Abstract
Plantaris muscle is accessory plantar flexor of calf, a vestigial muscle of triceps surae complex. Its importance lies in the fact that its rupture cans mimic deep vein thrombosis (DVT). Sometimes when there is rupture of Achilles tendon, intact plantaris can still cause plantar flexion at ankle presenting a confusing picture. We present one such case of plantaris rupture confused by radiology resident with DVT. A 51-year-old man had a feeling as if kicked in back of calf along with a snapping sound and severe pain while playing tennis. On seeing fluid between muscle plane and a hypoechoic structure radiology resident labelled it DVT. MRI suggested ruptured plantaris as fluid and muscle stump were seen between gastronemius and soleus. Patient was treated conservatively with rest, ice compression and elevated leg and showed significant reduction in pain and swelling.
Background
Plantaris muscle is a variably developed accessory plantar flexor of calf, a vestigial muscle of triceps surae complex. Its tendon is long and thin and is often confused with nerve and hence at times referred as ‘fool's nerve’ or ‘freshmen's nerve.’ It is absent in about 7–20% of limbs1 and is used by surgeons for tendon grafts. Its importance lies in the fact that its rupture can mimic DVT, a more serious condition, both clinically and radiologically. Moreover, sometimes when there is rupture of Achilles tendon, intact plantaris can still cause plantar flexion at ankle presenting a confusing picture. Hence, it is important to get familiar with this condition.
Case presentation
A 51-year-old man was playing lawn tennis when he suddenly had a feeling as if someone had kicked him in the back of calf. He heard a snapping sound and experienced severe pain which progressed over the next 2–3 days. He also developed swelling along with bruising which spread upto the ankle.
Investigations
Ultrasound (US) of the calf was advised which was completed during emergency hours by a resident doctor. He saw some fluid in the muscle planes and a linear hypoechoic structure in it and labelled it as a case of DVT. The clinician, however, was sceptical and sent the patient for MRI of the calf in the morning. On MRI examination, there was a fluid collection between the medial head of gastrocnemius and soleus along with an ill-defined mass-like structure in this space isointense to muscle (figure 1A,B)). It was thought to represent ruptured retracted plantaris muscle. In addition, there was a hyperintense signal in the medial head of gastrocnemius on T2-weighted images without any fibre discontinuity suggestive of strain (figure 2 A,B)). The popliteal arteries and veins were normal. US was again reviewed in the light of MRI findings and there was now a total agreement between US and MRI findings. Doppler examination ruled out DVT. It was diagnosed radiologically as a case of plantaris rupture along with strain of medial head of gastrocnemius (tennis leg).
Figure 1.
(A and B) Short tau inversion recovery coronal images of B/L calves showing fluid in the plane between gastrosoleus and retracted proximal (red arrow) and distal (yellow arrow) stumps of ruptured plantaris muscle of right leg.
Figure 2.
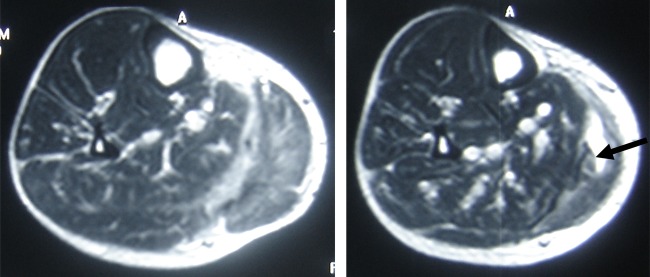
(A and B) T2-weighted axial images of calf showing fluid in the plane between gastrosoleus, hyperintensity in medial head of gastrocnemius suggesting strain and retracted stump of ruptured plantaris (arrow).
Differential diagnosis
Deep vein thrombosis is the main differential diagnosis both clinically as well as radiologically.
Ruptured Baker's cyst.
Treatment
The patient was treated conservatively. He was advised rest, ice compression and elevated leg for 3 days with adhesive tape to prevent ankle plantar flexion.
Outcome and follow-up
There was significant reduction in the pain and swelling. He was slowly put on to normal function and then built-up regimen. The patient is doing well on 1 year of follow-up.
Discussion
Plantaris is a vestigial muscle of triceps surae complex originating from the distal aspect of lateral supracondylar line of femur (superior and medial to the origin of the lateral head of gastrocnemius) as well as from oblique popliteal ligament in posterior aspect of knee. It courses distally in medial-inferior direction. The muscle belly is situated between popliteus, anteriorly and lateral head of gastrocnemius, posteriorly in proximal third of leg. The myotendinous junction is mostly at the level of origin of soleus muscle from tibia in the proximal leg. The tendon forms medial border of the muscle belly and courses between the medial head of gastrocnemius and soleus in mid portion of leg. The tendon attaches either independently to the calcaneus anteromedial to the Achilles tendon or merges with Achilles tendon proximal to the insertion.
Plantaris muscle traverses two joints (knee and ankle) which makes it prone to rupture. The most common mechanism of rupture is dorsiflexion of the ankle with knee in full extension which results in simultaneous active contraction and passive stretching of the muscle.2 It is very common in tennis players and hence the term ‘tennis leg’ was coined by Powell3. In our patient also, it happened when he was playing tennis though he was not a tennis player.
There has always been a controversy in the literature regarding the term ‘tennis leg’. Some orthopaedicians attribute it to ruptured plantaris while others totally deny such entity and attribute it to partial rupture/strain of the medial head of gastrocnemius. Allard et al4 were the first to demonstrate rupture of the plantaris muscle of two patients. The first surgically confirmed isolated rupture of plantaris was documented by Hamilton et al5. In a large retrospective study by Delgado et al6 plantaris rupture was caused due to tennis leg in only 2 (1.4%) patients out of 141 patients studied. In our opinion, injury to any of the muscles of posterior superficial compartment (gastrocnemius, soleus or plantaris) can lead to similar symptoms that is, ‘tennis leg’. Only the severity varies. With the isolated rupture of plantaris muscle/tendon, the symptoms are less severe as compared to rupture/strain of gastrocnemius and soleus and the patient is mobile comparatively earlier. Our patient had both rupture of plantaris and strain of medial head of gastrocnemius.
Plantaris is actually a vestigial muscle being harvested by surgeons for tendon grafts. Hence its rupture does not result in any significant loss of function. It is a self-healing condition. It becomes an emergency only when associated bleeding and swelling leads to compartment syndrome when urgent fasciotomy is required. The importance of diagnosing this condition lies in the fact that it can mimic other serious conditions like DVT, ruptured baker's cyst and calf neoplasms. Our resident also made mistake and initially diagnosed the condition as DVT. This was because he was not aware of the entity of ruptured plantaris muscle. There is similar lack of knowledge about this entity in emergency care physicians and surgeons and it is mostly overlooked. Plantaris rupture is a strong diagnostic possibility when a mass-like structure of same intensity/echogenisity as muscle is seen in the plane between gastrosoleus along with fluid collection. In such cases, Doppler examination should be added to view normal vein. Moreover, the history is insidious in cases of DVT and not dramatic (snapping pain) as in plantaris rupture. But even in cases of plantaris rupture, snapping pain may be absent (as in two cases reported by Allard et al4). This situation is still more confusing both clinically and radiologically but prudent observation of retracted mass-like stump of ruptured plantaris and visualized normal veins on MRI as well as Doppler can help reach the proper diagnosis. In case of ruptured baker's cyst, the communication of the collection with knee joint between the tendons of medial head of gastrocnemius and semimembranosus should help make the diagnosis. No such communication of fluid collection with knee joint exists in cases of plantaris rupture.
Learning points.
Plantaris rupture can mimic deep vein thrombosis (DVT), ruptured Baker's cyst and calf neoplasm.
Plantaris is actually a vestigial muscle, its rupture does not result in any significant loss of function. It is a self-healing condition.
Plantaris rupture may become an emergency condition only when associated bleeding and swelling leads to compartment syndrome when urgent fasciotomy is required.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned, externally peer reviewed.
References
- 1.Simpson SL, Hertzog MS, Barja RH. The plantaris tendon graft: an ultrasound study. J Hand Surg (Am) 1991;16:708–11 [DOI] [PubMed] [Google Scholar]
- 2.Kwak HS, Han YM, Lee SY, et al. Diagnosis and follow-up US evaluation of ruptures of the medial head of the gastrocnemius (‘tennis leg’). Korean J Radiol 2006;7:193–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Powell RW. Lawn tennis leg. Lancet 1883;2:444173254 [Google Scholar]
- 4.Allard JC, Bancroft J, Porter G. Imaging of plantaris muscle rupture. Clin Imaging 1992;16:54–8 [DOI] [PubMed] [Google Scholar]
- 5.Hamilton W, Klostermeier T, Lim EV, et al. Surgically documented rupture of the plantaris muscle: a case report and literature review. Foot Ankle Int 1997;18:522–3 [DOI] [PubMed] [Google Scholar]
- 6.Delgado GJ, Chung CB, Lektrakul N, et al. Tennis leg: Clinical US study of 141patients and anatomic investigation of four cadavers with MR imaging and US. Radiology 2002;224:112–9 [DOI] [PubMed] [Google Scholar]



