Abstract
Epidermolysis bullosa (EB) constitutes a group of phenotypically diverse genodermatoses, which manifests with blistering and erosions of the skin and mucous membranes as the unifying diagnostic feature. It is an acquired disease or inherited as either autosomal-dominant or recessive with an incidence of 1/50 000. The prominent clinical characteristic of the disease is the development of bullae or vesicles in mucosa or skin in response to minor trauma. It is a chronic mechanobullous disease characterised by auto antibodies against Type VII collagen. This paper documents a case of a man diagnosed with dominant dystrophic EB; describing the measures that dentists and healthcare providers should adopt in order to provide a safe and effective dental treatment. Early prevention protocols for these patients have also been discussed.
Background
Epidermolysis bullosa (EB) is a group of rare genetically determined disorders characterised by the development of blisters following minor trauma or traction to the skin and/or mucosal surfaces.1–3 It appears that the cause of EB is related to abnormal enzyme activity and collagen degradation. There are four major forms—simplex, junctional, dystrophic and Kindler syndrome.4
The dystrophic EB has two subtypes—recessive (RDEB) and dominant (DDEB).
The recessive dystrophic subtype of EB with generalised involvement is a dermatological condition producing serious mucosal lesions with sublamina dura separation, due to blistering below the lamina densa of basement membrane zone.
The prototypic dominant dystrophic subtype of EB is characterised by generalised blistering at birth which, with time, is associated with milia, atrophic (or less commonly, hypertrophic) scarring and nail dystrophy. Recurrent oesophageal blistering and erosions, leading to oesophageal stricture formation or progressive dysphagia, are common among these patients.
But other features of RDEB, that is failure to thrive, growth retardation, pseudosyndactyly, severe anaemia, early infant mortality and risk of squamous cell carcinoma are not characteristic features of DDEB.
Oral manifestations and dental involvement of EB vary in frequency, and severity according to the form. Intraoral manifestations include multiple carious lesions affecting almost the entire dentition, with severe gingival inflammation, microstomia, ankyloglossia and obliteration of oral vestibule.
Case presentation
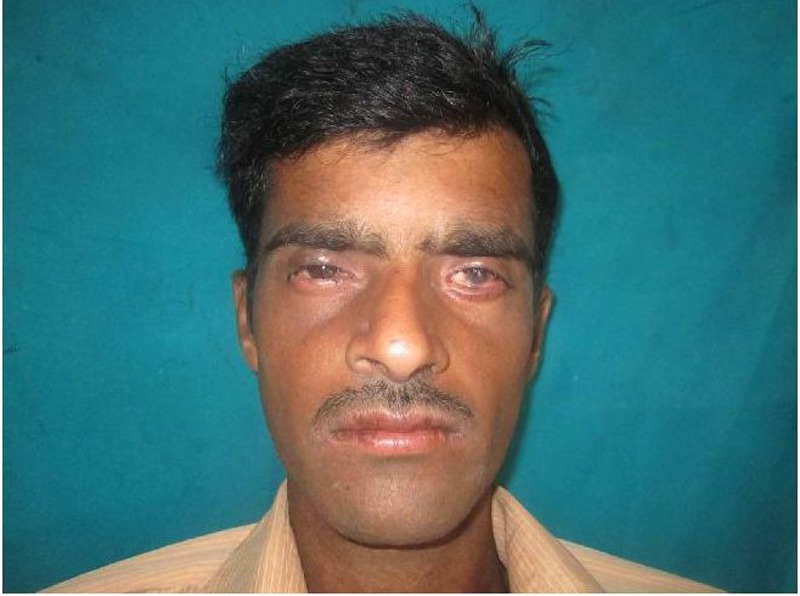
A 20-year-old male patient reported for treatment, with a chief complaint of multiple carious teeth and painful oral mucosa. History revealed that he has been developing small blisters over extremities following minor trauma. These blisters used to rupture and the erosions would heal with scarring. Familial history was insignificant. On examination, scars were present on lips and perioral mucosa (figure 1). Blistering lesions, healed scars with mottling pigmentation, milia and keratoderma (hyperkeratosis of palms and soles) were found on both hands and legs, as seen in figure 2. Nail dystrophy was also present as seen in figure 3. In addition, trichiasis (inward growth of eyelashes), chronic conjunctivitis and corneal opacification were seen (figure 4).
Figure 1.
Frontal photograph showing perioral lesions.
Figure 2.

Cutaneous lesions on hands and feet.
Figure 3.

Nail dystrophy.
Figure 4.

Trichiasis, conjunctivitis and corneal opacification.
Intraoral examination revealed multiple carious lesions (Rampant caries) affecting almost the entire dentition (figure 5), with severe gingival inflammation, erosive lesions in mandibular molar vestibular region and microstomia (figure 6). The tongue was found to be normal in size and attachment. Systemic examination showed no abnormality.
Figure 5.
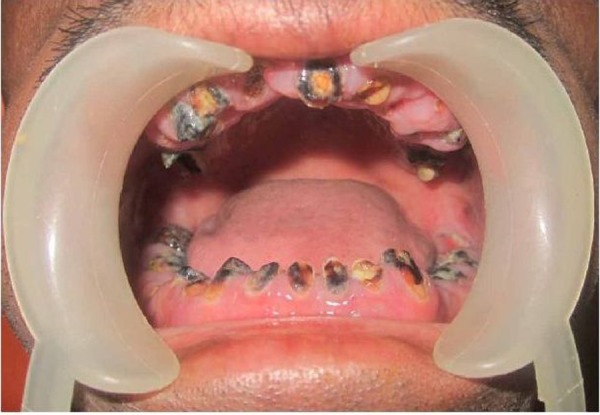
Rampant caries and healing oral lesions.
Figure 6.

Restricted mouth opening (microstomia).
Investigations
Routine laboratory investigations including complete blood counts, serum biochemistry and urine analysis were advised and the reports were essentially normal except for mild anameia (haemoglobin 8 mg%). Chest x-ray was also normal. Orthopantomogram (figure 7) showed the presence of root stumps of all teeth and multiple periapical lesions. Histopathological examination of skin biopsy specimen from a leg lesion showed hyperkeratosis, mild acanthosis, intact basal cells and sub-basal cleft (figure 8). There was mild interstitial and perivascular lymphocytic infiltrate in the upper and mid-dermis. Milia were also observed in few sections. On the basis of characteristic clinical and histological features a diagnosis of EB was made and the patient was counselled for genetic and prognostic implications of the disorder.
Figure 7.
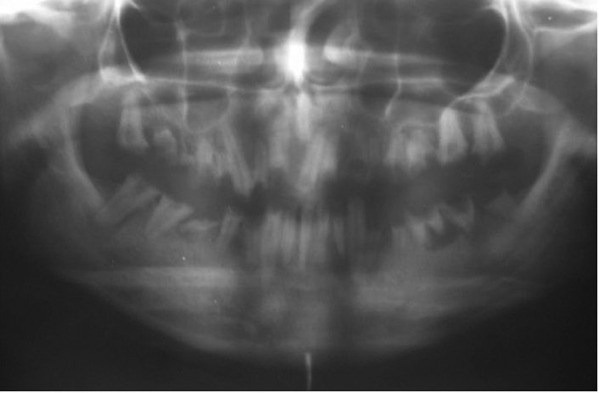
Orthopantomogram showing root stumps of all teeth with multiple periapical lesions.
Figure 8.
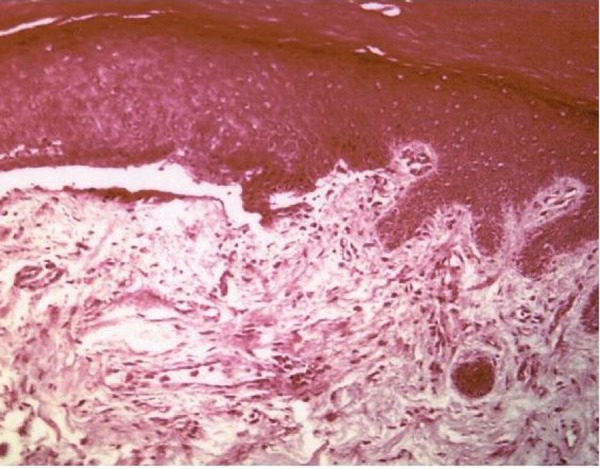
Histopathology section showing sub-basal cleavage.
Differential diagnosis
Herpes simplex
Systemic lupus erythmatosis
Mucous membrane pemphigus.
Treatment
There is no specific therapy for EB; treatment is both supportive and preventive.
Preventive
Genetic counselling was done. The patient was instructed to eat just soft foods and avoid hard/sticky foods and foods with high acidic content. He was advised to stop smoking, avoid trauma and cover the extensor skin surfaces with protective pads. Gentle but thorough daily oral hygiene was advised. The primary focus was on proper diagnosis, prevention of new lesions and to guard against infection.
Supportive
The goal of treatment in the present case was to prevent blisters from forming and its resulting complications. Topical steroids and antibiotics were used to promote healing and prevent secondary infection of blisters. Since restoration of teeth was not possible due to severe crown destruction, total extraction was done in two sittings under local anaesthesia. Implant supported denture is planned at a later date for dental rehabilitation. The patient was referred to an ophthalmologist and a gastroenterologist for the management of ocular and gastrointestinal lesions.
Outcome and follow-up
Follow-up is advised after every 6 months for the evaluation of oral status and to detect any early carcinomatous changes.
Discussion
EB is a group of rare genetically determined disorders characterised by the development of blisters following minor or insignificant trauma or traction to the skin or mucosal surfaces.1–3
There are four major forms—simplex, junctional, dystrophic and Kindler syndrome with more than 20 distinctive clinical subtypes.4 The prevalence of dominant and recessive dystrophic types of EB is 1–2.86%, and 0.92–2.04%, respectively, in 50 000 live births.5
Oral manifestations and dental involvement of EB vary in frequency, in severity and according to subtype.6 In the simplex form the teeth are not affected; however, the dystrophic types often display malformed teeth due to enamel hypoplasia, early caries development and gingival inflammation due to plaque accumulation.
In the present case the possibility of pemphigous, mucous membrane pemphigoid was ruled out due to the lack of clinically significant mechanical fragility or any of the other skin findings (milia, nail dystrophy and scarring) that are characteristic of inherited EB.
The goal of treatment is to prevent blisters from forming and complications. How much treatment is needed depends on how severe the disease is. To avoid skin damage and blistering it is recommended to wear padding around injury-prone areas. Contact sports should be avoided. Topical steroids and topical antibiotics are used to promote healing and prevent secondary infection of blisters. For swallowing difficulties, use of oral steroids is recommended for a short period of time. Dilation of the oesophagus may be required if there is narrowing (stricture). Repair of hand deformities is required in severe cases of pseudosyndactyly.
Dental treatment of these individuals is further complicated by their severe oral and perioral scarring, microstomia, ankyloglossia and obliteration of the oral vestibule.7 Thus, the treatment of the EB patient must be modified in order to decrease the effects of local trauma to the tissues. Oral ulceration due to trauma during dental manipulation is unavoidable, but it could be limited by the mucosa lubrication before any manipulation with hydrocortisone cream, triamcinalone or petroleum jelly.8 9 In addition, the use of small-sized instruments, short-shaft dental burs and handpieces with a small-sized head is indicated.9 Dentures and restorations should be carefully adapted and highly polished; secondary infections should be prevented with the use of oral antiseptics or using topical antibiotics on existing bullous lesions.10 During the dental treatment in outpatient settings, the administration of local anaesthesia to patients with EB may also cause blister formation and should therefore be avoided whenever possible.11 Nevertheless, when necessary, local anaesthetic should be injected slowly and deeply into the tissues to prevent mechanical tissue separation and blistering.
Regarding dental treatment under general anaesthesia, some authors12 affirm that it can be complicated since the intubation predisposes the patient to high risk of pharyngeal and tracheal lesions.
Owing to the difficulties related to the restorative dental treatment of these patients, the emphasis on the oral health management must be on prevention beginning at an early age. Daily application of topical and systemic fluoride, oral hygiene instructions and dietary guidelines minimise caries development and improves overall oral health.5 13
It is essential to preserve the natural dentition, as prosthetic rehabilitation is usually complicated, due to distortion of normal oral tissues by scarring. This makes the retention of dentures difficult, even if they can be tolerated.14
It is noteworthy that some dentists do not feel comfortable or prepared for treating special need individuals due to their lack of knowledge on the disease-specific manifestations and implications. We hope that the issues discussed in this paper can be helpful to elucidate the most relevant clinical aspects and typical oral findings of patients with EB and provide research-based information that can make oral health professionals more familiar with this condition and more qualified to offer a dental treatment of excellence.
Learning points.
Dominant dystrophic epidermolysis bullosa (EB) patient has generalised blistering at birth which, with time, is associated with milia, atrophic (or less commonly, hypertrophic) scarring, nail dystrophy, oesophageal stricture, dysphagia and ocular involvement.
Oral manifestations include Rampant caries, bullae formation leading to scars, severe gingival inflammation, ankyloglossia and microstomia.
Genetic counselling is recommended for prospective parents who have a family history of any form of EB.
Every precaution has to be taken to protect the skin and oral mucosal surfaces from trauma.
Follow-up is mandatory to detect any early carcinomatous changes.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Carroll DL, Stephan MJ, Hays GL. Epidermolysis bullosa-review and report of a case. J Am Dent Assoc 1983;107:749–51 [DOI] [PubMed] [Google Scholar]
- 2.Fine JD, Johnson LB, Suchindran CM. The National Epidermolysis Bullosa Registry. J Invest Dermatol 1994;102:545–65 [DOI] [PubMed] [Google Scholar]
- 3.Gormley JW, Show CE. Epidermolysis bullosa and associated problems in oral surgical treatment. J Oral Surg 1976;34:45–52 [PubMed] [Google Scholar]
- 4.David JO. Fine inherited epidermolysis bullosa. Orphanet J Rare Dis 2010;5:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wright JT. Comprehensive dental care and general anesthetic management of hereditary epidermolysis bullosa. Oral Surg Oral Med Oral Pathol 1990;70:573–8 [DOI] [PubMed] [Google Scholar]
- 6.Hochberg MS, Varquez-Santiago IA, Sher M. Epidermolysis bullosa. A case report. Oral Surg Oral Med Oral Pathol 1993;75:54–7 [DOI] [PubMed] [Google Scholar]
- 7.Prabhu VR, Rekka P, Ramesh , et al. Dental and anesthetic management of a child with epidermolysis bullosa. J Indian Soc Pedod Prev Dent 2011;29:155–60 [DOI] [PubMed] [Google Scholar]
- 8.Stavropoulos F, Abramowicz S. Management of the oral surgery patient diagnosed with epidermolysis bullosa: report of 3 cases and review of the literature. J Oral Maxillofac Surg 2008;66:554–9 [DOI] [PubMed] [Google Scholar]
- 9.De Freitas AC, Ribeiro ZMM, De Oliveira MCT, et al. Clinical management of a case of epidermolysis bullosa. Rev Fac Odontol Ribeirao Preto 1986;23:71–8 [PubMed] [Google Scholar]
- 10.Siqueira MA, De Souza Silva J, Silva FW, et al. Dental treatment in a patient with epidermolysis bullosa. Spec Care Dentist 2008;28:92–5 [DOI] [PubMed] [Google Scholar]
- 11.Kostara A, Roberts GJ, Gelbier M. Dental maturity in children with dystrophic epidermolysis bullosa. Pediatr Dent 2000;22:385–8 [PubMed] [Google Scholar]
- 12.Herod J, Denyer J, Goldman A, et al. Epidermolysis bullosa in children: pathophysiology, anaesthesia and pain management. Paediatr Anaesth 2002;12:388–97 [DOI] [PubMed] [Google Scholar]
- 13.Wright JT, Fine JD, Johnson L. Hereditary epidermolysis bullosa: oral manifestations and dental management. Pediatr Dent 1993;15:242–8 [PubMed] [Google Scholar]
- 14.Wright JT. Epidermolysis bullosa: dental and aesthetic management of two cases. Oral Surg Oral Med Oral Pathol 1984;57:155–7 [DOI] [PubMed] [Google Scholar]


