Abstract
A woman having already undergone maxillectomy came to the department complaining of difficulty in eating and speech. During the construction of an obturator, the bulb area should be hollowed to reduce weight so that the teeth and supporting tissues are not stressed unnecessarily. The conventional open design drains fluid from the adjacent mucosa, possibly increasing the weight of the prosthesis, and is difficult to clean. The closed bulb design does not drain secretions and may cause obstruction and susceptibility to infection in the paranasal and pharyngeal regions, though it is easier to maintain. An alternative to the two designs, combining their advantages, is presented in this report. As the open hollow part of the obturator was shallow, it was easy to clean. Making the inferior part of the bulb hollow and closed led to a reduction in the overall weight of the prosthesis while increasing its resonance.
Background
A maxillectomy defect creates a communication from the oral cavity to the nasal cavity that may extend to the orbit which creates deglutition, cosmetic and speech problems with a significant soft and osseous tissue deficiency. Reconstruction of the maxillectomy defect remains a considerable challenge because of the structural design of the defect. Bone restoration should be planned in medium to large defects with good prognosis whenever midface contour, orbital support and dental rehabilitation are a priority. Although maxillectomy defects may also be managed using a maxillofacial obturator or a soft tissue free flap, bone flaps are often required to restore midfacial defect and to provide adequate bone for mastication, aesthetic, speech and osseointegrated dental implants, which are usually required for retention of maxillofacial prostheses.1
The use of a palatal plate-type obturator in patients with palatal defects is a common procedure. The main challenge resides in the proper management of problems such as regurgitation and nasal voice, particularly if the patient uses a palatal plate kind of denture-obturator, which, when in function, often causes the denture to move, subsequently leading to food entrapment between the denture and the defect. A full bulb is likely to increase the weight of the prosthesis, compromising the success of the rehabilitation; a hollow bulb prosthesis is often a good choice, as it is lighter in weight and is more hygienic. Furthermore, a closed hollow bulb obturator also increases speech intelligibility and prevents fluid and food collection, reducing the airspace and maximising the extension.2
The classic technique for making an open-type hollow obturator was to grind the interior of the bulb after processing while monitoring the thickness of the wall.3 The open-type hollow obturator has the advantages of collecting secretions, with associated weight and odour problems. The closed hollow obturator fails to drain secretions, thereby increasing the tendency to infections. The technique described here attempted to remove the inherent disadvantages of the open and closed bulb designs while incorporating their advantages.
Case presentation
A 35-year-old woman having already undergone maxillectomy of the right side due to a pleomorphic adenoma came to the department complaining of difficulty in eating and speech. Except for tooth numbers 17 and 36, all teeth were present in the mandibular arch and remaining maxillary arch (figure 1). The mouth opening was adequate, with an obliterated vestibule on the resected side. The mucosa appeared normal and the records showed that a split thickness graft had been given to line the defect. As healing had occurred and more than 4 months had elapsed since the resection, it was decided to give an obturator.
Figure 1.

Maxillary defect.
Treatment
Preliminary impressions were made with irreversible hydrocolloid after blocking the defect undercut with gauze and custom trays were fabricated. Low and high fusing impression compounds were mixed in 1:1 ratio and added incrementally to record the extension of the defect area. This ratio was selected to provide a combination of rigidity and mouldability for the accurate recording of anatomical landmarks. The patient was made to perform a variety of movements to shape the impression material according to the associated muscles. At the completion of moulding, the roof of the bulb was carefully scraped in its centre to produce a small saucer of 10–12 mm depth, with borders of the saucer being at least 2–3 mm wide for collection of secretions, taking care that the borders were not damaged. This would form the future open part of the hollow bulb in its superior half. This was followed by a routine final impression with zinc oxide eugenol, and the impression was poured out (figure 2).
Figure 2.
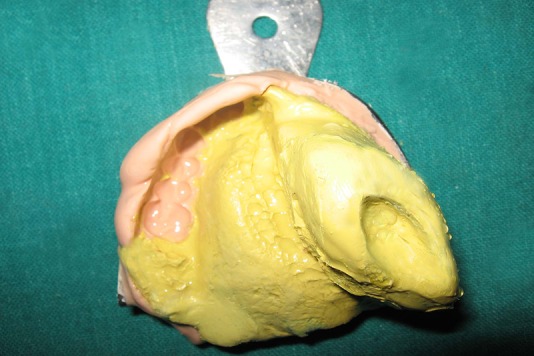
Dual impression of the defect showing a superior open hollow bulb.
The record base and occlusal rim were constructed taking due care not to damage the cast; jaw relation records, teeth setting and try in appointment were performed conventionally. To create the inferior closed hollow bulb, modelling clay was contoured in the defect area using the patient's palatal form as a guide. The clay was covered with a tin foil as a separating medium, followed by a wax lid construction and separation. The wax lid and trial dentures were processed separately. The open palatal end of the denture was sealed with the processed lid using autopolymerising resin. Thus, a bulb was fabricated with two parts, the superior one being an open hollow and the inferior one, a closed hollow (figure 3).
Figure 3.
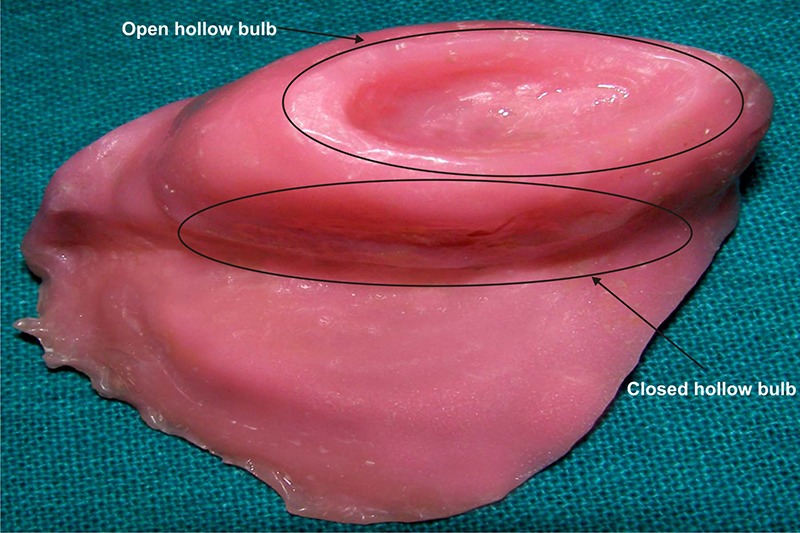
Finished obturator with a superior open hollow bulb and inferior closed hollow bulb.
Outcome and follow-up
Insertion, postinsertion and follow-up appointments were carried out at regular intervals. The patient was satisfied with the prosthesis and was practicing good denture and oral hygiene measures.
Discussion
The study of Oral K and Aramany MA supported the open hollow bulb obturator as it was less obtrusive and permitted better airflow, resonance and speech.4 The superior small saucer end of the fabricated obturator helped in drainage of the fluid, eliminating the need for a full difficult to clean, open-type hollow obturator. The retention and stability of the obturator can be enhanced by making a closed hollow bulb obturator as it reduces the weight of the prosthesis.5 6 The inferior closed hollow portion of the fabricated bulb aided in weight reduction of the prosthesis, thus combining the best of the open and closed design hollow obturator philosophies.
Learning points.
The objective of this phase is to provide the patient with a comfortable and functional prosthesis.
The obturator fabricated for this case is a hybrid obturator which is more hygienic and lightweight.
As the open hollow part of the obturator was shallow, it was easy to clean. Making the inferior part of the bulb hollow and closed led to a reduction in the overall weight of the prosthesis while increasing its resonance.
The appliance improved the quality of life by improving speech and mastication.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Andrades P, Militsakh O, Hanasono MM, et al. Current strategies in reconstruction of maxillectomy defects. Arch Otolaryngol Head Neck Surg 2011;137:806–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Elangovan S, Loibi E. Two-piece hollow bulb obturator. Indian J Dent Res 2011;22:486–8 [DOI] [PubMed] [Google Scholar]
- 3.Matalon V, LaFuente H. A simplified method for making a hollow obturator. J Prosthet Dent 1976;36:580–2 [DOI] [PubMed] [Google Scholar]
- 4.Aramany MA, Drane JB. Effect of nasal extension sections on the voice quality of acquired cleft palate patients. J Prosthet Dent 1972;27:194–2 [DOI] [PubMed] [Google Scholar]
- 5.Bhasin AS, Singh V, Mantri SS. Rehabilitation of patient with acquired maxillary defect, using a closed hollow bulb obturator. Indian J Palliat Care 2011;17:70–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Raja HZ, Saleem MN. Gaining retention, support and stability of a maxillary obturator. J Coll Physicians Surg Pak 2011;21:311–14 [PubMed] [Google Scholar]


