Abstract
Atlanto-occipital dislocation (AOD) is a grave injury that is rarely survivable. Patients who do survive often have long-term sequelae resulting from the intracranial damage sustained during the traumatic event. The high impact needed to cause AOD is translated to the intracranial vessels, which can lead to vascular injury. Pseudoaneurysm is one of the possible outcomes of damage to the vessel wall. We present a case of basilar artery pseudoaneurysm diagnosed 5 months after a traumatic AOD who was treated with intracranial stent placement and coiling.
Keywords: Aneurysm, Trauma, Stent, Pediatrics, Coil
Background
Atlanto-occipital dislocation (AOD) is frequently a fatal injury that usually occurs after a high impact trauma. In cases of survival, significant intracranial damage and permanent neurologic deficit is a common occurrence. Intracranial vascular structures are exposed to significant shearing forces when the skull and spinal column experience a high-speed acceleration-deceleration. Shearing of the vessel can lead to vessel wall damage with progression to pseudoaneurysm formation or arterial dissection.1 Because of the morbid nature of AOD, there is a paucity of literature addressing the long-term follow-up of functioning survivors. We present the case of a 7-year-old girl who survived an AOD and presented with a delayed mid-basilar pseudoaneurysm 5 months after the initial trauma who was treated with stent-assisted coiling.
Case presentation
A 7-year-old girl presented to our institution after being an unrestrained passenger in a high-speed motor vehicle collision. The Glasgow Coma Scale score reported at the scene was 3T. The initial brain CT showed diffuse cerebral edema, subarachnoid hemorrhage within the basal cisterns and subdural hemorrhage. The patient was also noted to have AOD with significant prevertebral edema (figure 1A,B). The initial MRI of the brain showed T2 signal hyperintensity in the brainstem, specifically the caudal pons and medulla. Ventriculostomy and a cranial ring were placed in the acute period. The patient underwent occipital to C3 fusion for definitive management as well as a ventriculoperitoneal shunt for persistent hydrocephalus. During the patient's prolonged hospital course she was treated for several concomitant abdominal and orthopedic injuries. Five months after the initial trauma the patient had residual weakness of the upper and lower extremities on the right requiring a wheel chair, as well as hyper-reflexia of the lower extremities.
Figure 1.
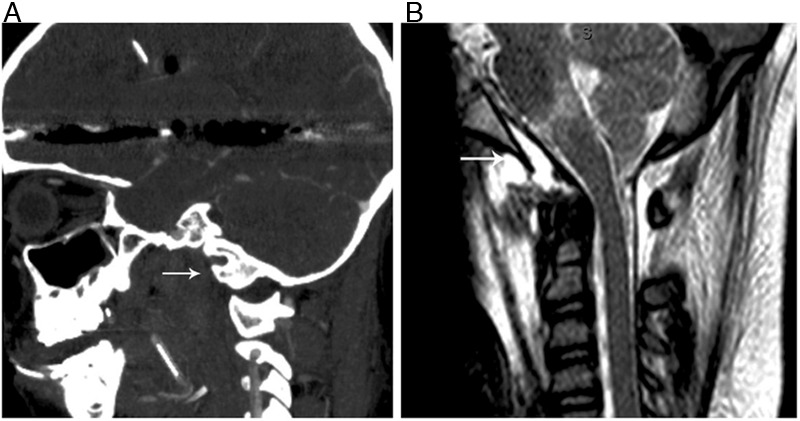
(A) Sagittal CT of the head and cervical spine in bone windows at the time of injury demonstrating atlanto-occipital dislocation (arrow). (B) Sagittal T2-weighted MRI showing prevertebral edema (arrow).
Investigations
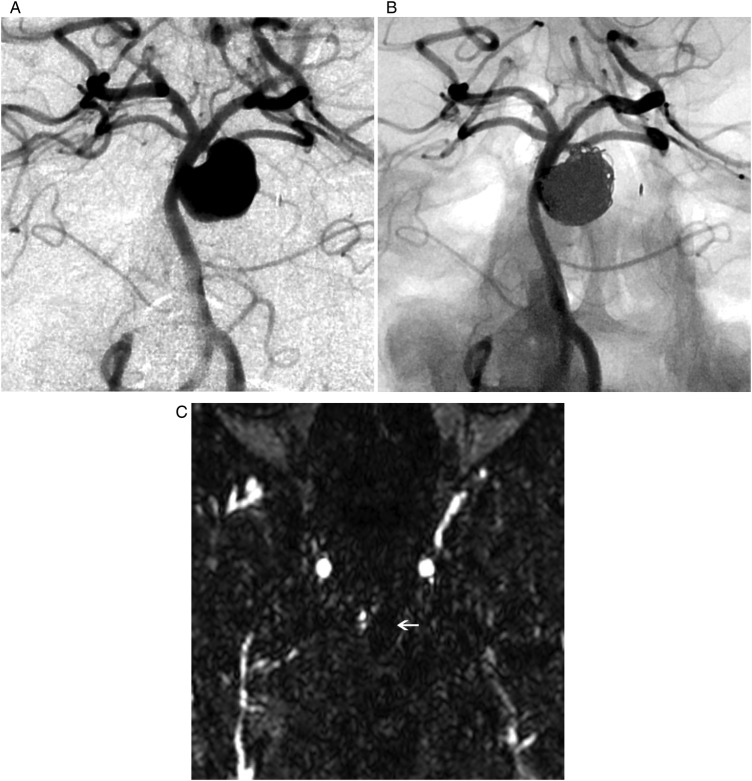
The initial follow-up MRI of the brain at 3 months showed a dark T2 signal lesion distorting the pons (figure 2A). A follow-up CT angiogram 5 months after the trauma showed development of a large saccular pseudoaneurysm arising from the basilar artery (figure 2B). Digital subtraction angiography was then performed and revealed a mid-distal basilar artery multilobulated pseudoaneurysm measuring 10 mm×12 mm with a 5.5 mm neck (figure 3A).
Figure 2.
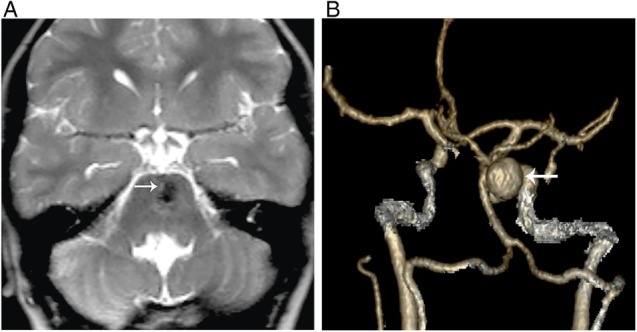
(A) Axial T2-weighted MRI 5 months after the initial trauma showing a dark signal lesion distorting the pons (arrow). (B) Three-dimensional reconstruction CT angiogram 5 months after the initial trauma showing development of a large saccular aneurysm arising from the mid-distal basilar artery (arrow).
Figure 3.
(A) Anterior posterior right vertebral artery angiogram confirms the findings of the CT angiogram. (B) Post-intervention right vertebral angiogram showing normal filling of the parent vessel with only minimal filling of the aneurysm neck. (C) Axial contrast enhanced magnetic resonance angiogram 3 months after coil placement showing no filling of the pseudoaneurysm with metal artifact from the coils.
Treatment
The patient was started on a dual antiplatelet regimen consisting of 81 mg aspirin and 50 mg clopidogrel (Plavix; Bristol-Meyers Squibb, New York, USA) based on the patient's weight 7 days prior to the procedure. Under general anesthesia, the right common femoral artery was punctured retrograde and a 6 F sheath placed. A 6 F MPC guide catheter (Cordis, Miami Lakes, Florida, USA) was advanced into the right vertebral artery. A right vertebral arteriogram was obtained in the anteroposterior and lateral projections. Intravascular ultrasound demonstrated evidence of a dissection in the region of the pseudoaneurysm. The patient was treated by jailing the microcatheter within the pseudoaneurysm, with ‘off-label’ placement of a 3 mm×20 mm Neuroform EZ stent (Stryker Neurovascular; Freemont, California, USA) across the neck of the pseudoaneurysm. This off-label use of a Humanitarian Device Exemption (HDE) device was communicated to the Institutional Review Board and to the manufacturer as per protocol in the USA. Nineteen coils were placed within the pseudoaneurysm and a follow-up angiogram showed no occlusion of the parent vessel and only minimal filling of the pseudoaneurysm neck (figure 3B).
Outcome and follow-up
At 3-month follow-up, magnetic resonance angiography with contrast showed no evidence of pseudoaneurysm recurrence.
Discussion
AOD has long been considered a grave injury resulting in immediate death or significant neurologic damage (quadriparesis, vegetative state). Recent reports have suggested that AOD is a survivable injury in cases without a high cervical cord injury.2 In such cases, complete or incomplete neurologic deficits occur most of the time.3 Although significant intracranial damage with AOD is common, there are no reports of basilar artery pseudoaneurysm after traumatic AOD.
Basilar artery pseudoaneurysm as a result of trauma is a rare but reported event. It is often the result of penetrating trauma4 or adjacent fracture.5 There is one case report of a traumatic basilar pseudoaneurysm without an associated skull fracture.6 In that case, there was immediate development of a pseudoaneurysm (post-trauma day 1), unlike our patient who was found to have a pseudoaneurysm 5 months after the trauma. The authors postulated that acceleration-deceleration caused shearing of the basilar artery or compression of it against the clivus, which damaged the arterial wall.6 We believe that this is a likely mechanism for the formation of pseudoaneurysm in our case as well. The traumatic forces that caused dissociation of the occiput from the spine probably placed significant shear stress on the basilar artery, thus tearing the layers of the vessel wall and forming a pseudoaneurysm.1 This hypothesis is further strengthened by the evidence of high signal within the brainstem of our patient, which could have been due to small perforator vessel shearing.6
Stent-assisted coiling was determined to be the best treatment option given the wide aneurysm neck (>4 mm). This technique has become a promising option for dissecting or wide-necked ‘true’ or ‘pseudo’ aneurysms.7–11 As an additional benefit in cases of dissection, the stent bolsters the true lumen and traps the associated hematoma.10 Although stent coiling is not without risk, in the past definitive management of basilar pseudoaneurysm has progressed to vessel sacrifice.5 With stent coiling this morbid option can be avoided, allowing for better outcomes and preserved neurologic function in treated patients. The coil mass theoretically could contribute to persistent compression of the descending corticospinal tract resulting in permanent spasticity. In the future, flow diverting stents may have a role in the treatment of this condition, thus avoiding mass effect from placement of coils in the pseudoaneurysm.
Learning points.
Traumatic atlanto-occipital dislocation (AOD) is a possible mechanism for development of an intracranial vessel pseudoaneurysm.
Monitoring of the intracranial vasculature for development of pseudoaneurysm is reasonable in the long-term follow-up of patients with AOD.
Failure to adequately follow patients after AOD could lead to a devastating outcome.
Stent-assisted coiling is a feasible treatment option for a traumatic mid-basilar pseudoaneurysm or dissection.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Parkinson D, West M. Traumatic intracranial aneurysms. J Neurosurg 1980;52:11–20 [DOI] [PubMed] [Google Scholar]
- 2.Chaput CD, Torres E, Davis M, et al. Survival of atlanto-occipital dissociation correlates with atlanto-occipital distraction, injury severity score, and neurologic status. J Trauma 2011;71:393–5 [DOI] [PubMed] [Google Scholar]
- 3.Labbe JL, Leclair O, Duparc B. Traumatic atlanto-occipital dislocation with survival in children. J Pediatr Orthop B 2001;10:319–27 [PubMed] [Google Scholar]
- 4.Bank WO, Nelson PB, Drayer BP, et al. Traumatic aneurysm of the basilar artery. AJR Am J Roentgenol 1978;130:975–7 [DOI] [PubMed] [Google Scholar]
- 5.Quintana F, Diez C, Gutierrez A, et al. Traumatic aneurysm of the basilar artery. AJNR Am J Neuroradiol 1996;17:283–5 [PMC free article] [PubMed] [Google Scholar]
- 6.Connor SE, Martin AJ, Deasy NP, et al. Traumatic basilar pseudoaneurysm with a basilar-cavernous arteriovenous fistula. Neuroradiology 2001;43:249–53 [DOI] [PubMed] [Google Scholar]
- 7.Phatouros CC, Sasaki TY, Higashida RT, et al. Stent-supported coil embolization: the treatment of fusiform and wide-neck aneurysms and pseudoaneurysms. Neurosurgery 2000;47:107–13; discussion 113–5 [DOI] [PubMed] [Google Scholar]
- 8.Ahn JY, Han IB, Kim TG, et al. Endovascular treatment of intracranial vertebral artery dissections with stent placement or stent-assisted coiling. AJNR Am J Neuroradiol 2006;27:1514–20 [PMC free article] [PubMed] [Google Scholar]
- 9.Fiorella D, Albuquerque FC, Woo H, et al. Neuroform stent assisted aneurysm treatment: evolving treatment strategies, complications and results of long term follow-up. J Neurointerv Surg 2010;2:16–22 [DOI] [PubMed] [Google Scholar]
- 10.Ansari SA, Thompson BG, Gemmete JJ, et al. Endovascular treatment of distal cervical and intracranial dissections with the neuroform stent. Neurosurgery 2008;62:636–46 [DOI] [PubMed] [Google Scholar]
- 11.McElroy KM, Malone RJ, Freitag WB, et al. Traumatic pseudoaneurysm of the basilar artery. Am J Phys Med Rehabil 2008;87:690–1 [DOI] [PubMed] [Google Scholar]