Abstract
Purpose
The purpose of this study was to assess cone-beam computed (CBCT) sialography imaging in the detection of different changes associated with lesions of salivary glands.
Materials and Methods
This study consisted of 8 cases with signs and symptoms from salivary gland lesions. Conventional sialography using digital panoramic and lateral oblique radiographs and CBCT sialography were performed for each subject. The radiographs were evaluated by 3 radiologists independently of each other. The results were compared between conventional sialography and CBCT sialography in the evaluation of various lesions associated with the salivary glands.
Results
There was an agreement between the radiologists in interpreting the lesions that affected salivary glands with both techniques. The detection of the presence of stones or filling defects, stenosis, ductal evagination, dilatation, and space occupying lesions was 83% for conventional sialography compared with CBCT sialography. CBCT sialography was superior to conventional sialography in revealing stones, stenosis, and strictures, especially in the second and third order branches.
Conclusion
It would be advisable to perform CBCT sialography in cases of obstructive salivary gland diseases for better demonstration of the ductal system of the gland.
Keywords: Cone-Beam Computed Tomography, Salivary Glands, Sialography
Introduction
Major salivary glands can present a variety of lesions, which can appear clinically as a lateral facial swelling or diffuse glandular enlargement accompanied by symptoms of obstruction or inflammation. Radiographic examination is essential in diagnosing the lesions, and useful for planning further management, whether surgery or alternatives.1,2 Plain radiography, sialography, computed tomography (CT), cone-beam CT (CBCT), ultrasonography (US), magnetic resonance imaging (MRI), and nuclear scintigraphy/positron emission tomography (PET) all play roles in the diagnosis of salivary gland lesions.3
Evaluation of the salivary glands by plain radiography is of limited clinical value. It can show sialoliths or involvement of the adjacent mandible by a tumor. Sialography requires injecting contrast media into the Stensen's or Wharton's duct of the major salivary glands to identify the outline of the ductal anatomy and any presence of sialoliths. It creates excellent contrast resolution and allows small stones or strictures to be detected. The invasiveness of the technique, use of contrast media, and possible failure of the technique are limitations of sialography.2 CT is the technique of choice to look for bony erosion caused by malignant lesions, small calculi within the salivary gland or duct, and inflammatory diseases such as abscess, calculi, major salivary duct dilatation, and acute inflammation. Also, CT is useful for patients with contraindication for MRI. Enhanced CT can enable the staging of malignant disease that involves the salivary glands. Coronal and sagittal reconstructions can be helpful in the evaluation of perineural spread. Moreover, enhanced CT is useful for assessing lymphadenopathy of the pharynx and neck. CT is more readily available and of lower cost than MRI; however, its main disadvantage is the high dose of radiation involved.4-8
Recently, CBCT has been increasingly used for head and neck and dento-maxillofacial diagnosis. It provides relatively high isotropic spatial resolution of osseous structures. Due to the cone-shaped x-ray beam and two-dimensional detectors, the CBCT scanner can collect volume data by means of a single rotation taking 9-40 seconds. The CBCT scanners offer hard tissue visualization of the maxillofacial region and evaluation of skeletal morphology.9 CBCT sialography has rarely been reported. Drage and Brown10 were pioneers in reporting cases of CBCT sialography. They concluded that CBCT sialography was superior to conventional sialography and explained that 3D reconstruction could be performed and then viewed from any direction and in any slice thickness, and from which cross-sectional slices might be obtained in any direction. This might prove useful for demonstrating areas of complex anatomy.
In this study, further investigation of the potentials of CBCT sialography was conducted. The role of CBCT sialography in diagnosing salivary gland lesions was also assessed.
Materials and Methods
The study protocol was approved by the Ethics Committee of the Faculty of Dentistry, Minia University. Eight patients were selected from among the outpatients of dental clinics. The selection criteria were based on the presence of the symptoms of pain and swelling of the parotid or submandibular salivary gland. Detailed history taking and clinical examination of the patients were performed. Inclusion criteria in this study were having signs and symptoms related to a salivary gland disease, while exclusion criteria were the presence of acute stages of inflammation affecting the salivary glands. In total, this study consisted of 8 patients (6 males and 2 females) with ages ranging from 18 to 60 years.
Sialography was conducted by probing and cannulation of Wharton's ducts for submandibular salivary gland and Stensen's duct for the parotid gland, followed by injection of approximately 1.5-2 mL Urografin contrast media until the patient felt fullness. For conventional sialography evaluation in cases involving the submandibular gland, the patients underwent digital panoramic, lateral oblique, postroanterior, and occlusal imaging. In addition, CBCT examination was performed using Scanora® 3D with Auto-Switch™ (Soredex, Helsinki, Finland) with 85 kVp, 15 mA, and a field of view (FOV) of 4 cm for the submandibular gland and 5 cm for the parotid gland. OnDemand 3DTM software (Cybermed Inc., Seoul, Korea) was used to manipulate the CBCT images in multiplanar slices as well as three dimensional images to examine the lesions.
Three radiologists evaluated the images separately and scores were given for the interpretation of the images according to the following scoring systems. A scoring system was performed to evaluate the presence of ductal evagination (unique diverticulum filled with contrast media and narrow neck of the duct). The scores given were: 0=definitely not present, 1=probably not present, 2=not sure, 3=probably present, 4=definitely present, and 5=many evaginations within the duct. This rating system was also used to record the presence of dilatation of the primary and secondary ducts. The presence of salivary stones or filling defects was rated as follows: 1=one sialolith, 2=two sialoliths, 3=three sialoliths, 4=four sialoliths, and 5=more than four sialoliths. The presence of stenosis was also rated as follows: 0=not present, 1=the presence of stenosis, 2=the presence of stenosis in more than one area, and 3=intraglandular second-order branches. The presence of a space-occupying lesion and the presence of bizarrely shaped contrast media was rated as follows: 0=definitely not present, 1=probably not present, 2=not sure, 3=probably present, 4=definitely present, and 5=bizarre area. The above mentioned scoring system for evaluation was used by each radiologist to assess the interpretation criteria separately and then results were discussed with the others.
Fine needle aspiration biopsy was done when needed to examine the type of pathology present, while surgical intervention was conducted in cases of obstructive lesions (stones and stenosis). Analysis of the resulting data was performed to evaluate the concordance among interpretations of the three radiologists.
Results
There was agreement among the three radiologists in interpreting the lesions of the salivary glands with both techniques. The detection of salivary gland lesions was 100% for both conventional sialography and CBCT sialography. Among the 8 patients in this study, two patients suffered from autoimmune disease (Sjögren's syndrome) affecting the parotid gland and one case had a lymphoepithelial lesion in the parotid gland (according to biopsy examination), while the other five cases suffered from obstructive diseases due to stones and calculi in the parotid gland (2 cases) and in the submandibular gland (3 cases).
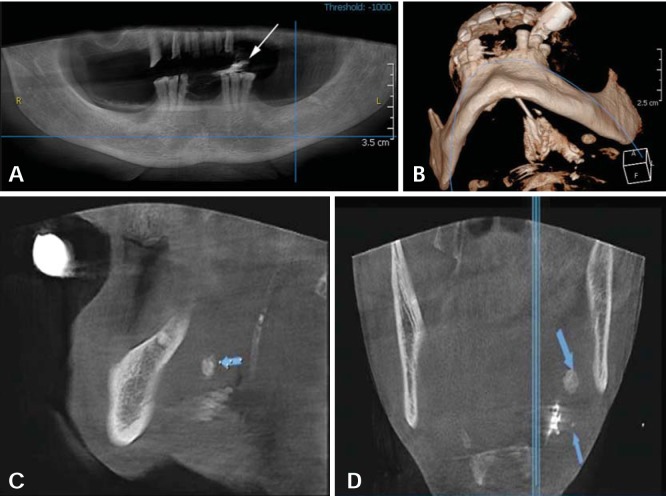
Two parotid gland cases showed the signs of filling defects, strictures in the main duct, and dilatation of the ducts distal to the filling defect. Three cases of the submandibular glands showed obstructive diseases with stenosis and evagination. In addition, stones of various sizes, locations, and radiodensities were observed. The detection rate of the presence of stones or filling defects, stenosis, ductal evagination, dilatation, and space occupying lesions was 83% for conventional sialography compared with CBCT sialography (Fig. 1). CBCT sialography was superior to conventional sialography in revealing stones, especially in the second and third order branches.
Fig. 1.
Panoramic (A), 3D reconstruction (B), sagittal (C), and coronal (D) images of CBCT with large and small stones in the submandibular gland (arrows).
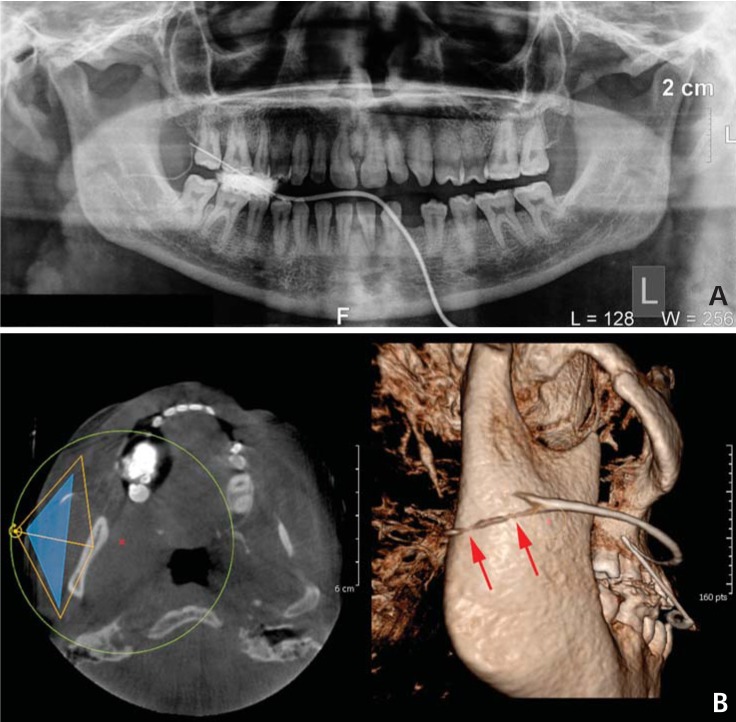
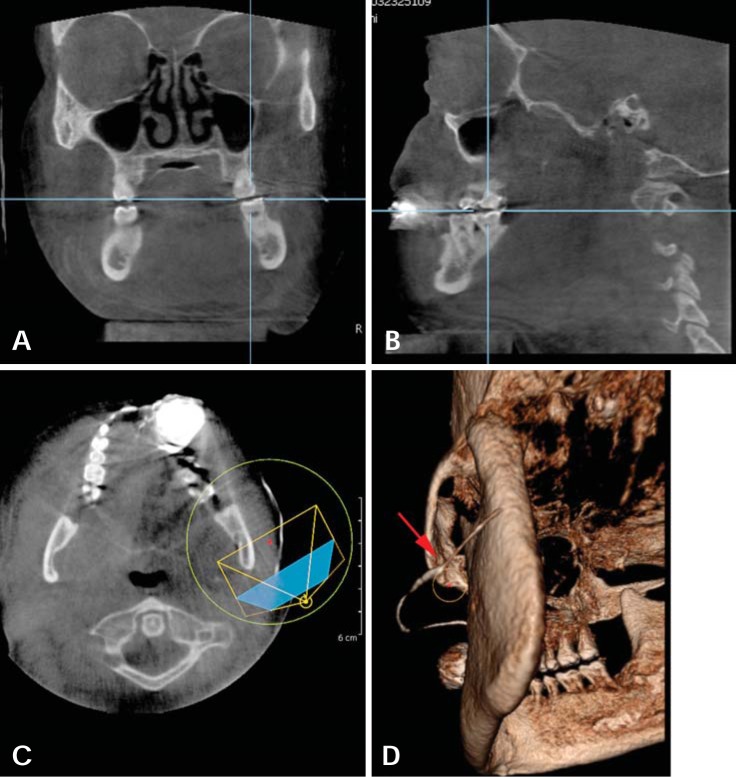
The two cases of autoimmune disease (Sjögren's syndrome) showed stenosis and strictures along the main ducts and the first, second, and third order branches. CBCT sialography was superior to conventional sialography in revealing the areas with strictures and a punctuated appearance of the glands (Figs. 2-4).
Fig. 2.
A. Panoramic sialogram shows stenosis of the right Stensen's duct. B. CBCT sialography axial cut of the same patient and the relevant 3D reconstruction show stenosis with areas of strictures through the glandular ductules (arrows).
Fig. 4.
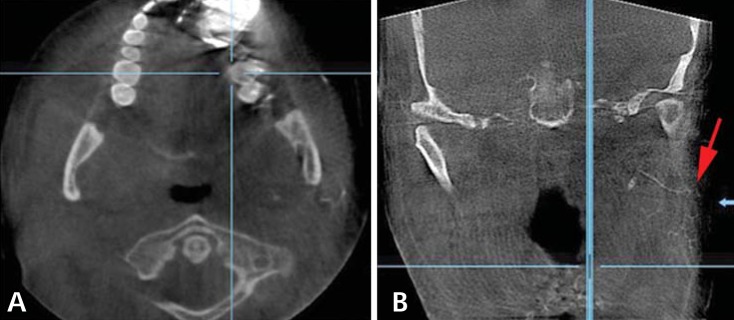
Axial cut (A) and coronal cut (B) of CBCT sialography show stenosis of the ductules with punctuated appearance of the gland (arrow).
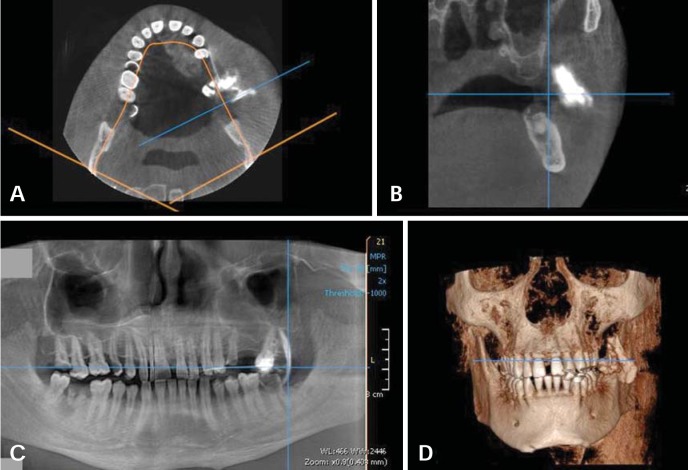
The case of a lymphoepithelial lesion of the parotid gland showed no specific radiologic features. It prevented the contrast medium from distribution inside the gland ductal system and showed unspecific accumulation of it (Fig. 5).
Fig. 5.
Axial (A), coronal (B), panoramic (C), and 3D reconstruction (D) images of CBCT sialography in a case of lymphoepithelial lesion show unspecific accumulation of contrast medium.
Discussion
Despite several limitations of sialography, it remains widely used for the diagnosis of salivary gland diseases, which affect the ductal system; in addition it provides the ability to assess the suitability for interventional procedures and radiolucent stones. Although CT and ultrasonography have been used, they have shown to be of limited value in visualizing the ductal system. However, a reliable technique that generates reproducible results similar to those of sialography has yet to emerge.1,11-14
CBCT has recently become widespread in maxillofacial radiology due to its high resolution and low radiation dose. It offers improvement in demonstration of the ductal system over conventional sialography.15 In this study, stenosis, ductal evagination, dilatation, stones or filling defects, and space occupying lesions were used as the parameters for the diagnosis in CBCT sialography since these findings were the signs of salivary gland diseases. Some authors have suggested that major salivary gland diseases could be divided into neoplastic lesions, obstructive or inflammatory lesions, and systemic diseases.4,16 Salivary gland neoplasms usually manifest clinically as enlarging masses, sometimes with dull gnawing pain. In cases of malignant neoplasms, infiltration of the overlying skin, regional adenopathy, or facial nerve palsy may develop. Primary malignancies of salivary glands, relatively infrequent, can spread to regional lymph nodes. As a rule in salivary gland neoplasms, the smaller the salivary gland, the higher the rate of malignancy. In contrast to salivary gland neoplasms, the obstructive and inflammatory lesions clinically manifest with cardinal signs of inflammation such as pain and swelling of the gland. Sialolithiasis is the second most common disease of the salivary glands after mumps. Obstruction of the salivary gland usually results from the development of salivary calculi, ductal strictures, or both. Imaging plays a crucial role in the diagnosis of the cause, extent, and effects of the obstruction.2,3,17-19
In this study, five of eight cases had sialolithiasis: two cases in the parotid and three in the submandibular gland. This was in agreement with previous studies,4,20 which have stated that the submandibular gland more frequently forms sialoliths due to more alkaline, thick, and viscous saliva. It should also be noted that the stasis in the Wharton's duct is a result of its uphill course with a wider lumen and a tighter orifice.4,20 The location of the calculi can affect the symptoms. The symptoms tend to be minor when the calculi occur within the gland in comparison with a location within the intraglandular ductal tributaries or within the main ducts.3 The calculi can be single or multiple. As a complication of sialolithiasis, stricture can occur. Evagination can be found in cases of the presence of stones due to wall damage and weakness. It has also been hypothesized that evagination might be a form of duct wall malformation, which leads to a localized weakness of the duct wall that becomes evident despite increased pressure in the ductal system, caused by impairment of excretion of the saliva.20 In this study, one case with severe stricture showed evagination. Chronic sialadenitis may result from the poor outflow of saliva. Moreover, secondary infection of the gland can originate from incomplete obstruction by a sialolith. When complete obstruction continues, glandular atrophy eventually occurs, which was demonstrated in this study. On the other hand, Sjögren's syndrome can also show stenosis and strictures of ductal systems due to autoimmune inflammatory conditions, which produced chronic sialadenitis.1,21
One case in this study was diagnosed histopathologically as a benign lymphoepithelial lesion, or Godwin's tumor, which represented a manifestation of autoimmune disease in the salivary glands. It showed no specific findings in conventional sialography and CBCT sialography. CT or MRI should be used for the evaluation of the extent and nature of any space-occupying lesions in the salivary gland.22,23
The inter-observer correlation in conventional sialography to detect signs such as evagination, dilatation, stones, and presence of a space-occupying lesion was good. Sialography represents an appropriate first line investigation in cases with strong clinical suspicion of inflammatory duct disease or salivary calculi conditions. Conventional sialography uses panoramic, occlusal, and postroanterior radiographs, which provide appropriate views for examining the major salivary glands.9 Moreover, the high correlation among the three observers interpreting the salivary gland lesions, in terms of presence of stenosis, dilatation, evagination, and stones by using CBCT sialography, suggests the superiority of using CBCT. The CBCT scanner uses a cone-shaped X-ray beam with two-dimensional detectors and collects data by means of a single rotation around the patient taking 9-40 seconds. The reconstruction is then processed and the resultant image matrix is isotropic. The software of the system provides various processed images such as multiplanar reconstruction, volume rendering, cross sectional, and partial panoramic images. Due to the isotropic voxels, the images of the anatomic structures can be reconstructed clearly and accurately in any plane.9 Li et al studied the diagnosis of simple bone cysts by CBCT sialography.15 They noted that the sialographic technique could be improved by the combination of sialography and CBCT, especially by 3D formatting. CBCT sialography was considered to be a novel and promising approach for investigating simple bone cysts as it provides detailed information about the content of the cavity.15 Regarding the effective doses from CBCT examinations centered on the parotid and submandibular glands, Jadu et al concluded that they were similar to those calculated for plain radiography for sialography when 15 cm FOV was chosen in combination with exposure conditions of 80 kVp and 10 mA.24
In conclusion, in cases that have obstructive salivary gland diseases, it would be advisable to perform CBCT sialography as the modality of choice in demonstrating the ductal system of the gland and as an alternative to conventional sialography.
Fig. 3.
Coronal (A), sagittal (B), axial (C), and 3D reconstruction (D) images show multiple stenoses in Stensen's duct (arrow).
References
- 1.Jäger L, Menauer F, Holzknecht N, Scholz V, Grevers G, Reiser M. Sialolithiasis: MR sialography of the submandibular duct - an alternative to conventional sialography and US? Radiology. 2000;216:665–671. doi: 10.1148/radiology.216.3.r00se12665. [DOI] [PubMed] [Google Scholar]
- 2.Burke CJ, Thomas RH, Howlett D. Imaging the major salivary glands. Br J Oral Maxillofac Surg. 2011;49:261–269. doi: 10.1016/j.bjoms.2010.03.002. [DOI] [PubMed] [Google Scholar]
- 3.Levy DM, ReMine WH, Devine KD. Salivary gland calculi. Pain, swelling associated with eating. JAMA. 1962;181:1115–1119. doi: 10.1001/jama.1962.03050390017005. [DOI] [PubMed] [Google Scholar]
- 4.Yousem DM, Kraut MA, Chalian AA. Major salivary gland imaging. Radiology. 2000;216:19–29. doi: 10.1148/radiology.216.1.r00jl4519. [DOI] [PubMed] [Google Scholar]
- 5.Rinast E, Gmelin E, Hollands-Thorn B. Digital subtraction sialography, conventional sialography, high-resolution ultrasonography and computed tomography in the diagnosis of salivary gland diseases. Eur J Radiol. 1989;9:224–230. [PubMed] [Google Scholar]
- 6.Eracleous E, Kallis S, Tziakouri C, Blease S, Gourtsoyiannis N. Sonography, CT, CT sialography, MRI and MRI sialography in investigation of the facial nerve and the differentiation between deep and superficial parotid lesions. Neuroradiology. 1997;39:506–511. doi: 10.1007/s002340050455. [DOI] [PubMed] [Google Scholar]
- 7.Szolar DH, Groell R, Braun H, Preidler K, Stiskal M, Kern R, et al. Ultrafast computed tomography and three-dimensional image processing of CT sialography in patients with parotid masses poorly defined by magnetic resonance imaging. Acta Otolaryngol. 1996;116:112–118. doi: 10.3109/00016489609137723. [DOI] [PubMed] [Google Scholar]
- 8.Szolar DH, Groell R, Preidler K, Braun H, Stiskal MA, Stammberger H, et al. Three-dimensional processing of ultrafast CT sialography for parotid masses. AJNR Am J Neuroradiol. 1995;16:1889–1893. [PMC free article] [PubMed] [Google Scholar]
- 9.Yajima A, Otonari-Yamamoto M, Sano T, Hayakawa Y, Otonari T, Tanabe K, et al. Cone-beam CT (CB Throne) applied to dentomaxillofacial region. Bull Tokyo Dent Coll. 2006;47:133–141. doi: 10.2209/tdcpublication.47.133. [DOI] [PubMed] [Google Scholar]
- 10.Drage NA, Brown JE. Cone beam computed sialography of sialoliths. Dentomaxillofac Radiol. 2009;38:301–305. doi: 10.1259/dmfr/90784441. [DOI] [PubMed] [Google Scholar]
- 11.Gritzmann N. Sonography of the salivary glands. AJR Am J Roentgenol. 1989;153:161–166. doi: 10.2214/ajr.153.1.161. [DOI] [PubMed] [Google Scholar]
- 12.Avrahami E, Englender M, Chen E, Shabtay D, Katz R, Harell M. CT of submandibular gland sialolithiasis. Neuroradiology. 1996;38:287–290. doi: 10.1007/BF00596550. [DOI] [PubMed] [Google Scholar]
- 13.Ngu RK, Brown JE, Whaites EJ, Drage NA, Ng SY, Makdissi J. Salivary duct strictures: nature and incidence in benign salivary obstruction. Dentomaxillofac Radiol. 2007;36:63–67. doi: 10.1259/dmfr/24118767. [DOI] [PubMed] [Google Scholar]
- 14.Salerno S, Cannizzaro F, Comparetto A, Speciale R, Lo Casto A. Sialographic findings in Wharton duct evagination. Dentomaxillofac Radiol. 2009;38:550–553. doi: 10.1259/dmfr/63463343. [DOI] [PubMed] [Google Scholar]
- 15.Li B, Long X, Cheng Y, Wang S. Cone beam CT sialography of Stafne bone cavity. Dentomaxillofac Radiol. 2011;40:519–523. doi: 10.1259/dmfr/84472023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Licitra L, Grandi C, Prott FJ, Schornagel JH, Bruzzi P, Molinari R. Major and minor salivary glands tumours. Crit Rev Oncol Hematol. 2003;45:215–225. doi: 10.1016/s1040-8428(02)00005-7. [DOI] [PubMed] [Google Scholar]
- 17.Brown JE. Interventional sialography and minimally invasive techniques in benign salivary gland obstruction. Semin Ultrasound CT MR. 2006;27:465–475. doi: 10.1053/j.sult.2006.09.003. [DOI] [PubMed] [Google Scholar]
- 18.Murray ME, Buckenham TM, Joseph AE. The role of ultrasound in screening patients referred for sialography: a possible protocol. Clin Otolaryngol Allied Sci. 1996;21:21–23. doi: 10.1111/j.1365-2273.1996.tb01019.x. [DOI] [PubMed] [Google Scholar]
- 19.Haring JI. Diagnosing salivary stones. J Am Dent Assoc. 1991;122:75–76. doi: 10.14219/jada.archive.1991.0030. [DOI] [PubMed] [Google Scholar]
- 20.Rzymska-Grala I, Stopa Z, Grala B, Gołębiowski M, Wanyura H, Zuchowska A, et al. Salivary gland calculi - contemporary methods of imaging. Pol J Radiol. 2010;75:25–37. [PMC free article] [PubMed] [Google Scholar]
- 21.Sumi M, Izumi M, Yonetsu K, Nakamura T. The MR imaging assessment of submandibular gland sialoadenitis secondary to sialolithiasis: correlation with CT and histopathologic findings. AJNR Am J Neuroradiol. 1999;20:1737–1743. [PMC free article] [PubMed] [Google Scholar]
- 22.Thoeny HC. Imaging of salivary gland tumours. Cancer Imaging. 2007;7:52–62. doi: 10.1102/1470-7330.2007.0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee YY, Wong KT, King AD, Ahuja AT. Imaging of salivary gland tumours. Eur J Radiol. 2008;66:419–436. doi: 10.1016/j.ejrad.2008.01.027. [DOI] [PubMed] [Google Scholar]
- 24.Jadu F, Yaffe MJ, Lam EW. A comparative study of the effective radiation doses from cone beam computed tomography and plain radiography for sialography. Dentomaxillofac Radiol. 2010;39:257–263. doi: 10.1259/dmfr/62878962. [DOI] [PMC free article] [PubMed] [Google Scholar]