Abstract
A 14-year-old girl was referred for evaluation of headache with episodes of transient blurring of vision, and intermittent fever for 4 weeks. On examination she was conscious and febrile, with multiple annular purpuric skin lesions present over the face and back. Neurological examination revealed a bilaterally extensor plantar response, with bilateral papilloedema. Lumbar puncture yielded clear spinal fluid with a very high opening pressure with a normal biochemistry and cytology. Neuroimaging showed evidence of raised intracranial tension. She was provisionally diagnosed to have idiopathic intracranial hypertension (IIH) and started on anticerebral oedema measures. Despite medication, she continued to be symptomatic. On the sixth day of admission, her antinuclear antibody and antidouble-stranded DNA registered positively in high titres. She was diagnosed with systemic lupus erythematosus (SLE) with IIH and was started on corticosteroids, with dramatic recovery of her symptoms and clinical signs. Reports of SLE, the maiden presentation of which is IIH, are rare in the literature.
Background
Idiopathic intracranial hypertension (IIH) is a condition that affects predominantly overweight women and is characterised by raised intracranial pressure without any identifiable pathology in the brain and with normal cerebrospinal fluid (CSF) composition. The cause of IIH is unclear, and as such, it remains a diagnosis of exclusion. Systemic lupus erythematosus (SLE) is a multisystem connective tissue disease of unknown cause in which tissues and cells are damaged by pathogenic autoantibody and immune complexes. Headache is a common symptom in patients with SLE and occurs due to various causes. IIH is an uncommon syndrome of neuropsychiatric SLE and one of the causes of headache in SLE. Even while definitive criteria exist for diagnosing SLE, the initial presentation may be so camouflaging that a high index of suspicion should be present when making a diagnosis. Compounding this is the fact that the currently updated textbooks of medicine do not describe IIH as among the neuropsychiatric manifestations of SLE.1
Case presentation
A 14-year-old girl presented with a history of headache, episodes of transient blurring of vision and bilateral throbbing hemicranial headache. Visual obscuration lasted only for a few minutes. There was postural variation with the blurring of vision intensifying on getting up from a lying down position. There was no diplopia. She also had high-grade intermittent fever with no chills or rigour fever for 4 weeks. It was getting relieved spontaneously. There was no associated dysuria, loose stools, throat pain, earache, cough or dyspnoea. There was no history of associated joint pain. One week before presentation, she also noticed reddish, scaly lesions over both sides of the cheek which gradually turned darker over the course of 1 week. It was non-pruritic with no photosensitivity. There was no history of seizures or behavioural abnormalities. She gave a history of loss of appetite and loss of weight over the previous few months. She had been having irregular menstrual periods for the previous 3 months and had noticed neck swelling over the previous 2 months. There was no history of loss of hair, photosensitivity, recurrent oral ulcers, abdominal pain or skin rash, of prior hospitalisations, or of prolonged drug intake (figure 1A).
Figure 1.

(A) Photograph of a face with skin rashes sparing the bridge of the nose and malar area. (B) Photograph showing asymmetric hyperpigmented, polycyclic and annular scaly plaques with scaling involving the preauricular area and cheek.
Upon examination, she was moderately built thin. She had a temperature of 36.4°C, pulse rate was 98/min, blood pressure was 110/70 mm Hg in the right upper limb in the supine position and her respiratory rate was 16/min. She was pale, and her submandibular and jugulodigastric nodes were enlarged 1.5 cm, non-matted and non-tender, with no icterus, cyanosis, clubbing or oedema. Multiple erythematous annular purpuric skin lesions were present over the face and back. The thyroid gland was enlarged. Neurological examination showed bilateral extensor plantar response and papilloedema (figure 2A,B). There was no neck stiffness. Abdominal examination showed minimal hepatomegaly. Cardiovascular and respiratory system examination were normal.
Figure 2.
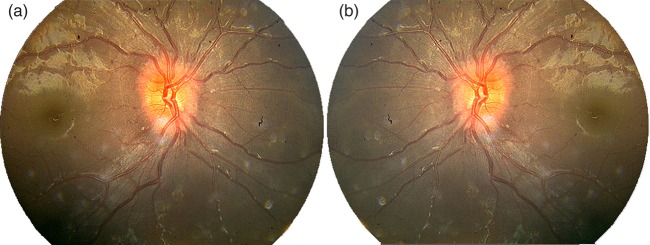
(A) Right optic fundus showing papilloedema and exudates. (B) Left optic fundus showing papilloedema and exudates.
Investigations
Investigations on day 1 are summarised in table 1. Peripheral smear examination was suggestive of hypochromic microcytic anaemia. Urine albumin was present in trace amounts with no red blood cells or casts. A CT scan of the brain done on the same day was normal. On the second day of admission, a guarded lumbar puncture was carried out, which yielded clear CSF with a high opening pressure of 300 mm H2O. CSF glucose was 58 mg/dl (with a corresponding blood sugar of 83 mg/dl) and protein 14.4 mg/dl. CSF showed no cells and adenosine deaminase was 1.5 u/l. By the third day, the results of the Mantoux test, rapid malaria test, serologies for immunoglobulin (Ig) M dengue virus infection, IgM scrub typhus and IgM leptospirosis were found to be negative. HBsAg was non-reactive. Anti-HCV, HIV 1 and 11 and VDRL were also reported as negative. Fine-needle aspiration cytology (FNAC) performed on the third day from the lymph nodes was normal, and FNAC from the thyroid showed lymphocytic thyroiditis. Tests for the antinuclear antibody and double-stranded DNA produced positive results by the fourth day of admission (table 1). On the same day, we proceeded with an MRI scan of the brain, which showed a flattening of the posterior sclera of the globe bilaterally with mild perioptic space prominence and associated herniation of CSF space into the sella (figure 3A,B). There were no focal lesions in the brain. The MR venogram showed no evidence of dural venous thrombosis.
Table 1.
Results of investigations summarised in chronological sequence
| Haemoglobin | 8.3 g/dl |
| Total leucocyte count | 3000/µl |
| Neutrophils | 60% |
| Lymphocytes | 34% |
| Eosinophils | 6% |
| Platelet count | 110×109/l |
| Erythrocyte sedimentation rate | 134 mm/h |
| Urine protein creatine ratio | 0.16 |
| Serum ferritin | 393.8 ng/ml |
| Serum bilirubin | 1.6 mg/dl |
| Serum glutamateoxaloacetate transaminase | 75 IU/l |
| Serum glutamate pyruvate transaminase | 28 IU/l |
| Serum sodium | 134 meq/dl |
| Serum potassium | 4 meq/dl |
| Blood urea | 35 mg/dl |
| Serum creatine | 1.2 g/dl |
| Uric acid | 3.6 mg/dl |
| TSH | 46.3 µIU/ml |
| Free T4 | 0.648 ng/dl |
| Free T3 | 2.86 pg/ml (2.02–4.43) |
| Antithyro-peroxidise antibody | 579 IU/ml |
| Antinuclear antibody | 30.4 U/ml (positive >10). |
| Antidouble-stranded DNA | 300 IU/ml (positive >55). |
| C-ANCA | Negative |
| P-ANCA | Negative |
| Antiphospholipid antibodies IgM | Negative |
| Antiphospholipid antibodies IgG | Negative |
ANCA, antineutrophil cytoplasmic antibodies; Ig, immunoglobulin; TSH, thyroid stimulating hormone
Figure 3.
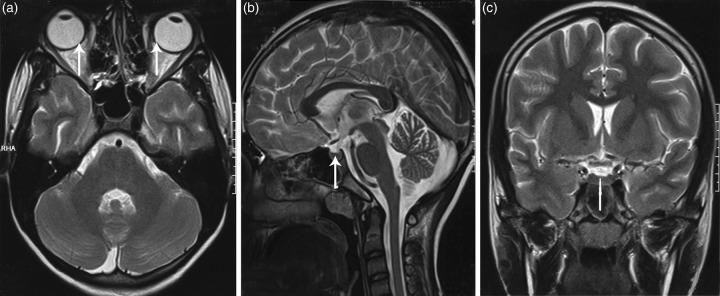
MRI showing (A) flattening of the posterior sclera of the globe bilaterally with mild perioptic space prominence (white arrows), no focal lesions in the brain or any evidence of dural venous thrombosis; (B) herniation of cerebrospinal fluid space into the sella (white arrow) and (C) MR venogram coronal section showing no focal lesion or dural venous thrombosis.
Differential diagnosis
The patient was diagnosed with SLE with IIH and lymphocytic thyroiditis. The other differentials considered were dural venous sinus thrombosis, hydrocephalus, cerebral mass lesions, hypertensive encephalopathy, optic disc anomalies (disc drusen and tilted optic disc), intracranial hypertension secondary to medications and systemic diseases.
Treatment
She was treated with intravenous mannitol, oral glycerine and methyl prednisolone 1 g once daily, which was started on the fourth day and was continued for 3 days followed by cyclophosphamide 25 milligrams daily.
Outcome and follow-up
The fever and headache subsided by the third day of initiating corticosteroids and she was fully symptom-free by 1 week. Repeat fundus examination after 5 days showed that papilloedema has decreased. She was discharged with cyclophosphamide tablets with an advice to review after 25 days.
Discussion
The syndrome of increased intracranial pressure without hydrocephalus or mass lesion and with normal CSF composition, previously referred to as benign intracranial hypertension, pseudotumour cerebri, is a diagnosis of exclusion that is now termed IIH.2 This syndrome of signs and symptoms of increased intracranial pressure does not show causative lesions on images obtained by MRI or CT.2 In 1968, Bettman et al3 first reported a patient with concomitant SLE and IIH. Since then, IIH has been reported in a few sporadic cases in adult patients with SLE.4 Neuropsychiatric SLE includes the neurological syndromes of the central, peripheral and autonomic nervous system and psychiatric syndromes observed in patients with SLE after excluding other causes. Neuropsychiatric affliction in SLE has become well established with a frequency of as much as 14–75%.5 The pathogenetic mechanism of IIH in SLE is not yet fully understood. It is not clear whether the overproduction of CSF, relative absorptive failure of CSF or increased cerebral blood flow is associated with the pathogenesis of IIH in SLE.4 Immune-mediated injury within the arachnoid villi and the resultant decrease in CSF absorption and/or thrombotic obliteration of cerebral arteriolar and venous systems due to a hypercoagulable state are among the most probable mechanisms.5–7 In our patient, even though the test for serum anticardiolipin antibody and lupus anticoagulant test were negative and no evidence of sagittal or other venous or arterial thromboses was demonstrated in MRI,6 autoimmunity could have contributed to IIH and thyroiditis. A recent retrospective study by Kim et al8 in 2012 found that, in 1084 patients with SLE, 8 suffered from IIH, out of 47 investigated with lumbar puncture, because of intractable headache. Dave et al9 found that 1% of his 410 patients with SLE had IIH (4 in 410). The conclusion from this study adequately describes the level of available evidence: ‘The association of SLE and IIH may occur more than by chance alone’.9 The association of IIH and SLE is probably not coincidental.10 The high prevalence of serological or clinical evidence of a hypercoagulable state suggests that microscopic thromboembolic events play a role in the genesis of IIH.7 However, the occurrence of this unusual neuro-ophthalmological presentation is infrequently encountered.4 IIH is an uncommon manifestation of neuropsychiatric SLE.4 11 SLE-associated IIH usually indicates a favourable outcome.11 The most critical sequela of IIH is permanent visual impairment. Furthermore, recurrent IIH, chronic low-grade papilloedema and death from progressive renal disease have been observed in some patients.11 Corticosteroid is currently the mainstay of the treatment of IIH in patients with SLE,12 and acetazolamide, intravenous mannitol and frusemide are also used to reduce the intracranial tension.11 In addition, plasmapheresis, azathioprine, cyclophosphamide and other immunosuppressive agents can be used in the treatment of such patients.11 In their review article, Dhungana et al13 provide a comprehensive list of systemic diseases and medications associated with IIH. Even though considered an idiopathic syndrome, many systemic diseases such as hypothyroidism, collagen vascular diseases, anaemia, antiphospholipid antibody syndrome and hypervitaminosis A have been found to lead to the syndrome of IIH.13
A thorough and meticulous search for such initially obscure secondary causes often turns out to be rewarding in arriving at the aetiology, as was demonstrated in our case. Such a search would also save the patient from unnecessary repeated lumbar punctures and shunt surgeries, because treating the primary problem could lead to total resolution of the symptoms and complications of IIH. In our case, the presence of fever, rashes and haematological findings prompted our search for secondary causes of raised ICT and IIH-like presentation.
Conclusion
IIH presenting as a severe, unremitting headache may be the first manifestation of SLE. In view of the camouflaging presentations of SLE, it is prudent to work-up for autoantibodies, prothrombotic factors and imaging studies in a woman presenting with headache and fever in order to confirm the diagnosis. Even in the latest literature, the prevalence of IIH as a premonitory manifestation of SLE is underestimated. But in any case of IIH, a screening for dyscollagenosis is in order. As more of such aetiological factors emerge for IIH, the nomenclature and the ‘Idiopathic’ terminology may disappear in the future.
Learning points.
Even in the latest textbooks of Internal Medicine, idiopathic intracranial hypertension (IIH) is not mentioned as a major complication of neurolupus. It will be relevant to include IIH in the spectrum of neuropsychiatric manifestations of systemic lupus erythematosus (SLE).
IIH presenting as a severe, unremitting headache may be the first manifestation of SLE.
The association of IIH and SLE is probably not coincidental. The high prevalence of serological or clinical evidence of a hypercoagulable state suggests that microscopical thromboembolic events play a role in the genesis of pseudotumour cerebri.10
While not life threatening, IIH has a significant morbidity with up to 25% of patients developing visual impairment from optic atrophy. Visual surveillance is, therefore, vital. Long-term follow-up is recommended as the disease may worsen after an initial period of stability.12
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Hahn BH. Systemic lupus erythematosus in Harrisons principles of internal medicine. 18th edn New York: Mac Graw Hill, 2012:2724–35 [Google Scholar]
- 2.Friedman DI, Jacobson DM. Diagnostic criteria for idiopathic intracranial hypertension. Neurology 2002;59:1492–5 [DOI] [PubMed] [Google Scholar]
- 3.Bettman JW, Jr, Daroff RB, Sanders MD, et al. Papilloedema and asymptomatic intracranial hypertension in systemic lupus erytheymatosus. A fluorescein angiographic study of resolving papilloedema. Arch Ophthamol 1968:80:189–93 [DOI] [PubMed] [Google Scholar]
- 4.Li EK, Ho PCP. Pseudotumor cerebri in systemic lupus erythematosus. J Rheumatol 1989;16:113–16 [PubMed] [Google Scholar]
- 5.Horoshovski D, Amital H, Katz M, et al. Pseudotumor cerebri in SLE. Clin Rheumatol 1995;14:708–10 [DOI] [PubMed] [Google Scholar]
- 6.Shiozawa Z, Yoshida M, Kobayashi K, et al. Superior sagittal sinus thrombosis and systemic lupus erythematosis. Ann Neurol 1986;20:272. [DOI] [PubMed] [Google Scholar]
- 7.Green L, Vinker S, Amital H, et al. Pseudotumor cerebri in systemic lupus erythematosus. Semin Arthritis Rheum 1995;25:103–8 [DOI] [PubMed] [Google Scholar]
- 8.Kim JM, Kwok SK, Ju JH, et al. Idiopathic intracranial hypertension as a significant cause of intractable headache in patients with systemic lupus erythematosus: a 15-year experience. Lupus 2012;21:542–7 [DOI] [PubMed] [Google Scholar]
- 9.Dave S, Longmuir R, Shah VA, et al. Intracranial hypertension in systemic lupus erythematosus. Semin Ophthalmol 2008;23:127–33 [DOI] [PubMed] [Google Scholar]
- 10.Padeh S, Passwell JH. Systemic lupus erythematosus presenting as idiopathic intracranial hypertension. J Rheumatol 1996;23:1266–8 [PubMed] [Google Scholar]
- 11.Yoo WH, Park JH, Kim HK, et al. Recurrent pseudotumor cerebri in systemic lupus erythematosus: a case report. J Korean Med Sci 2001;16:805–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hershko AY, Berkun Y, Mevorach D, et al. Increased intracranial pressure related to systemic lupus erythematosus: a 26-year experience. Semin Arthritis Rheum 2008;38:110–15 [DOI] [PubMed] [Google Scholar]
- 13.Dhungana S, Sharrack B, Woodroofe N. Idiopathic intracranial hypertension. Acta Neurol Scand 2010;121:71–82 [DOI] [PubMed] [Google Scholar]


