Abstract
Inclusion body myositis is a chronic progressive myopathy which tends not to respond to steroids and immunosuppressive treatments. Dysphagia is more common in this group than other inflammatory myopathies like polymyositis and dermatomyositis. Otolaryngologists are involved in the management of dysphagia in inclusion body myositis. They usually use a combination of cricopharyngeal myotomy, upper oesophageal dilation or botulinum injection to help with the symptoms. Cricopharyngeus myotomy is the preferred treatment in this group and patients tend to be discharged after a short stay in the hospital. However, our experience was completely different from what we expected as a relatively straightforward procedure led to severe morbidity and prolonged hospital admission due to continuous acid reflux and aspiration. We believe that the presence of hiatus hernia led to this problem as the patient's problem resolved completely after her hernia was treated.
Case presentation
A 68-year-old woman presented to the otolaryngology department with long-standing history of dysphagia. She was diagnosed with inclusion body myositis (IBM) confirmed by muscle biopsy and was treated with a combination of prednisolone and methotrexate (figure 1). The patient had an associated hiatus hernia, which was diagnosed as an incidental finding during barium swallow examination for progressive dysphagia (figure 2).
Figure 1.

Contrast swallow study confirming aspiration.
Figure 2.
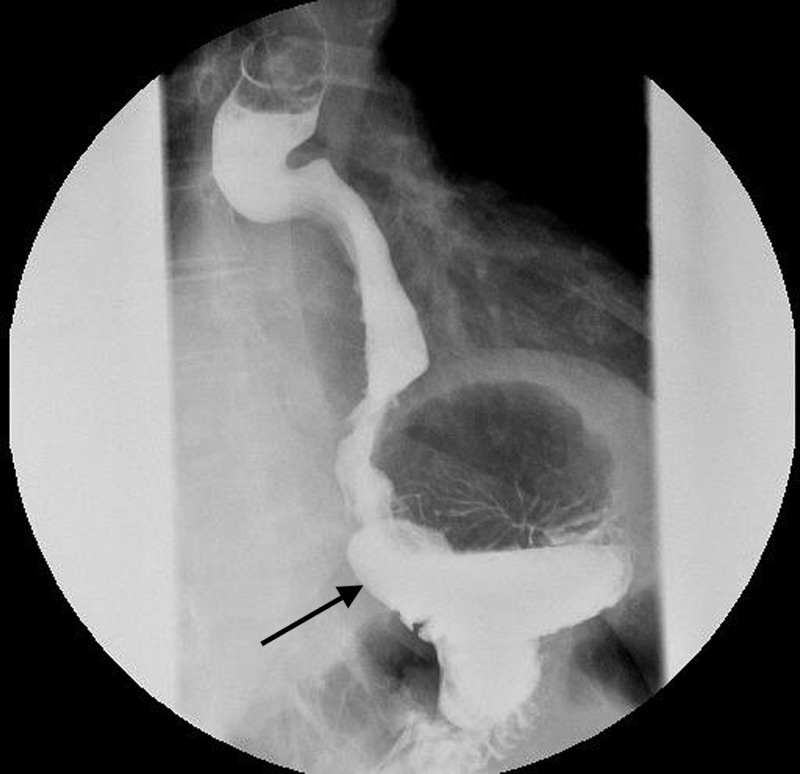
Contrast swallow study demonstrating hiatus hernia (arrow).
Two rigid oesophagoscopy and dilation had failed to resolve the dysphagia. A multidisciplinary meeting of gastroenterologists and upper gastrointestinal surgeons recommended treatment of the cricopharyngeal stricture before a definitive surgical management of hiatus hernia was undertaken as it was generally agreed that cricopharyngeus hypertrophy is responsible for her symptoms.
An external approach cricopharyngeal myotomy was undertaken. Six hours postoperatively the patient had a gastric aspiration leading to respiratory arrest needing intubation and assisted ventilation for several days. An assessment postoperatively suggested that the upper oesophageal stricture was acting as a natural protection preventing the aspiration of gastric contents due to the hiatus hernia.
The cricopharyngeal myotomy caused a loss of this natural protection leading to aspiration pneumonia and its subsequent morbidity.
Outcome and follow-up
The patient had a slow recovery and eventually underwent a laparoscopic repair of hiatus hernia and returned to oral intake 2 months after her cricopharyngeal myotomy. The patient remains well 12 months postoperation.
Discussion
Chou first described IBM in 1967.1 It is a chronic progressive acquired myopathy, which usually affects patients over 50, and men are affected twice as much as women.1 2 The differential diagnoses are mainly polymyositis and dermatomyositis. There is no definitive treatment for IBM but immunosuppressive drugs may provide some benefits.1 3–5
Dysphagia may not be the presenting symptom in IBM patients but is reported by as many as two-thirds of patients at some stage of the disease and can be severe enough to interfere with nutrition.3 Around 40–80% of cases suffer from a degree of swallowing difficulties that may describe it as food sticking in the back of the throat, coughing during meals or taking a long time to finish their meal1 4 5. Among various myopathies, patients with IBM suffer more from dysphagia4 5 and therefore are more prone to aspiration pneumonia and respiratory failure. According to Oh et al5 respiratory failure in association with aspiration pneumonia is the most common cause of death in IBM patients and that highlights the importance of dealing with cricopharyngeus stricture in this group.
Otolaryngologists are involved in treatment of dysphagia in IBM patients. The treatment options include upper oesophageal dilation, botulinum toxin injection or cricopharyngeal myotomy3 which can be done endoscopically or transcervical. It is generally accepted that cricopharyngeal myotomy is the most effective treatment for dysphagia in IBM patients.1 2 4 5 Some authors advocate that all the patients should have antireflux treatment before proceeding with cricopharyngeal myotomy6 but the Williams et al7 study suggests that cricopharyngeal myotomy does not increase the risk of oesophagopharyngeal regurgitation in patients with pharyngeal dysphagia. Henderson et al8 stress that cricopharyngeal myotomy may be performed even in the presence of reflux without fear of subsequent aspiration.
Unfortunately there is no dedicated multidisciplinary team setting for such uncommon conditions. In our case, patient was diagnosed and medically treated by neurologist and subsequently referred to ENT for her cricopharyngeus stricture after it was decided that she should have her cricopharyngeal myotomy before the hiatus hernia being addressed.
Learning points.
Inclusion body myositis (IBM) is a chronic progressive myopathy, it has an insidious course and tends not to respond to steroids and immunosuppressive treatments.1 3–5
Dysphagia due to cricopharyngeus involvement is a more common IBM.2 4
Cricopharyngeal myotomy is the preferred mode of treatment with a better outcome in treatment of dysphagia.2 4
Our report demonstrates that how overlooking an anatomical problem (hiatus hernia) completely changed the outcome and led to unsatisfactory outcome.
Our experience reiterates the fact that each case should be assessed individually and all comorbidities should be accounted for when it comes to treatment choice.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Houser S, Calabrese L, Strome M. Dysphagia in patients with inclusion body myositis. Laryngoscope 1998;108:1001–5 [DOI] [PubMed] [Google Scholar]
- 2.Wintzen A, Bots G, de Bakker H, et al. Dysphagia in inclusion body myositis. J Neurol Neurosurg Psychiatry 1988;51:1542–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Needham M, James I, Corbett A, et al. Sporadic inclusion body myositis: phenotypic variability and influence of HLA-DR3 in a cohort of 57 Australian cases. J Neurol Neurosurg Psychiatry 2008;79:1056–60 [DOI] [PubMed] [Google Scholar]
- 4.Oh T, Brumfield K, Hoskin T, et al. Dysphagia in inclusion body myositis: clinical features, management, and clinical outcome. Am J Phys Med Rehabil 2008;87:883–9 [DOI] [PubMed] [Google Scholar]
- 5.Oh T, Brumfield K, Hoskin T, et al. Dysphagia in inflammatory myopathy: clinical characteristics, treatment strategies, and outcome in 62 patients. Mayo Clin Proc 2007;82:441–7 [DOI] [PubMed] [Google Scholar]
- 6.Kelly JH. Management of upper esophageal sphincter disorders: indications and complications of myotomy. Am J Med 2000;108(Suppl 4a):43S–6S [DOI] [PubMed] [Google Scholar]
- 7.Williams RB, Ali GN, Hunt DR, et al. Cricopharyngeal myotomy does not increase the risk of esophagopharyngeal acid regurgitation. Am J Gastroenterol 1999;94:3448–54 [DOI] [PubMed] [Google Scholar]
- 8.Henderson RD, Hanna WM, Henderson RF, et al. Myotomy for reflux-induced cricopharyngeal dysphagia. Five-year review. J Thorac Cardiovasc Surg 1989;98:428–33 [PubMed] [Google Scholar]


