Abstract
A 17-year-old boy reported for evaluation of two episodes of massive haemoptysis. His clinical examination was unremarkable and investigations (haemogram, coagulogram, serological tests for connective tissue disorders) were normal. A 64-slice CT angiography revealed a saccular aneurysm of 3.8×3.7×3.3 cm arising from the right lower lobe pulmonary artery which was confirmed by cardiac catheterisation. The aneurysm was successfully blocked with a 16–14 Amplatzer duct occluder. A repeat CT angiogram performed after 15 days revealed the device in situ obliterating the aneurysm. Pulmonary artery aneurysm is an extremely rare cause of massive haemoptysis and indicates imminent rupture of the aneurysm which can be rapidly fatal. This case highlights the importance of using an innovative endovascular technique for treatment of a rare cause of haemoptysis.
Background
Pulmonary artery aneurysms are very rare and have variable aetiology which include infections (fungal, tuberculosis, syphilitic or bacterial), vasculitis (Behcet disease), chronic pulmonary embolism and trauma during cardiac catheterisation.1–4 They are also associated with structural cardiac abnormalities like patent ductus arteriosus (PDA), atrial septal defect, ventricular septal defect, tetralogy of Fallot, pulmonary valve stenosis, pulmonary valve regurgitation and absent pulmonary valve. In the past, surgical techniques namely aneurysmectomy, lobectomy or dacron graft replacement were the only treatment options available.5 Endovascular techniques using coil, glue or balloon embolisation6 7 stent graft placement8 or vascular closure device9 are less invasive and cause minimal damage to the normal pulmonary parenchyma.
Case presentation
A 17-year-old boy was referred to the hospital for an evaluation of two episodes of massive haemoptysis. The patient had no associated history of fever, weight loss or chronic cough. There was no history of tuberculosis or vasculitis in the patient or in any of the family members. Clinical examination at the time of admission revealed him to be haemodynamically stable with an unremarkable general and systemic examination.
Investigations
Routine biochemical and haematological investigations were normal. Coagulation profile and the serological tests for connective tissue disorders and vasculitis were negative. Posteroanterior chest radiograph revealed ill-defined spherical non-homogenous opacity in the right upper zone (figure 1), there was no other parenchymal abnormality noted. Brochoscopy was normal and bronchoalveolar lavage for mycobacteria and fungi was negative. Ultrasound abdomen and two-dimensional echocardiography did not reveal any abnormality. Sixty-four slice CT angiography done using non-ionic contrast revealed a saccular aneurysm of 3.8×3.7×3.3 cm arising from the right lower lobe pulmonary artery (figure 2). This aneurysm had a short neck with a wide ostium measuring 1.3 cm.
Figure 1.

Posteroanterior chest radiograph showing ill-defined spherical non-homogenous opacity in the right upper zone.
Figure 2.

64-Slice CT scan demonstrating the aneurysm of the descending branch of right pulmonary artery.
Differential diagnosis
The differential diagnosis of haemoptysis includes a wide spectrum of infectious, autoimmune, vascular and neoplastic diseases as well as chest trauma and systemic coagulopathy. Pulmonary aneurysm is secondary to infections (commonly right-sided endocarditis), vasculitis, chronic pulmonary embolism and trauma. It may also be noted in association with structural cardiac abnormalities.
Treatment
Cardiac catheterisation was done for further characterisation of the aneurysm. Selective injections of the right lower lobe pulmonary artery using the Judkins right coronary catheter demonstrated the aneurysm (figure 3). In view of the thin walls of the aneurysm and its large size it was decided not to place multiple coils as the risk of rupture was considered too high. An Amplatzer PDA occluder was considered appropriate, as it would not only hold on to the aneurysm sac but also block the feeder vessel. A 6 F right coronary diagnostic was used to enter the right pulmonary artery through which a 0.035 inch exchange wire (Emerald, Cordis, USA) was advanced into the aneurysm. An 8 F Amplatzer PDA delivery sheath (AGA medical Corp, USA) was advanced over the wire and the dilator and wire were removed. A 16–14 Amplatzer duct occluder (AGA medical Corp) was then deployed into the sac (figure 4). Postdeployment selective angiogram revealed minimal flow across the aneurysm neck with stasis of contrast in the aneurysm sac, suggesting successful embolisation. There were no periprocedural complications and the patient was discharged after 48 h.
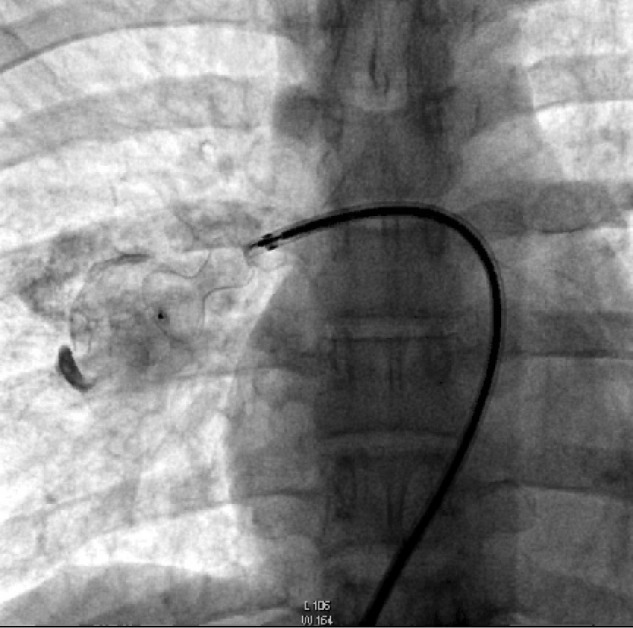
Figure 3.

Selective right pulmonary artery angiogram done using the Judkins right catheter demonstrating the aneurysm.
Figure 4.
A 16-14 Amplatzer duct occluder (AGA Medical Corp, USA) deployed into the aneurysm sac.
Outcome and follow-up
A repeat CT angiogram was done 15 days after the device closure of the aneurysm revealed the device in situ along with obliteration of the aneurysm sac (figure 5).
Figure 5.

A 64-slice CT scan done 2 weeks postprocedure showing duct occluder device in situ along with obliteration of the aneurysm.
Discussion
Pulmonary artery aneurysms are very rare and account for <1% of the intrathoracic aneurysms. Aetiology is variable and they most often follow right-sided infective endocarditis with recurrent pulmonary artery embolisation; however, as in our case the aetiology is not easy to establish. Pulmonary aneurysm may be an incidental finding as with the availability of the multidetector CT angiography a higher number of these aneurysms are being diagnosed.10 Presenting symptoms include dyspnoea, chest pain, haemoptysis, pericardial tamponade or sudden death.1 2 Haemoptysis as was noted in the present case indicates imminent rupture of the aneurysm which can be rapidly fatal.11 The treatment options of such an aneurysm could be either medical, surgical or catheter embolisation5–9 Large aneurysms (high risk of rupture) and those arising from the main pulmonary trunk require surgical intervention.1 2 While those arising from the peripheral branches can be dealt with using embolotherapy using coils, vascular plug or stent grafts.5–9 The choice of embolic agents or covered stents is dictated by the morphology of the lesion (number, location and width of neck). In our case, the aneurysm was solitary and had a short neck, making device closure an attractive and a safer option. Employment of the duct occluder is an easy process which allows targeted precise delivery of the device within the artery. PDA closure device enabled treatment of the aneurysm without patient having to face the morbidity of the surgical procedure. The patient could be discharged from the hospital in short duration with no immediate procedure-related complications. This case highlights the importance of thinking out of the box while treating life-threatening emergencies along with use of newer prosthetic devices for the treatment of such conditions.
Learning points.
Pulmonary artery aneurysm is an extremely rare entity and accounts for <1% of the intrathoracic aneurysms.
It has a variable aetiology which includes infections, structural cardiac abnormalities, vasculitis, chronic pulmonary embolism and trauma.
Pulmonary aneurysm may be an incidental finding, common presentations are dyspnoea, chest pain, haemoptysis, pericardial tamponade or sudden death.
Haemoptysis is due to dissection or imminent rupture of pulmonary artery aneurysm which is usually fatal.
Endovascular treatment is less invasive and causes little trauma to the intimal damage to surrounding normal lung parenchyma.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Lopez-Candales A, Kleiger RE, Aleman-Gomez J, et al. Pulmonary artery aneurysm: review and case report. Clin Cardiol 1995;18:738–40 [DOI] [PubMed] [Google Scholar]
- 2.Karkoulias K, Lykouras D, Nanopoulou M, et al. An unexpected pulmonary arterial aneurysm in a COPD patient. Acta Clin Belg 2011;66:379–80 [DOI] [PubMed] [Google Scholar]
- 3.Lee R, Son JS, Park YM. A case of left main pulmonary artery aneurysm associated with valvular pulmonary stenosis in a child. Pediatr Cardiol 2011;32:1055–6 [DOI] [PubMed] [Google Scholar]
- 4.Goda M, Budts W, Troost E, et al. Bicuspid pulmonary valve with atrial septal defect leading to pulmonary aneurysm. Ann Thorac Surg 2012;93:1706–8 [DOI] [PubMed] [Google Scholar]
- 5.Vistarini N, Aubert S, Gandjbakhch I, et al. Surgical treatment of a pulmonary artery aneurysm. Eur J Cardiothorac Surg 2007;31:1139–41 [DOI] [PubMed] [Google Scholar]
- 6.Liddell RP, Patel S, Neuwirth M, et al. Transcatheter coil embolization of large pulmonary artery pseudoaneurysms in a child. J. Vasc Interv Radiol 2003;14:923–7 [DOI] [PubMed] [Google Scholar]
- 7.Aoshima H, Mae M, Ikeda T, et al. Peripheral pulmonary artery aneurysm treated with embolization. Kyobu Geka 2012;65:890–3 [PubMed] [Google Scholar]
- 8.Hannan RL, Miyaji K, Burke RP, et al. Endovascular stent graft treatment of a pulmonary artery pseudoaneurysm. Ann Thorac Surg 2001;71:727–9 [DOI] [PubMed] [Google Scholar]
- 9.Jagia P, Sharma S, Juneja R, et al. Transcatheter treatment of pulmonary artery pseudoaneurysm using a PDA closure device. Diagn Interv Radiol 2011;17:92–4 [DOI] [PubMed] [Google Scholar]
- 10.Khalil A, Parrot A, Nedelcu C, et al. Severe hemoptysis of pulmonary arterial origin signs and role of multidetector row CT angiography. CHEST 2008;133:212–19 [DOI] [PubMed] [Google Scholar]
- 11.Haridas KK, Neeraakal GM, Moorthy S, et al. Ruptured idiopathic pulmonary artery aneurysm: unusual case of hemothorax treated by selective embolization. Indian Heart J 2001;53:769–72 [PubMed] [Google Scholar]


