Abstract
We report a 25-year-old young man presenting with cognitive decline, pancerebellar features, spastic quadriparesis, bilateral cataract (operated) and tendo-Achilles swelling (xanthoma). The CT of the head showed bilateral cerebellar hypodensities. There were bilateral cerebellar hypointensities involving dentate nuclei on T1-weighted images with corresponding hyperintensities on T2-weighted MRI. Additionally, an interesting MRI finding—‘hot cross bun’ appearance was seen in pons which has not been reported in the literature so far. Biopsy from tendo-Achilles confirmed xanthoma. He was treated with chenodeoxycholic acid following which he showed improvement in cognition and weakness.
Case presentation
A 25-year-old man born of a consanguineous marriage, with normal birth and developmental history, presented with a history of insidious onset and gradually progressive cognitive decline, pancerebellar features and spastic quadriparesis since 6–7 years. He was operated for bilateral cataract at the age of 12 years. There was no history of seizures. Neuropsychological tests indicated mental retardation with an intelligence quotient of 60. Patient had bilateral aphakic eyes and fundus was normal. Slit lamp examination for Kayser-Fleischer ring was negative. He also had a small swelling in the tendo-Achilles which was clinically suggestive of xanthoma (figure 1). Neurological examination revealed Mini-Mental State Examination (MMSE) scores of 12/30. He had behavioural abnormalities like irritability, temper tantrums and panic attacks. He also had motor weakness in all the four limbs (4/5 in the upper limbs and 3/5 in lower limbs), associated with spasticity, generalised hyper-reflexia, bilateral ankle clonus and positive Babinski sign. There were pancerebellar features in the form of titubation, nystagmus, scanning speech, truncal ataxia and finger–nose coordination without any asymmetry. However, there were no extrapyramidal features and sensory system examination was normal.
Figure 1.

Tendon xanthoma of the Achilles tendon, a common site in cerebrotendinous xanthomatosis.
Investigations
His routine laboratory examination showed normal haemogram, renal and liver function tests. Lipid profile showed a low total cholesterol of 124 mg/dl. His 24 h urinary copper excretion was normal. ECG, two-dimensional echocardiography of the heart, ultrasound of the abdomen, nerve conduction studies and electromyogram were all within the normal limits.
CT of the head showed bilateral cerebellar hypodensities which was reconfirmed with an MRI which revealed hypointensities in the cerebellum bilaterally involving the dentate nuclei on T1-weighted images, which were hyperintense on T2-weighted images (figure 2). Additionally, there was an interesting finding of ‘hot cross bun’ (HCB) appearance in the pons (figure 3). Periventricular white matter changes were also observed.
Figure 2.

MRI of the cerebellum showing hyperintensities in the bilateral dentate nuclei—a site classically affected in cerebrotendinous xanthomatosis.
Figure 3.

MRI T2-weighted axial image showing ‘hot cross bun’ sign in pons.
An MRI of tendo-Achilles revealed hypointensity on T1-weighted images (figure 4). Fine needle aspiration cytology of tendo-Achilles swelling was inconclusive, but biopsy of the same revealed abnormal foamy macrophages with foreign body type and Touton giant cells, which were surrounding the cholesterol clefts within the fibrocollagenous tissue which was suggestive of a xanthoma (figures 5 and 6). Serum cholestanol estimation and genetic analysis could not be performed because of the lack of resources.
Figure 4.

MRI T1-weighted image of Achilles tendon showing hypointense lesion.
Figure 5.

Microphotograph showing Touton giant cell with wreath like nuclei and extracellular lipid and foamy macrophages (H&E ×400).
Figure 6.
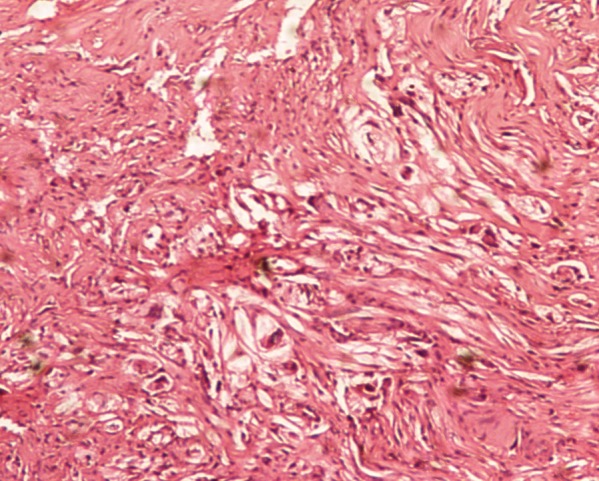
Microphotograph showing foamy macrophages, extracellular lipid and numerous cholesterol clefts (H&E ×400).
Differential diagnosis
▸ Marinesco-Sjogren syndrome
Treatment
The patient was treated with oral chenodeoxycholic acid (CDCA) of 750 mg daily in three divided doses.
Outcome and follow-up
The patient was started on oral CDCA 750 mg daily in three divided doses. He is under regular follow-up for the last 1 year and has shown improvement in his cognition and weakness. His repeat MMSE score was 15/30 and there was an improvement in his attention and behaviour.
Discussion
Cerebrotendinous xanthomatosis (CTX) is a potentially treatable condition and an early diagnosis can prevent progression of the disease. Treatment with CDCA has raised interest towards this rare disease as there is evidence of reversibility in some of the neurological features.1
In CTX, there is an abnormal storage of cholesterol owing to defective enzymatic pathway of bile acid synthesis leading to the accumulation of cholesterol precursors, particularly cholestanol in various tissues with a predilection for brain, liver, lungs and tendons.2 Usually tendon xanthomas are seen in Achilles tendon which is considered as a hallmark sign.3 But cases of CTX without tendon xanthomas mimicking the Marinesco-Sjogren syndrome have also been reported by Sieber et al.4
Though xanthomas can be associated with many other diseases of cholesterol derangement, particularly with hypercholesterolaemia or hyperlipoproteinemia, but in CTX, xanthomas are associated with normal or low serum cholesterol as in this patient.5 In CTX, xanthoma formation occurs because of abnormal cholestanol accumulation in various tissues rather than cholesterol.5
In CTX, xanthomas also occur in the nervous system with a predilection for cerebellum particularly the dentate nuclei leading to bilateral non-homogenous, hyperintense signal on MRI T2-weighted images which can be considered as the neuroradiological diagnostic marker.6 Pathological examination has shown prominent cerebellar involvement owing to extensive granulomatous lesions that replace the cerebellar white matter.2 Fiorelli et al7 described a patient presenting with dementia, spastic tetraparesis, cerebellar features, seizures and bilateral cataracts showing bilateral cerebellar lesions on CT and MRI.
Our patient presented with cognitive decline, pancerebellar features, spastic quadriparesis and bilateral juvenile cataract (operated). Clinical examination revealed swelling of bilateral tendo-Achilles, though small, raising high the index of suspicion of CTX . These xanthomas were confirmed by the histopathological examination after the radiological assessment. Though CT of the brain did show bilateral cerebellar hypodensities, an MRI of the brain showed classical hypointensities on T1-weighted images and hyperintensities on T2-weighted images in the corresponding areas particularly involving the dentate nuclei.
Additionally, an MRI of the brain revealed a very interesting finding in our patient's HCB sign in the pons. HCB sign is classically described in cerebellar type of multiple system atrophy (MSA-C). In MSA-C, the degeneration of pontine neurons, gliosis and loss of myelinated transverse fibres with preserved tegmentum and corticospinal tracts is considered as a cause of HCB sign, which is a cruciform hyperintensity in the pons best seen on the axial T2-weighted and fluid-attenuated inversion recovery (FLAIR) sequence.8 HCB sign has also been described in spinocerebellar ataxia types 2 and 3,9 in a variant of Creutzfeldt-Jakob disease10 and in a case of severe Parkinsonian syndrome associated with cerebellar and brainstem dysfunction owing to presumed vasculitis.11 Yadav et al12 reported HIV-related progressive multifocal leucoencephalopathy as a rare cause of HCB sign in two of their patients. To the best of our knowledge HCB sign in CTX has not been reported so far in the literature as seen in our patient.
We suggest that whenever a young patient presents with juvenile cataract, cognitive decline, cerebellar features and spastic tetraparesis, tendon xanthomas should be carefully looked particularly in Achilles tendon. An MRI of the brain, and if possible an MRI of tendo-Achilles, should also be performed to look for classical radiological findings. Though serum cholestanol estimation would be diagnostic, we strongly recommend biopsy of the tendon swelling to confirm xanthoma when resources for serum cholestanol estimation are not available. CTX should be ruled out before labelling any patient with aforementioned clinical features as degenerative brain disease since we have a simple and non-expensive treatment to offer which can prevent the progression of disease and at times can even reverse some of the neurological manifestations.
Learning points.
We suggest that whenever a patient presents with juvenile cataract, cognitive decline, cerebellar features and spastic tetraparesis every attempt should be made to look carefully for tendon xanthomas particularly in Achilles tendon.
An MRI of the brain, and if possible of tendo-Achilles, should also be performed to look for classical radiological findings.
Though serum cholestanol estimation would be diagnostic, we strongly recommend biopsy of swelling to confirm xanthoma when the required facility for serum cholestanol is not available.
CTX should be ruled out before labelling any patient with aforementioned clinical features as degenerative brain disease since we have treatment to offer which can prevent the progression of disease and at times can even reverse some of the neurological manifestations.
Lastly, hereafter CTX can be listed as one of the causes for ‘hot cross bun’ sign, though rare.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Berginer VM, Salen G, Shefer S. Long-term treatment of cerebrotendinous xanthomatosis with chenodeoxycholic acid . N Engl J Med 1984;311:1649–52 [DOI] [PubMed] [Google Scholar]
- 2.Van Bogaert L, Scherer HJ, Froelich A, et al. Une deuxieme observation de cholesterinose tendineuse symetrique avec symptoms cerebraux. Ann Med 1937;42:69–101 [Google Scholar]
- 3.Berginer VM, Salen G, Shefer S. Cerebrotendinous xanthomatosis. In: Rosenberg RN, Prusiner S, DiMauro S, et al. eds. The molecular and genetic basis of neurological disease. London: Butterworths, 1993:295–305 [Google Scholar]
- 4.Siebner HR, Berndt S, Conrad B. Cerebrotendinous xanthomatosis with out tendon xanthoma mimicking Marinesco-Sjogren syndrome: a case report. J Neurol Neurosurg Psychiatry 1996;60:582–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.De Jong JG, Van Grent CM, Delleman JM. Cerebrotendinous cholestanolosis in relation to other cerebralxanthomatosis . Clin Neurol Neurosurg 1997;79:253–72 [DOI] [PubMed] [Google Scholar]
- 6.Salen G, Berginer V, Shore V. Increased concentrations of cholestanol and apolipoprotein B in the cerebrospinal fluid of patients with cerebrotendinous xanthomatosis: effect of chenodeoxycholic acid. N Engl J Med 1987;316:1233–8 [DOI] [PubMed] [Google Scholar]
- 7.Fiorelli M, Piero VD, Bastieanello S, et al. Cerebrotendinous xanthomatosis: clinical and MRI study (a case report). J Neurol Neurosurg Psychiatry 1990;53:76–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schrag A, Kingsley D, Phatouros C, et al. Clinical usefulness of magnetic resonance imaging in multiple system atrophy . J Neurol Neurosurg Psychiatry 1998;65:65–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee YC, Lin CS, Wn HM, et al. The “Hot-cross bun sign” in the patients with spinocerebellar ataxia. Eur J Neurol 2009;16:513–16 [DOI] [PubMed] [Google Scholar]
- 10.Soares-Fernandes JP, Ribeiro M, Machado A. “Hot cross bun” sign in variant Creutzfeldt-Jakob disease. AJNR Am J Neuroradiol 2009;30:E37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Muqit MM, Mort D, Miskiel KA, et al. “Hot cross bun” sign in a patient with parkinsonism secondary to presumed vasculitis. J Neurol Neurosurg Psychiatry 2001;71:565–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yadav R, Ramdas M, Karthik N, et al. “Hot cross bun” sign in HIV-related progressive multifocal leukoncephalopathy. Neurol India 2011;59:293–4 [DOI] [PubMed] [Google Scholar]


