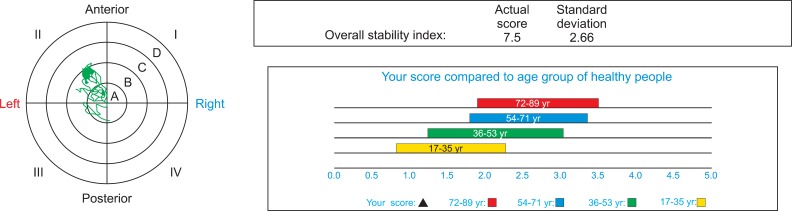
For quantitative evaluation of balance, Balance System (Biodex Medical System) was used. All participants underwent a one-leg standing test of both lower extremities for 20 seconds with their eyes open (Fig. 2). The center of pressure (COP) was shown by a point on the screen. Body sway was quantified by displacement of the COP in the anterior/posterior (AP) and medial/lateral (ML) direction; and the overall stability index (OSI) was measured by force platform. Force platform surface was divided into 2,000 pixels wide and long. Extent of sway was recorded as the maximal displacement in pixels in the AP direction and the ML direction. OSI means displacement of COP according to tilting angles of the force plate to represent sway index.
Fig. 2.
Center of gravity sway and overall stability index are measured using Balance System.
Self-reported Desmond fall risk questionnaire was collected from all participants to evaluate risk of falls. Desmond questionnaire consists of 15 questions about experiences of falls and falling sensations.
Statistical analysis
One-way analysis of variance (ANOVA) was used to compare ankle strength and ROM between each group, and Spearman's correlation coefficients were calculated to evaluate the relationship between ankle strength, ROM, and maintenance of balance in each group. Statistical analysis was carried out with SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). A significance level of p<0.05 was considered.
RESULTS
Age related changes in ankle strength and ROM
Muscle strength of ankle dorsiflexion, plantarflexion, inversion, and eversion were declined with aging. Out of these, only the strength of plantarflexor was significantly decreased in this study (Table 2). Maximum passive ankle ROM of dorsiflexion, plantarflexion, inversion, and eversion were declined with aging. Out of all directions, only eversion ROM was significantly decreased in this study (Table 3).
Table 2.
Strength of the ankle
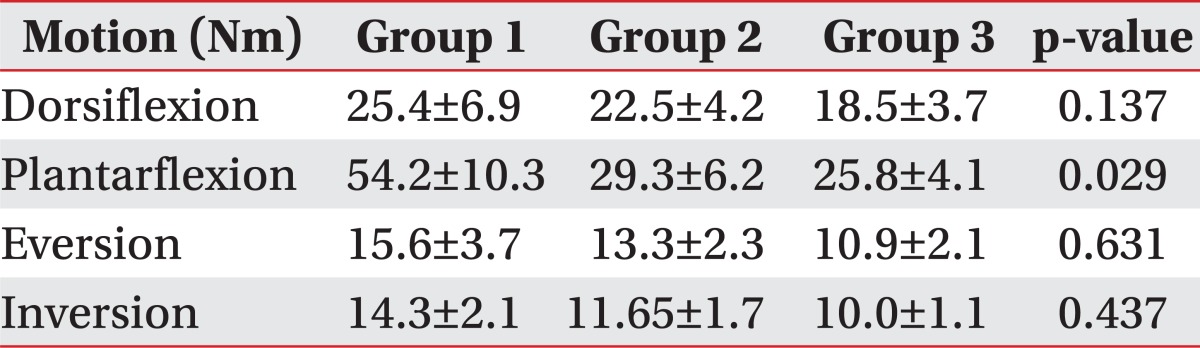
Values are presented as mean±standard deviation.
Each group is divided by age: group 1, 20-40 years; group 2, 41-65 years; group 3, >65 years. Compared among the groups by one-way analysis of variance.
Table 3.
Range of motion of ankle
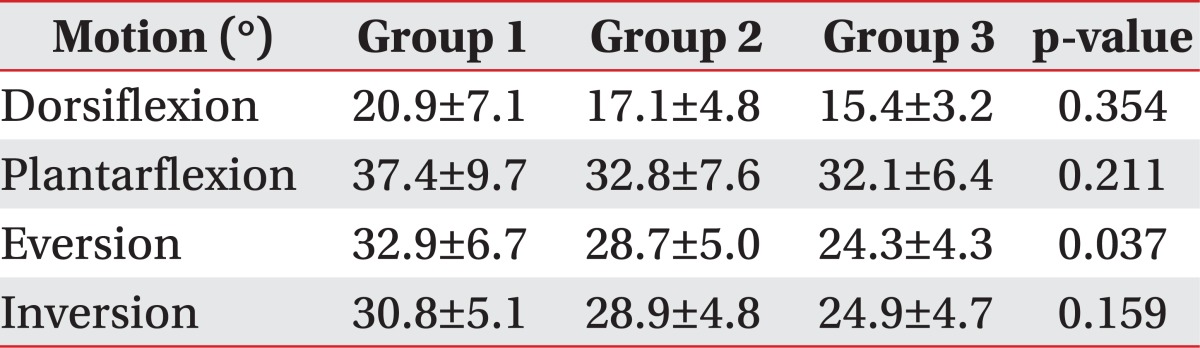
Values are presented as mean±standard deviation.
Each group is divided by age: group 1, 20-40 years; group 2, 41-65 years; group 3, >65 years. Compared among the groups by one-way analysis of variance.
Age related changes in maintenance of balance and fall risk
AP postural sway and ML postural sway were extended with aging. Especially increments of AP sway had statistical significance in this study. OSI and Desmond score (DS) were increased with aging. Only DS was significantly increased in this study (Table 4).
Table 4.
Balance index of subject
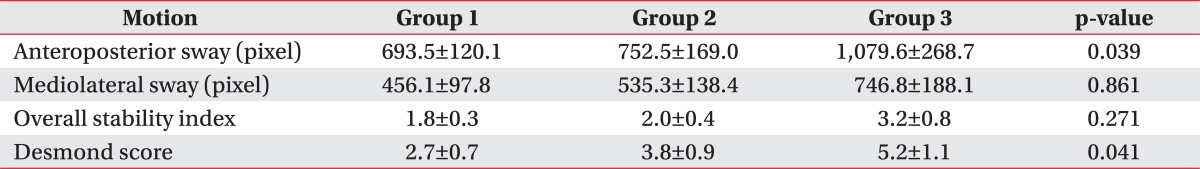
Values are presented as mean±standard deviation.
Each group is divided by age: group 1, 20-40 years; group 2, 41-65 years; group 3, >65 years. Compared among the groups by one-way analysis of variance (ANOVA).
Correlations between ankle variables and balance related to aging
Correlations between the ankle strength, ROM, and the balance are shown in Table 5. There weren't any strong correlation between ankle strength, ROM variables, and balance in groups 1 and 2. The ankle plantarflexor strength was associated with AP postural sway (p<0.05) and maximum ankle eversion ROM was associated with ML postural sway (p<0.05) in group 3. Both AP and ML sway was correlated with DS (p<0.05).
Table 5.
Correlation between stability index and strength and range of motion of ankle related to aging
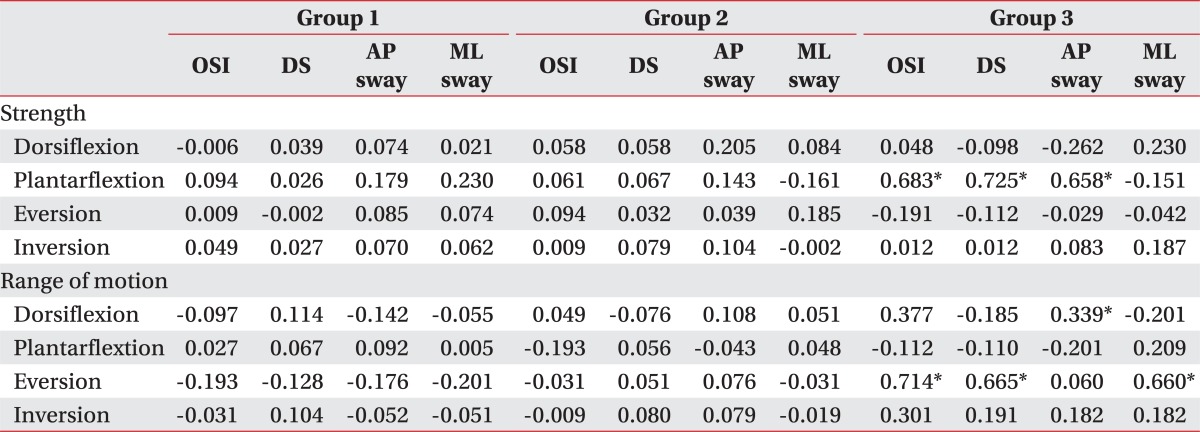
Values are correlation coefficient. Each group is divided by age: group 1, 20-40 years; group 2, 41-65 years; group 3, >65 years.
OSI, overall stability idex; DS, Desmond score; AP, anteroposterior; ML, mediolateral.
*p<0.05.
DISCUSSION
Balance is the ability to maintain equilibrium and orientation in a gravitational environment. The maintenance of balance is influenced by multifactorial sensorimotor factors, including visual acuity, vestibular function, peripheral sensation, cerebellar function, and muscle strength of both lower extremities. Several neuromuscular diseases and drugs affect impairment of balance. To maintain balance, kinesthetic sense from proprioceptor support postural control. Kinesthetic sense information intends joint position and motion, such as tension or pressure of muscle and ligament, for keeping joint position and velocity or acceleration during joint movement. This kinesthetic information integrates with visual and vestibular sensation to maintain balance.
Berg Balance Scale, functional reach test, Tinetti performance oriented mobility assessment, get up and go test, are clinical validated balance tests for the elderly. Woo et al. [11] demonstrated that balance ability was decreased according to the increase in age, tested by Berg balance scale, Tinetti performance oriented mobility assessment and one-leg standing. However, these clinical balance tests are less objective, nevertheless, commonly used in practice because it is easier to perform. Therefore, there is a need of methods to evaluate the objective and quantitative. Balance System (Biodex Medical System), a device we used in this study can measure COP. The displacement of COP represents criterion of stability.
Laughton et al. [12] reported that elderly fallers demonstrated significantly greater amounts of sway in the AP direction and greater muscle activity during quiet standing compared with the young subject, and Lim et al. [13] demonstrated low directional control and low on-axis velocity in front/back rhythmic weight shift than right/left in older groups. The findings of this study also demonstrate that both AP sway and ML sway were increased with age, but only AP sway has significantly increased with age. According to the increase of age, keeping of static balance was considered to increase in the AP sway. The findings of this study demonstrated that OSI and DS were increased with age. Only DS is significantly increased with increasing age.
Muscle weakness is an important factor associated with falls in the elderly. There have been reports of hip abductor, knee flexor, knee extensor or ankle dorsiflexor weakness related to an older adult's fallen status [1,14]. Hip abductor has an important role in maintaining body alignment at the initial stance phase, as they provide lateral support at hip joint. Knee extensors provide eccentric contraction needed during the loading phase of the gait cycle. Knee flexor and ankle dorsiflexors are involved in lifting the lower limb during the swing phase of gait, thereby allowing sufficient clearance of the toes over the ground; which is important in the prevention of tripping [15]. In a contrary, Spink et al. [16] reported that age related changes of foot problems are common and it impairs balance and increase the risk of falls. Particularly, hallux plantarflexor strength and ROM of ankle inversion-eversion were the variables most frequently associated with the balance and functional ability in older people [16]. Our findings of this study demonstrate that ankle plantarflexor strength is significantly declined with aging and there is a significant association between ankle plantarflexor strength and AP sway of COP and OSI in the elderly. Plantarflexor has a role in supporting weight of body and providing stability at the ankle and feet for standing and gait, whereas dorsiflexor muscles against gravity during the swing phase of gait clear the feet from the floor. Our findings suggest that static balance may be related to plantarflexor strength more than dorsiflexor strength.
Not only strength of muscles, but also joint movement is influencing maintenance of balance. Amundsen [17] reported that most of the ROM in lower extremities are reduced with age. Woo et al. [11] demonstrated that the flexibilities of lower extremities were decreased according to an increase in age. Flexibility of the ankle joint, in particular, showed the strongest correlation with clinical balance score with age. Horak et al. [18] reported that ankle strength and flexibility are required when the body is exposed to gravity or external force at first. The findings of this study demonstrate that ankle eversion ROM is significantly declined with aging and there is a significant association between ankle eversion ROM and ML sway of COP and OSI in elderly. Our findings confirmed significant decline in balance due to aging in consequence of muscle weakness and motion limitation of the ankle. This may be a result that ankle strength and ROM acts as an important role of postural control at the initial of stance phase. Therefore, impairment of balance in healthy older adults has been related to muscle weakness and impairment of ROM in the ankle. However, strength and ROM of hip and knee joints were not assessed in this study. As such, additional research is needed to evaluate the correlations between hip and knee strength and ROM and balance in older adults.
In our study, subjects had only 5 seconds rest between isometric contractions. Due to shortness of resting period, this study has the limitation that muscle fatigue cannot be excluded in each trial. Another limitation of this study is that each ankle of dominant and nondominant sides was used as independent variables. The dominant side may affect correlation in strength and balance. Further, balance removed visual input is not assessed and that variance of visual compensation is unaccounted for. Also, further research are required to establish whether intervention programs that include strengthening and stretching exercises for the ankle may achieve improvement in balance and functional ability, thereby play a role in the prevention of falls and loss of independence in older people.
In conclusion, this study shows that ankle strength, ROM and control of balance were declining and risk of falls was increasing with aging. In particular, weakening of ankle plantarflexor and decline of ankle eversion ROM are important determinants of balance and falls in elderly people. Therefore, it is necessary to assess ankle strength and ROM, while evaluating falling risks. In addition, further studies are needed for intervention programs to improve the strength and flexibility of the ankle are beneficial in improving balance and prevention of falls in the elderly.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319:1701–1707. doi: 10.1056/NEJM198812293192604. [DOI] [PubMed] [Google Scholar]
- 2.Campbell AJ, Borrie MJ, Spears GF. Risk factors for falls in a community-based prospective study of people 70 years and older. J Gerontol. 1989;44:M112–M117. doi: 10.1093/geronj/44.4.m112. [DOI] [PubMed] [Google Scholar]
- 3.Brody LT. Balance impairment. In: Hall CM, Brody LT, editors. Therapeutic exercise: moving toward function. Philadelphia: Lippincott Williams & Wilkins; 1999. pp. 112–127. [Google Scholar]
- 4.Nashner LM. Sensory neuromuscular and biomechanical contributions to human balance. In: Duncan PW, editor. Balance: proceedings of the APTA Forum; 1989 Jun 13-15; Nashville, TN. Alexandria, VA: American Physical Therapy Association; 1990. [Google Scholar]
- 5.Lord SR, Clark RD, Webster IW. Postural stability and associated physiological factors in a population of aged persons. J Gerontol. 1991;46:M69–M76. doi: 10.1093/geronj/46.3.m69. [DOI] [PubMed] [Google Scholar]
- 6.Daubney ME, Culham EG. Lower-extremity muscle force and balance performance in adults aged 65 years and older. Phys Ther. 1999;79:1177–1185. [PubMed] [Google Scholar]
- 7.Colledge NR, Cantley P, Peaston I, Brash H, Lewis S, Wilson JA. Ageing and balance: the measurement of spontaneous sway by posturography. Gerontology. 1994;40:273–278. doi: 10.1159/000213596. [DOI] [PubMed] [Google Scholar]
- 8.Grimston SK, Nigg BM, Hanley DA, Engsberg JR. Differences in ankle joint complex range of motion as a function of age. Foot Ankle. 1993;14:215–222. doi: 10.1177/107110079301400407. [DOI] [PubMed] [Google Scholar]
- 9.Bennell KL, Goldie PA. The differential effects of external ankle support on postural control. J Orthop Sports Phys Ther. 1994;20:287–295. doi: 10.2519/jospt.1994.20.6.287. [DOI] [PubMed] [Google Scholar]
- 10.Vandervoort AA, Chesworth BM, Cunningham DA, Paterson DH, Rechnitzer PA, Koval JJ. Age and sex effects on mobility of the human ankle. J Gerontol. 1992;47:M17–M21. doi: 10.1093/geronj/47.1.m17. [DOI] [PubMed] [Google Scholar]
- 11.Woo YK, Hwang JH, An J, Park H, Kim YH, Lee PK, et al. Effect of characteristics of joint motion of lower extremity according to aging on balance in elderly. J Korean Acad Rehabil Med. 2005;29:109–118. [Google Scholar]
- 12.Laughton CA, Slavin M, Katdare K, Nolan L, Bean JF, Kerrigan DC, et al. Aging, muscle activity, and balance control: physiologic changes associated with balance impairment. Gait Posture. 2003;18:101–108. doi: 10.1016/s0966-6362(02)00200-x. [DOI] [PubMed] [Google Scholar]
- 13.Lim KB, Na YM, Lee HJ, Joo SJ. Comparison of postural control measures between older and younger adults using balance master system. J Korean Acad Rehabil Med. 2003;27:418–423. [Google Scholar]
- 14.Whipple RH, Wolfson LI, Amerman PM. The relationship of knee and ankle weakness to falls in nursing home residents: an isokinetic study. J Am Geriatr Soc. 1987;35:13–20. doi: 10.1111/j.1532-5415.1987.tb01313.x. [DOI] [PubMed] [Google Scholar]
- 15.Macrae PG, Lacourse M, Moldavon R. Physical performance measures that predict faller status in community-dwelling older adults. J Orthop Sports Phys Ther. 1992;16:123–128. doi: 10.2519/jospt.1992.16.3.123. [DOI] [PubMed] [Google Scholar]
- 16.Spink MJ, Fotoohabadi MR, Wee E, Hill KD, Lord SR, Menz HB. Foot and ankle strength, range of motion, posture, and deformity are associated with balance and functional ability in older adults. Arch Phys Med Rehabil. 2011;92:68–75. doi: 10.1016/j.apmr.2010.09.024. [DOI] [PubMed] [Google Scholar]
- 17.Amundsen LR. Effects of age on joints and ligaments. In: Kauffman TL, editor. Geriatric rehabilitation manual. New York: Churchill Livingstone; 1999. pp. 14–16. [Google Scholar]
- 18.Horak FB, Shupert CL, Mirka A. Components of postural dyscontrol in the elderly: a review. Neurobiol Aging. 1989;10:727–738. doi: 10.1016/0197-4580(89)90010-9. [DOI] [PubMed] [Google Scholar]