Abstract
Stereotactic body radiation therapy (SBRT) for early stage lung cancer has made significant strides as an alternative to surgery.1 We present two cases of non-small cell lung cancer treated with SBRT and then followed serially with imaging in which suspicion of recurrence led to biopsies.
Background
Although treatment success is high with stereotactic body radiation therapy (SBRT), follow-up to detect early local recurrence is challenging. Inflammatory changes with SBRT leading to radiographic pneumonitis and fibrosis confound differentiation of tumour response versus normal tissue injury.
Case presentation
Case 1
A 79-year old man presented with a fluorodeoxyglucose (FDG)-avid 2.1×1.7 cm (standard uptake value (SUV)max 3.1) stage I non-small cell lung cancer (NSCLC), adenocarcinoma type, involving the right middle lobe (RML). He received 54 Gy in three fractions planned with a pre-treatment PET-CT (figure 1). A routine 2-month post-treatment PET-CT revealed interval decrease in size and FDG avidity of the right upper lobe (RUL) tumour (SUVmax 2.1). CT scans performed every 3 months thereafter showed evolving radiation changes. A repeat PET-CT performed at 14 months demonstrated interval increase in FDG activity in the RML mass (SUVmax 3.0) with increased central density on CT concerning for recurrence as well as a new intensely FDG-avid nodule (SUVmax 3.8) in the left lower lobe (LLL) (figure 2). CT-guided needle biopsy of the LLL nodule showed reactive hyperplasia of alveolar lining cells, negative for malignancy. PET-directed biopsy of the RML confirmed reactive atypical pneumocytes, interstitial elastofibrosis and vascular thickening, all consistent with benign radiation-induced changes (figure 3). The patient continues to do well clinically 30 months after SBRT. The most recent CT scan revealed a post-radiation stable soft tissue mass without evidence of local growth (figure 2).
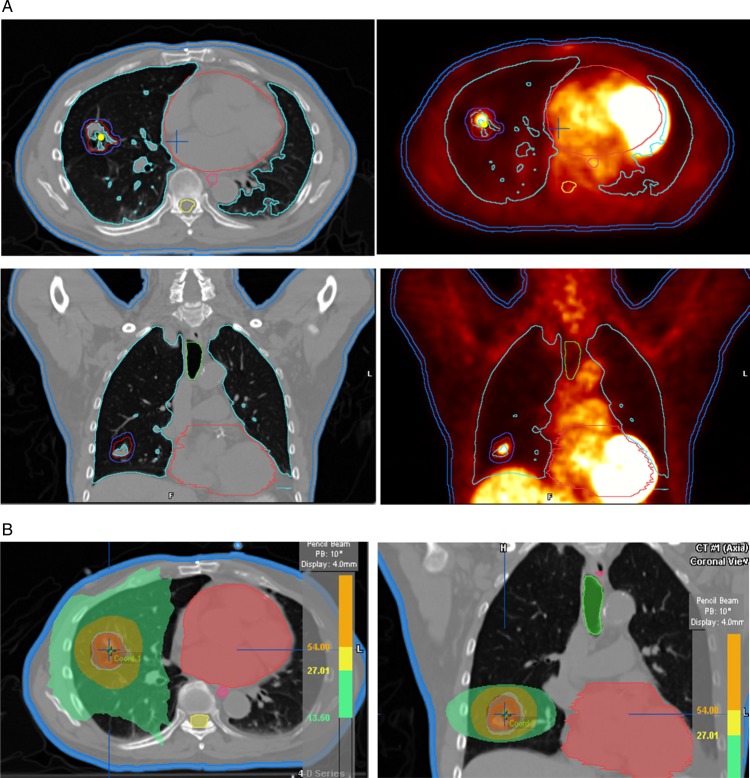
Figure 1.
(A) Case 1 pre-treatment PET-CT: (left) Axial and coronal CT and (right) fused PET-CT for a right middle lobe non-small cell lung cancer. The red line is the internal target volume, and the blue line is the planning target volume. (B) Case 1 treatment plan: (left) isodose colour wash in axial and (right) coronal planes.
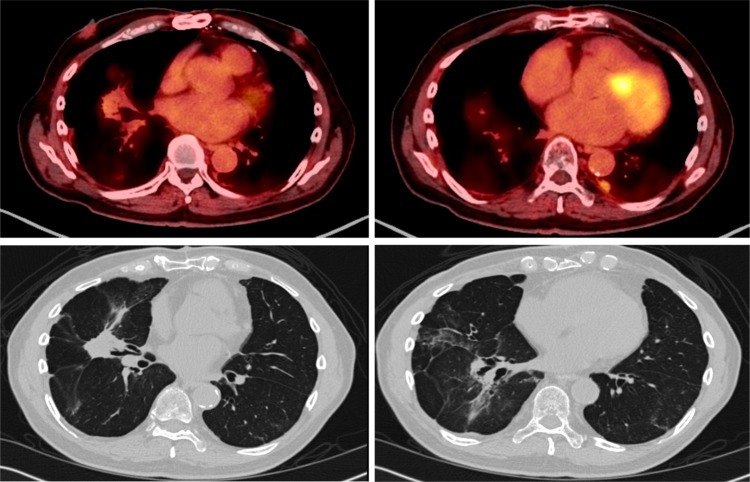
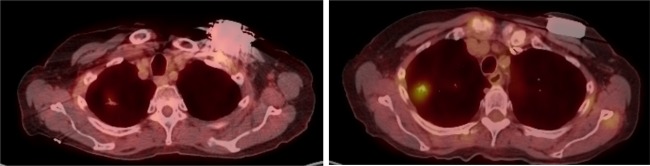
Figure 2.
Case 1 post-stereotactic body radiation therapy PET-CT: (top left) axial fused PET-CT at 14 months showing a concerning focus of FDG uptake; (top right) axial fused PET-CT at 14 months showing a new FDG-avid left lower lobe (LLL) nodule; (bottom left) axial CT at 30 months showing a stable right middle lobe soft tissue mass; (bottom right) axial CT at 30 months showing resolution of the LLL nodule.
Figure 3.
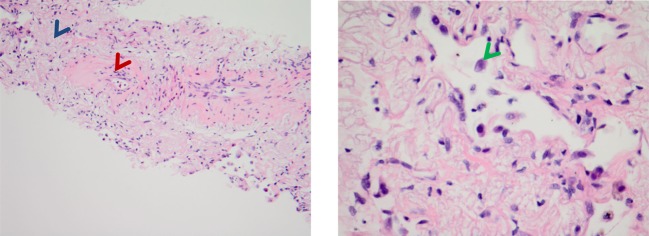
Case 1 pathology—stereotactic body radiation therapy site: (left) H&E stain showing hyalinisation of vessels (red arrow) and reactive interstitial fibrosis (blue arrow); (right) H&E stain showing peribronchial reactive atypical pneumocytes (green arrow).
Case 2
A 73-year old former smoker presented with a growing RUL tumour in the setting of biopsy proven stage IV (adenocarcinoma) NSCLC. She had received systemic chemotherapy with good response at all sites of disease (multiple pulmonary nodules, left 8th rib) with the exception of the RUL primary that increased from 1.4×1.1 to 1.9×1.3 cm. Based on multidisciplinary discussion, and given her excellent performance status, the patient was offered and treated with SBRT to the RUL tumour to a dose of 54 Gy in three fractions (figure 4). Routine 2-month post-treatment PET-CT revealed a decrease in the size, FDG avidity (SUVmax 1.4) and interval cavitation of the treated tumour to 1.8×0.8 cm consistent with a favourable response. A 5-month post-SBRT PET-CT was performed by the medical oncologist to evaluate metastatic disease burden and revealed interval development of an intensely FDG-avid mass-like lesion (SUVmax 4.1) in the field of prior SBRT concerning for local progression (figure 5). The patient was referred for consideration of re-irradiation. A CT-guided biopsy of the mass was performed to document recurrence. Pathology revealed lung tissue with atypical pneumocytes, consistent with reactive changes from radiation without evidence for malignancy. The most recent CT scan 13 months after SBRT showed continued evolving consolidation within the RUL, stable in size and without progressive distant disease (figure 6).
Figure 4.
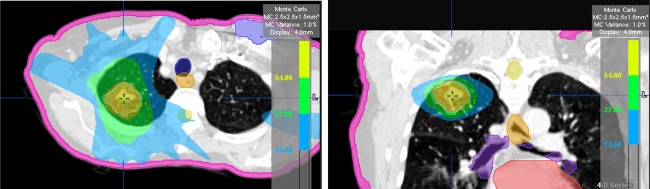
Case 2 treatment plan.
Figure 5.
Case 2 post-stereotactic body radiation therapy (SBRT) PET-CTs: (left) PET-CT at 2 months post-SBRT showing decreased FDG avidity and size; (right) PET-CT at 5 months post-SBRT showing increased FDG avidity.
Figure 6.
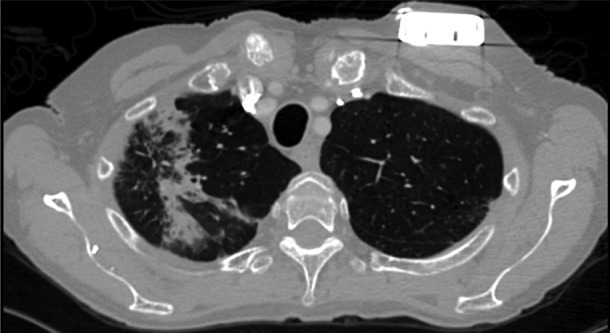
Case 2 post-stereotactic body radiation therapy (SBRT) CT: axial CT at 13 months post-SBRT showing radiographic radiation-induced injury.
Discussion
Post-lung SBRT imaging surveillance for tumour recurrence remains a clinical dilemma. SBRT is effective for localised NSCLC, however the nature of the treatment induces injury and inflammation that is challenging to differentiate from tumour recurrence. These two cases illustrate the limitation of PET-CT imaging at 5 and 14 months post-SBRT, both of which were suspicious for recurrence. Biopsy of the PET-positive areas revealed only evidence of lung injury. Active research is ongoing to determine which imaging modalities and at what interval are best to detect SBRT local failures. In a cohort of 128 patients, researchers at MD Anderson concluded that beyond 6 months, a maximum SUV greater than 5 on PET should prompt a biopsy to rule out recurrence.2 However, the positive predictive value based on this cut-off value was only 50%. Others have characterised changes in FDG uptake between 0 and 24 months after SBRT, revealing that up to 30% of treated thoracic tumours retained moderate to intense FDG uptake.3 4 These cases are consistent with findings that abnormal increased FDG uptake following lung SBRT may not be due to treatment failure, but rather treatment-induced normal tissue response. Our cases are consistent with the finding that post-SBRT abnormal SUVmax <5, despite an increase from a post-SBRT nadir, may likely represent false-positivity.
CT-based follow-up to detect recurrence is also difficult when nearly all treated patients have some radiographic abnormality.5 Acute phase changes are characterised by ground-glass opacities and consolidation, while late phase changes manifest as volume loss, consolidation and traction bronchiectasis.6 Trovo et al found that the majority of patients had no evidence of radiographic lung injury up to 6 weeks after SBRT; however, most of the patients had patchy and diffuse consolidation 2–6 months after SBRT, with up to 28% characterised as mass-like at 13 months.7 Matsuo et al found mass-like consolidation in 27 of 40 lung tumours treated with thoracic SBRT at a median time of 5 months.8 With longer follow-up, it was demonstrated that 24 of the 27 mass-like consolidations were due to radiation-induced lung injury, while three were due to local recurrence. Lastly, alertness to kinetic changes such as three consecutive soft-tissue volume increases 12 months after SBRT may be a promising approach to improve the accuracy of detecting recurrences.9
Learning points.
The role of stereotactic body radiation therapy (SBRT) for localised lung cancer continues to expand due to excellent results in medically inoperable patients.
The ongoing multi-centre randomised study (RTOG 1021) compares sublobar resection with SBRT in operable but high risk patients with stage I non-small cell lung cancer; as these are potentially healthier and younger patients identifying early failures of SBRT is important in order to offer timely definitive salvage surgery.
For an individual patient with radiographic suspicion of local recurrence and where salvage therapies such as re-irradiation, thermo/cryo ablation or surgery are considered, a biopsy is recommended to minimise futile retreatment.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Timmerman R, Paulus R, Galvin J, et al. Stereotactic body radiation therapy for inoperable early stage lung cancer. JAMA 2010;303:1070–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhang X, Liu H, Balter P, et al. Positron emission tomography for assessing local failure after stereotactic body radiotherapy for non-small-cell lung cancer. Int J Radiat Oncol Biol Phys 2012;83:1558–65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Matsuo Y, Nakamoto Y, Nagata Y, et al. Characterization of FDG-PET images after stereotactic body radiation therapy for lung cancer. Radiother Oncol 2010;97:200–4 [DOI] [PubMed] [Google Scholar]
- 4.Ishimori T, Saga T, Nagata Y, et al. 18F-FDG and 11C-methionine PET for evaluation of treatment response of lung cancer after stereotactic radiotherapy. Ann Nucl Med 2004;18:669–74 [DOI] [PubMed] [Google Scholar]
- 5.Dahele M, Palma D, Lagerwaard F, et al. Radiological changes after stereotactic radiotherapy for stage I lung cancer. J Thorac Oncol 2011;6:1221–8 [DOI] [PubMed] [Google Scholar]
- 6.Larici AR, del Ciello A, Maggi F, et al. Lung abnormalities at multimodality imaging after radiation therapy for non-small cell lung cancer. Radiographics 2011;31:771–89 [DOI] [PubMed] [Google Scholar]
- 7.Trovo M, Linda A, El Naqa I, et al. Early and late lung radiographic injury following stereotactic body radiation therapy (SBRT). Lung Cancer 2010;69:77–85 [DOI] [PubMed] [Google Scholar]
- 8.Matsuo Y, Nagata Y, Mizowaki T, et al. Evaluation of mass-like consolidation after stereotactic body radiation therapy for lung tumors. Int J Clin Oncol 2007; 12:356–62 [DOI] [PubMed] [Google Scholar]
- 9.Dunlap NE, Yang W, McIntosh A, et al. Computed tomography-based anatomic assessment overestimates local tumor recurrence in patients with mass-like consolidation after stereotactic body radiotherapy for early-stage non-small cell lung cancer. Int J Radiat Oncol Biol Phys 2012;84:1071–7 [DOI] [PubMed] [Google Scholar]