Abstract
Granular cell tumour (GCT) is a rare, usually benign neoplasm that can mimic carcinoma on breast imaging. GCT can originate anywhere in the body but is most frequently found in the head and neck region, particularly in the tongue. Of the reported cases, 6% have occurred in the breast, most commonly in the upper inner quadrant. We report a case of GCT of the breast presenting as a spiculated mass infiltrating the greater thoracic muscle on breast screening mammogram.
Background
Abrikossoff1 first described granular cell tumour (GCT) in 1926 as ‘granular cell myoblastoma’ assuming it was of myogenic origin. Subsequently, immunohistochemical and ultrastructural features have proposed a perineural or Schwann cell origin. The neoplastic cells of the tumour typically express S100 and CD68 (KP-1).2 However, the exact histogenesis of GCT is still unknown.2
GCT of the breast is usually benign, although there have been reported malignant GCT cases.3
Case presentation
A 57-year-old woman attended a screening mammogram as part of the Breast Screening Programme. A 2 cm spiculated mass infiltrating the greater thoracic muscle was noted. Clinical examination was normal. The lesion was suspicious for malignancy on imaging Breast Imaging-Reporting and Data System (BIRADS) 5 (figures 1A,B and 2), and excision biopsy was undertaken, without prior FNA. Histological examination showed a GCT. A wide local excision of the left breast mass was performed without complications. Final pathology confirmed GCT (figures 3 and 4).
Figure 1.
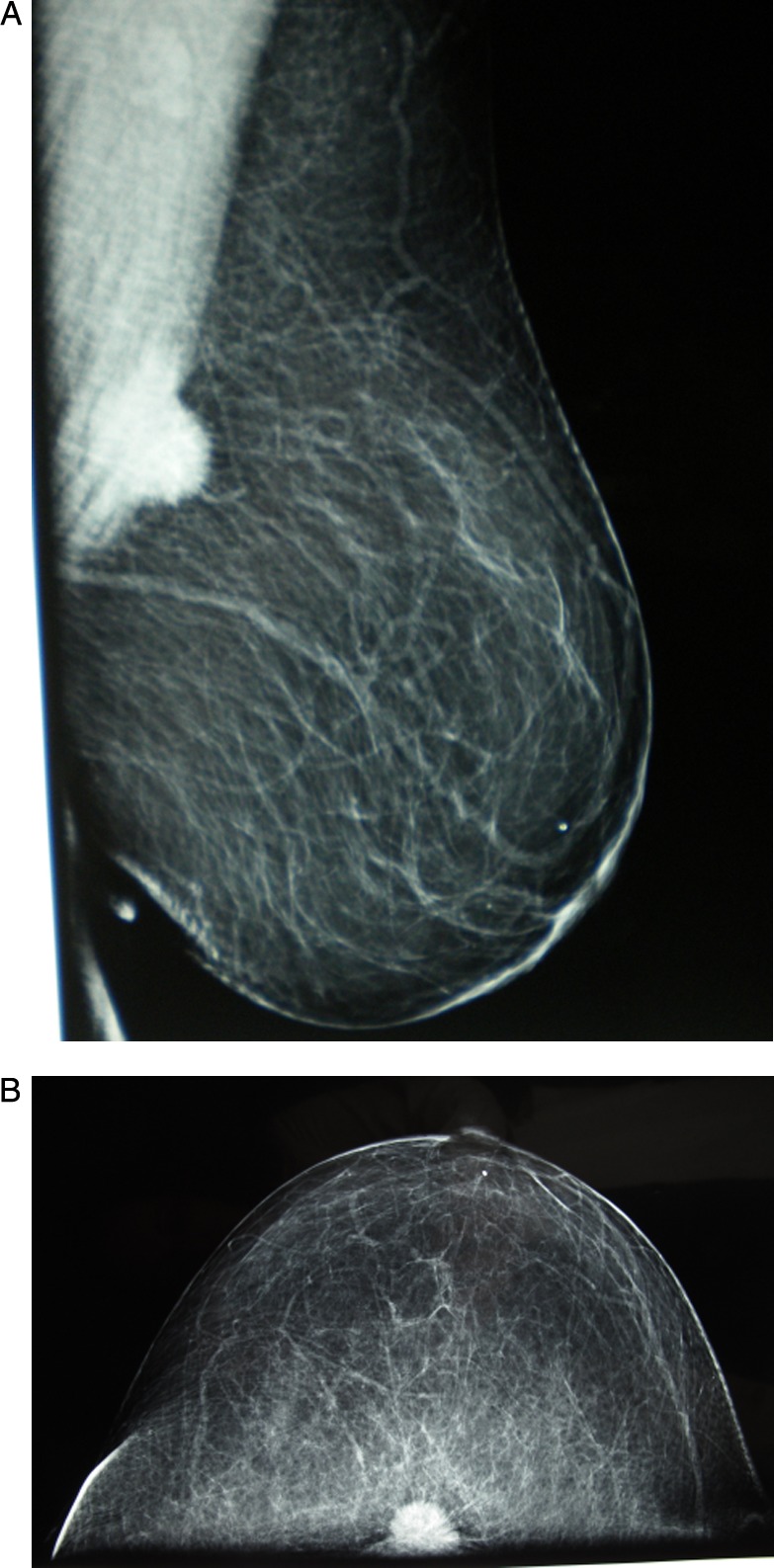
(A) Left mediolateral oblique view: spiculated mass 2 cm in diameter on the second hour of the left breast, infiltrating the greater thoracic muscle, Breast Imaging-Reporting and Data System (BIRADS) 5. (B) Craniocaudal view: spiculated mass 2 cm in diameter on the second hour of the left breast, BIRADS 5.
Figure 2.
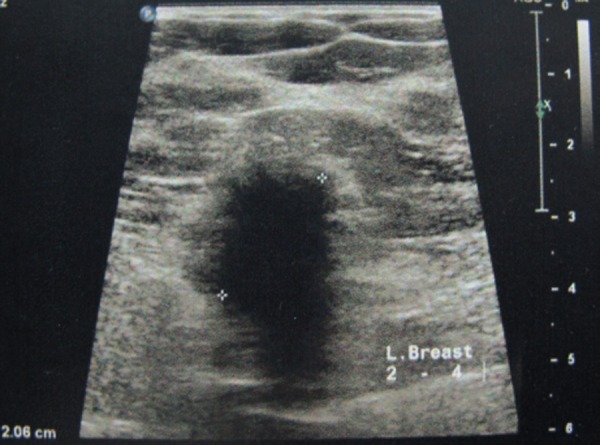
Breast ultrasound: hypoechoic spiculated mass on the second hour of the left breast. An acoustic shadow was present, but no significant vascularisation was detected.
Figure 3.
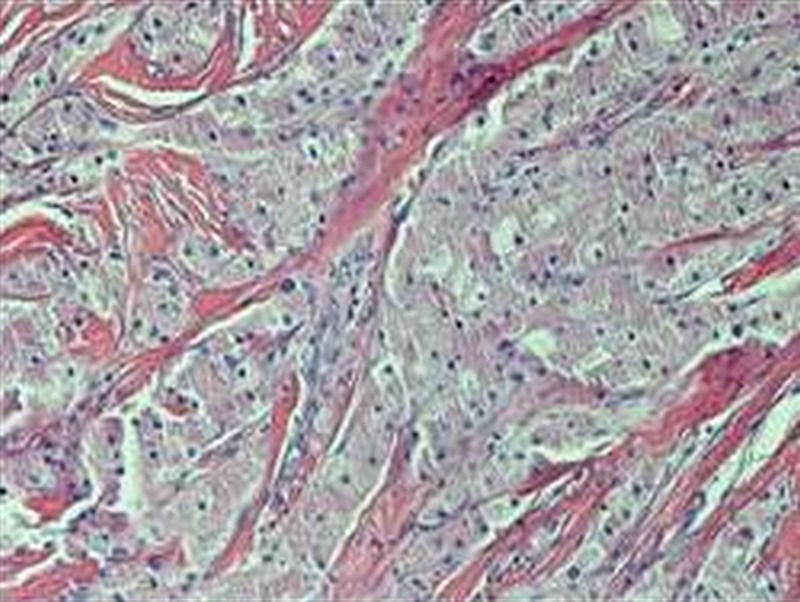
H&E ×200 solid nests of tumour cells with coarsely granular cytoplasm.
Figure 4.
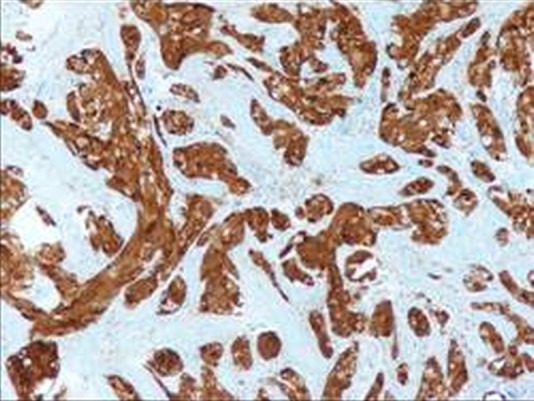
S100 positive. Immunoreactivity with S100 is important in confirming the diagnosis of granular cell tumour (GCT).
Differential diagnosis
GCT may present differential diagnostic difficulty since it may simulate carcinoma on mammography and ultrasound. Mammographically, it is difficult to distinguish from carcinoma, forming a typical stellate mass lacking calcifications.4 Ultrasound usually reveals a solid mass with posterior shadowing suggestive of carcinoma.4 5 Sonographically guided biopsy of the lesion is the diagnostic procedure of choice.4 6 The main striking histological element is the presence of abundant eosinophilic cytoplasm. The detection of S100 protein expression may be needed to support the diagnosis, especially on small biopsies, when there is marked pseudoepitheliomatous hyperplasia mimicking squamous cell carcinoma, or to distinguish GCTs from other neoplasms with abundant eosinophilic granular neoplasm.2
Treatment
Wide local excision is the treatment of choice for benign GCT.
Outcome and follow-up
She is in follow-up and doing well.
Discussion
Breast GCTs occur more commonly in premenopausal women with frequency approximately 1 in 1000 breast cancers.7 A slight preponderance in African-American women was reported.6–8 GCTs of the breast have also been described in men.9 In contrast to most other breast tumours, which occur predominantly in the upper outer quadrant, GCTs are most frequently found in the upper inner quadrant,6 corresponding to the cutaneous sensory territory of the supraclavicular nerve.6
GCT usually appears as a solitary unilateral painless lump. However, multiple lesions have been reported in 5, 4% to 17, 5% of cases.6–8
On mammography, GCT of the breast may present as round, circumscribed lesions as distinct densities, or as stellated masses difficult to distinguish from malignancy.4 5 On ultrasound it usually reveals as a solid mass with posterior shadowing.4 Radiographically, it is impossible to establish a definitive diagnosis of GCT of the breast without a biopsy.
Le et al2 and Adeniran et al6 proposed six histological criteria for distinction between benign and malignant GCTs. (1) Necrosis, (2) spindling, (3) vesicular nuclei with large nucleoli, (4) increased mitotic activity (>2 mitoses per 10 high power field at 200 magnification), (5) high nuclear/cytoplasmic ratio and (6) nuclear pleomorphism. These criteria classify GCT histologically into atypical (when two of these six criteria are present) and malignant (when three or more criteria are present).
Malignant GCTs are rare, but must be suspected when (1) pathologically enlarged lymph nodes are detected; (2) the tumour is greater than 5 cm; (3) there is a heterogenous signal intensity or rim enhancement on breast magnetic resonance imaging or (4) there is infiltration of the adjacent tissues.10 11
GCT must be distinguished from metastatic neoplasm in the breast that have oncocytic or clear cell features, such as renal carcinoma, malignant melanoma and alveolar soft part sarcoma.12
Learning points.
Clinically, most patients will present with a painless, firm, mobile nodule in the upper inner breast quadrant and are often initially diagnosed as having a fibroadenoma or carcinoma.12
Granular cell tumours of the breast are unlikely to be diagnosed correctly on initial examination unless biopsy and pathological results are obtained.12
The definitive diagnosis is based on biopsy and pathological results.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Abrikossoff A. Über myome, ausgehend von der quergestreiffen willkϋrlichen muskulatur. Virchows Arch Pathol Anat 1926;260:215–33 [Google Scholar]
- 2.Le BH, Boyer PJ, Lewis JE, et al. Granular cell tumor, immunohistochemical assessment of inhibin-alpha, protein gene product 9,5, S100 protein, CD68 and ki-67 proliferase index with clinical correction. Arch Pathol Lab Med 2004;128:771–5 [DOI] [PubMed] [Google Scholar]
- 3.Chetty R, Kalan MR. Malignant granular cell tumor of the breast. J Surg Oncol 1992;49:135–7 [DOI] [PubMed] [Google Scholar]
- 4.Yang WT, Edeiken-Monroe B, Sneige N, et al. Sonographic and mammographic appearances of granular cell tumors of the breast with pathological correlation. J Clin Ultrasound 2006;34:153–60 [DOI] [PubMed] [Google Scholar]
- 5.Vos LD, Tjon A, Vroegindweij D, et al. Granular cell tumor of the breast: mammographic and histologic correlation. Eur J Radiol 1994;19:56–9 [DOI] [PubMed] [Google Scholar]
- 6.Adeniran A, Al-Ahmadie H, Mahoney MC, et al. Granular cell tumor of the breast: a series of 17 cases and review of the literature. Breast J 2004;10:528–31 [DOI] [PubMed] [Google Scholar]
- 7.Kragel PJ, Fiorella RM, Kremer H. Tumoral fibrosis and lack of circumscription in granular cell tumor of the breast. South Med J 1995;88:1146–8 [DOI] [PubMed] [Google Scholar]
- 8.Lack EE, Worsham GF, Gallihan MD, et al. Granular cell tumor: a clinicopathologic study of 110 patients. J Surg Oncol 1980;13:301–16 [DOI] [PubMed] [Google Scholar]
- 9.Calo PG, Porcu C, Pollino V, et al. Granular cell tumor of the male breast. A case report. Minerva Chir 1998;53:1043–6 [PubMed] [Google Scholar]
- 10.Jardines L, Cheung L, Livolsi V, et al. Malignant granular cell tumors: report of a case and review of the literature. Surgery 1994;116:49–54 [PubMed] [Google Scholar]
- 11.Osanai T, Ishikawa A, Ogino T, et al. Contrast-enhanced magnetic resonance imaging of malignant granular cell tumor with pathological correlation: a case report. J Orthop Sci 2004;9:529–32 [DOI] [PubMed] [Google Scholar]
- 12.Willen R, Willen H, Balldin G, et al. Granular cell tumor of the mammary gland simulating malignancy. Virchows Arch 1984;403:391–400 [DOI] [PubMed] [Google Scholar]


