Abstract
Takayasu's arteritis (TA) is a chronic inflammatory disease of medium and large vessels, mainly involving the aorta and its major branches. TA may have diverse clinical presentation including claudication, stroke, asymmetric pulse or blood pressure. However, the association of TA with digital gangrene is a rare entity. Here, we report a case of a 40-year-old woman who presented with digital gangrene of the right hand, which on workup was diagnosed as a case of TA.
Background
Digital gangrene is a manifestation of systemic diseases like diabetes, vasculitis, thrombophilic states or infections. It requires detailed evaluation and timely treatment to prevent further progression of disease. Vasculitis is an important cause of digital gangrene. However, digital gangrene has rarely been reported in large vessel vasculitis such as Takayasu's arteritis (TA).
TA is a chronic inflammatory disease of large vessels predominantly involving the aorta and its major branches.1 TA predominantly presents as claudication, stroke, asymmetric pulse or blood pressure.2 Digital gangrene in association with TA is a rare manifestation. Till now, very few cases of TA with isolated lower limb gangrene have been reported.3 4 This is a rare case of TA presenting with digital gangrene of the right hand.
Case presentation
A 40-year-old woman presented with chief complaints of intermittent claudication of the right upper limb for 6 months and black discolouration of index and little fingers of right hand for 2 months. There was no history of diabetes mellitus, hypertension, trauma, rest pain, other thrombotic episodes, raynauds phenomena, cerebrovascular accident, rashes, joint or abdominal pain, oral ulcers or any previous drug intake. The patient was a non-smoker, married with four uneventful pregnancies. Family history was not significant. On examination, blood pressure was 96/70 mm Hg in the right arm, 130/76 mm Hg in left arm, 144/70 mm Hg in right leg and 148/80 mm Hg in the left leg. The pulse was 76/min, regular with brachial and radial pulses feeble on the right side as compared with left while femoral, popliteal and pedal pulses were bilaterally equally palpable. Bruit was audible over the right subclavian artery. Local examination of right hand showed evidence of dry gangrene in index and little fingers, with a line of demarcation between the normal and the gangrenous area. Detailed systemic examination did not reveal any obvious abnormality.
Investigations
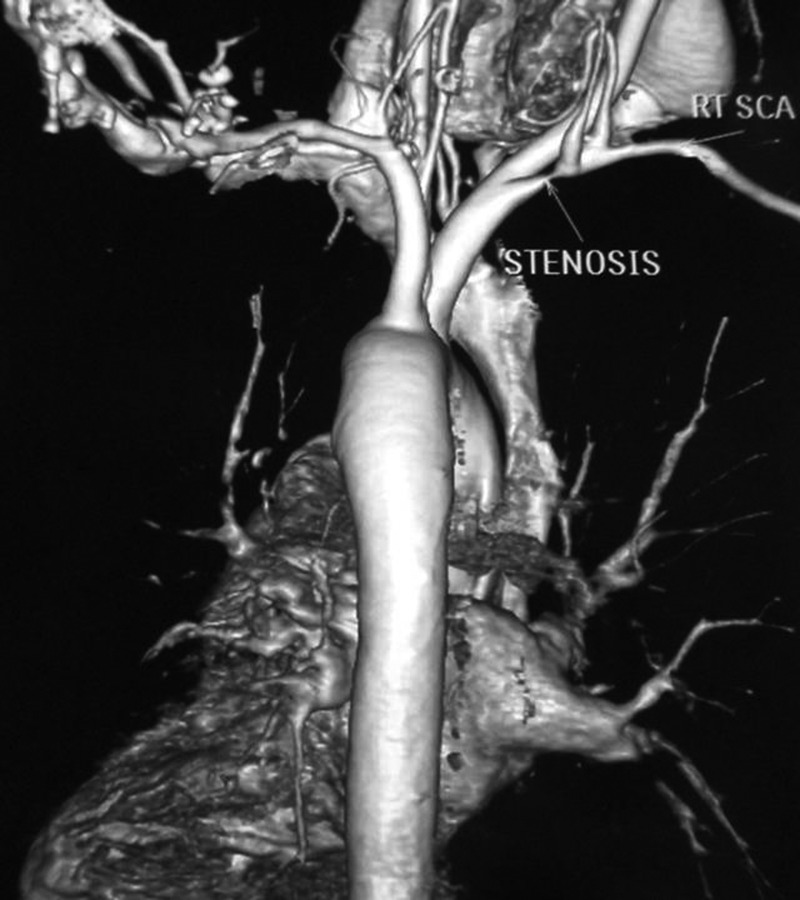
Investigations showed: haemoglobin 7.5 gm/dl, total leucocyte count 75.00/mm3 (68% neutrophils and 32% lymphocytes), platelet counts 2.2 lacs/mm3, random blood sugar 85 mg/dl, blood urea 24 mg/dl, serum creatinine 0.5 mg/dl and erythrocyte sedimentation rate greater than 96 mm/h. Antinuclear antibody, perinuclear antineutrophil cytoplasmic antibody, cytoplasmic antineutrophil cytoplasmic antibody, hepatitis B surface antigen, hepatitis C virus and HIV status were negative. x-ray chest posterioanterior view was normal. CT aortography revealed small segment severe stenosis of right subclavian artery proximal to the origin of vertebral artery with thickened wall and mild poststenotic dilation (figure 1). According to current angiographic classification of TA (table 1), our patient falls under type I.
Figure 1.
CT aortography showing severe stenosis of right subclavian artery.
Table 1.
Angiographic classification of Takayasu's arteritis
| Type | Vessel involvement |
|---|---|
| Type I | Main branches of the aortic arch |
| Type IIa | Ascending aorta, aortic arch and its branches |
| Type IIb | Ascending aorta, aortic arch and its branches and thoracic descending aorta |
| Type III | Thoracic descending aorta, abdominal aorta and/or renal arteries |
| Type IV | Abdominal aorta and/or renal arteries |
| Type V | Types IIb and IV occurring together |
Differential diagnosis
Atherosclerotic vascular disease
Buerger's disease
Inflammatory aortitis (eg, lupus and tuberculosis)
Treatment
The patient was prescribed prednisolone 40 mg/day. The patient was referred to cardiothoracic vascular surgery department for digital gangrene where surgical debridement followed by amputation of index and ring finger was performed (figure 2).
Figure 2.

Right hand with amputated index and little fingers.
Outcome and follow-up
Appropriate medical and surgical treatment led to relief of symptoms.
Discussion
Vasculitis is an important cause of digital gangrene. Among vasculitis syndromes, systemic lupus erythematosis (SLE) is the most common cause of digital ischaemia followed by medium and small vessel vasculitis such as polyarteritis nodosa (28–58%), Wegener's granulomatosis (30–40%) and microscopic polyangitis (15–20%).5 6
SLE is characterised by multisystem involvement requiring at least 4 of 11 clinical and laboratory diagnostic criteria. Polyarteritis nodosa commonly presents with cutaneous necrotising rashes and digital gangrene. However, in the absence of mesenteric arterial involvement or neuropathies, the diagnosis is difficult. Wegener's granulomatosis mostly presents with respiratory tract symptoms together with features of renal involvement. Buerger's disease can also cause claudication and digital gangrene with ulcers in more than 70% of cases. It is commonly associated with smoking and is uncommonly seen in women.
The diagnosis of TA can be made reliably based on the established American College of Rheumatology criteria (table 2).7 The diagnosis can be made if three of the six criteria are met. This standard yields a sensitivity of 91% and a specificity of 97%. Our patient met all the criteria for the diagnosis of TA.
Table 2.
Criteria of American College of Rheumatology for classification of Takayasu arteritis
| Criteria | Definition |
|---|---|
| Age at disease onset in years | Development of symptoms or findings related to Takayasu arteritis at age <40 years |
| Claudication of extremities | Development and worsening of fatigue and discomfort in muscles of one or more extremities while in use, especially the upper extremities |
| Decreased brachial artery pulse | Decreased pulsation of one or both brachial arteries |
| Blood pressure difference >10 mm Hg | Difference of >10 mm Hg in systolic blood pressure between arms |
| Bruit over subclavian arteries or aorta | Bruit audible on auscultation over one or both subclavian arteries or abdominal aorta |
| Arteriogram abnormality | Arteriographic narrowing or occlusion of the entire aorta, its primary branches, or large arteries in the proximal upper or lower extremities, not due to arteriosclerosis, fibro-muscular dysplasia, or similar causes: changes usually focal or segmental |
Till now, the occurrence of digital gangrene in TA is reported in lower limbs only. Moreover, symptomatic upper limb digital gangrene is uncommon because of the abundant collaterals and the infrequency of atherosclerosis in the upper extremity. Hence, occurrence of digital gangrene in the upper limb in association with TA, as seen in our patient, is a very rare presentation. One should always consider the differential diagnosis of TA in patients presenting with digital gangrene for early diagnosis and treatment.
Learning points.
Digital gangrene is a feature of systemic diseases like diabetes, vasculitis, thrombophilic states or infections.
Digital gangrene of the upper limb may be rarely seen in Takayasu's arteritis (TA).
One should always consider the differential diagnosis of TA in patients presenting with digital gangrene.
Early diagnosis and appropriate treatment may prevent further progression of disease.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Johnston SL, Lock RJ, Gompels MM. Takayasu arteritis: a review. J Clin Pathol 2002;55:481–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lie J. Aortic and extracranial large vessel giant cell arteritis: a review of 72 cases with histopathologic documentation. Sem Arthritis Rheum 1995;24:422–31 [DOI] [PubMed] [Google Scholar]
- 3.Al-Alawi E, Taraif S. Takayasu's arteritis as a cause of peripheral vascular insufficiency: a case report. J Bahrain Med Soc 2009;21;353–5 [Google Scholar]
- 4.Fielder JFA. 23-Year-old woman admitted to Kijabe Mission Hospital with bilateral lower extremity gangrene. MedGen Med 2004;6:56. [PMC free article] [PubMed] [Google Scholar]
- 5.Dieter RS, Dieter RA, Jr, Dieter RA, III, eds. Peripheral arterial disease. 1st edn. New York,: McGraw-Hill Professional, 2009: 197–233 [Google Scholar]
- 6.Balls GV, Bridges SL, eds. Vasculitis. 2nd edn Oxford: Oxford University Press, 2008: 439–61 [Google Scholar]
- 7.Arend WP, Michel BA, Block MA, et al. The American college of rheumatology 1990 criteria for the classification of Takayasu arteritis. Arthritis Rheum 1990;330:1129. [DOI] [PubMed] [Google Scholar]