Abstract
Actinomycosis is a rare, torpid, suppurative and chronic granulomatous infection caused by a Gram-positive organism that was initially thought to be a fungus. These organisms normally live as commensals in the human oral cavity, respiratory and digestive tracts, but become invasive when they gain access to the subcutaneous tissue through a musosal lesion, the triggering events being dental caries, dental manipulation and maxillofacial trauma. It is often misdiagnosed as it can mimic numerous infectious and non-infectious diseases. We describe an interesting case of cervical actinomycosis that was misdiagnosed as sebaceous cyst and precisely identified after histopathological examination of the tissue.
Background
Cervicofacial actinomycosis is a rare infectious disease caused by Gram-positive anaerobic and microaerophilic bacteria residing in the oral cavity.1 2 Diagnosis is difficult and definitive only after surgical excision of the cervicofacial mass. Use of special stains is often required to identify the causative organism and rule out the other differentials to prescribe appropriate treatment. We present an unusual case of cervicofacial actinomycosis that was misdiagnosed as sebaceous cyst and precisely identified after histopathological examination and use of modified Gram stain.
Case presentation
A 20-year-old woman presented with a 2-month history of a slowly growing painless swelling in the right cervical region, not associated with any discharge. She also denied history of fever, chills, weight loss and other constitutional symptoms as well as any history of tubercular infection or recent oromaxillofacial trauma or dental extraction. The patient was of low socioeconomic status and had bad oral hygiene. Clinically the patient's case was diagnosed as that of sebaceous cyst.
Investigations
A physical examination revealed a soft to firm non-tender, non-fluctuant and well-defined soft tissue swelling measuring 3×2 cm. Systemic examination was unremarkable and so were the haematological examination and imaging. The lesion was excised for aesthetic reasons and the tissue sent for examination. Histopathological evaluation revealed a central neutrophilic lobulated abscess that contained a large number of sulfur granules, characterised by round oval masses with basophilic appearance and a finely eosinophilic border (figure 1A,B). Histochemically, actinomycete filaments were stained deep bluish purple with the Brown and Brenn-modified Gram stain (figure 2A,B) and positively with the periodic acid-Schiff (PAS) stain but negatively with the Ziehl-Neelsen stain. The patient was hence diagnosed as cervicofacial actinomycosis.
Figure 1.
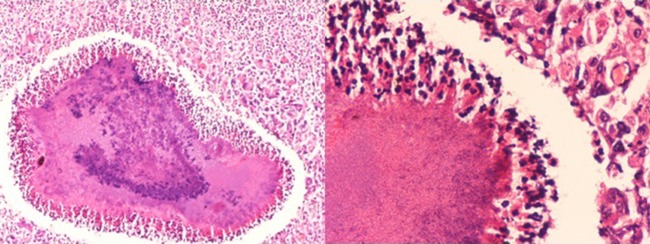
(A and B) Smear showing central neutrophilic lobulated abscess containing sulfur granules (H&E ×100 and ×400).
Figure 2.
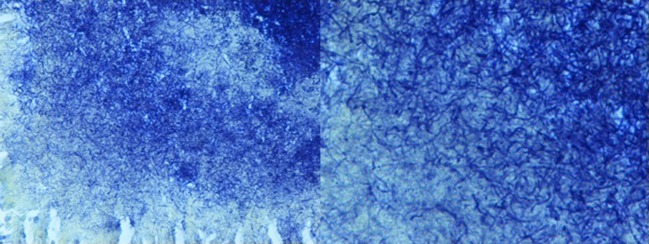
(A and B) Smear showing deep blue-coloured actinomycete filaments (Brown and Brenn modified Gram stain ×400 and ×1000).
Differential diagnosis
A very close differential diagnosis of actinomycosis is nocardiosis, but the granules in the latter consist of acid-fast branched bacilli. Botryomycosis may also have similar presentation but the granules in this case contained non-filamentous cocci.3
Treatment
The patient was started on high doses of penicillin for 4 weeks by the clinician.
Outcome and follow-up
This was followed by complete recovery and a follow-up which revealed no recurrence of the infection.
Discussion
Actinomycosis was first described in 1845 by Von Langebeck who thought it to be a fungus. It was the study done by Israel and Ponfick in 1891 in which they defined the anaerobic nature of actinomyces and isolated it in man. Waksman in 1960s established its Gram-positive nature. Human actinomycosis is a non-specific granulomatous chronic bacterial infection caused by Actinomyces israelii—a Gram-positive, non–acid-fast, anaerobic bacteria and a normal commensal flora of the oral cavity that cannot penetrate healthy tissue and requires mucosal breakdown as a pre-requisite for infection.4
In 1938, Cope classified actinomycosis infection into three distinct clinical forms: cervicofacial, pulmothoracic and abdominopelvic. Cervicofacial is the most common form although uncommon. The sites most commonly involved in this form include the submandibular space, cheek, parotid gland, teeth, tongue, nasal cavity, gingival and oral space, hypopharynx, medial aspect of aryepiglottic fold, parapharyngeal space, hyoid and the cartilage area of the thyroid, the frontal region, lymph nodes of the neck. Middle-aged adults are more commonly affected with a slight male predominance.4
The infection, most commonly presents as a chronic fluctuant mass, frequently located at the border of the mandible which progressively increases in size.5 The initial symptoms are often non-specific like pain, fever, swelling, erythema and oedema at the site of swelling. Sinus and tract formation is observed in 40% of the cases and this makes the diagnosis definite.6 It was the absence of this discharge that led to the misdiagnosis of the mass as sebaceous cyst in the present case.
Imaging techniques are usually non-productive as the radiological feature of the mass and the soft tissue involvement does not point to a distinct cause. Surgical excision of the mass followed by histopathological staining and special staining with modified Gram, Gomori methenamine silver and PAS of the tissue emains the only resolutive approach to make a definitive diagnosis.2 Through this case, we emphasise the importance of the modified Brown and Brenn Gram staining technique which is a special method used for differential staining of Gram-positive and Gram-negative bacteria. The tissue section in our case did not adsorb any stain with routine Gram stain, but the Actinomyces colonies stained blue with the Brown and Brenn stain.
A therapy with penicillin for at least 3 months is the mainstay of the treatment of actinomycosis. Alternatively, second line drugs like erythromycin, tetracycline may also be used in patients who are allergic to penicillin. Cephalosporins may also be used in the acute phase along with steroids to eliminate the residual inflammatory reaction.4 6
A very close differential diagnosis of actinomycosis is nocardiosis but the granules in the latter consist of acid-fast branched bacilli. The importance of this differential lies in the treatment of the two infections. Actinomyces is extremely sensitive to penicillin, and hence this becomes the treatment of choice for actinomycosis. Nocardia, on the other hand, is a relatively resistant organism responding mainly to sulfadiazines. Botryomycosis may also have similar presentation but the granules in this case contain non-filamentous cocci.3
To conclude, any soft tissue mass or swelling on the cervicofacial area should be investigated for cervicofacial actinomycosis and should be clearly differentiated from its counterpart nocardiosis in lieu of their varied response to a therapy.5
Learning points.
Human actinomycosis is an aspecific granulomatous chronic bacterial infection caused by Actinomyces israelii—a Gram-positive, non–acid-fast, anaerobic bacteria and a normal commensal flora of the oral cavity that cannot penetrate healthy tissue and requires mucosal breakdown as a prerequisite for infection.
Surgical excision of the mass followed by histopathological staining and special staining with modified Gram, Gomori methenamine silver and periodic acid-Schiff of the tissue remains the only resolutive approach to make a definitive diagnosis.
A very close differential diagnosis of actinomycosis is nocardiosis but the granules in the latter consist of acid-fast branched bacilli. Botryomycosis may also have similar presentation but the granules in this case contain non-filamentous cocci.
To conclude, any soft tissue mass or swelling on the cervicofacial area should be investigated for cervicofacial actinomycosis.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Bochev V, Angelova I, Tsankov N. Cervicofacial actinomycosis—report of two cases. Acta Dermatovenerol Alp Panonica Adriat 2003;12:105–8 [Google Scholar]
- 2.Mehta V, Balachandran C. Primary cutaneous actinomycosis on the chest wall. Dermatol Online J 2008;14:13. [PubMed] [Google Scholar]
- 3.Wee SH, Chang SN, Shim JY, et al. A case of primary cutaneous actinomycosis. J Dermatol (Tokyo) 2000;27:651–4 [DOI] [PubMed] [Google Scholar]
- 4.Lancella A, Abbate G, Foscolo AM, et al. Two unusual presentations of cervicofacial actinomycosis and review of the literature. Acta Otorhinolaryngol Ital 2008;28:89–93 [PMC free article] [PubMed] [Google Scholar]
- 5.Yılmaz Çiftdoğan D, Bayram N, Akalın T, et al. Actinomycosis in differential diagnosis of cervicofacial mass: a case report. J Pediatr Infect 2009;3:28–30 [Google Scholar]
- 6.Volante M, Contucci AM, Fantoni M, et al. Cervicofacial actinomycosis—still a difficult differential diagnosis. Acta Otorhinolaryngol Ital 2005;25:116–19 [PMC free article] [PubMed] [Google Scholar]


