Abstract
A 27-year-old woman with a history of depression and previous overdose presented within 60 min of ingestion of 50 g of caffeine powder. Initially alert but hypotensive and tachycardic, the patient developed a broad complex tachycardia followed by a seizure and multiple ventricular fibrillation (VF) arrests. Following multiple defibrillations for VF, eight cycles of cardiopulmonary resuscitation and treatment with amiodarone, lidocaine, magnesium and potassium supplementation, the patient went to the intensive care unit (ICU). While there, the patient had further VF and required haemofiltration for a profound metabolic acidaemia with cardiac rhythm instability. She developed a postcardiac arrest systemic inflammatory response syndrome with episodes of acute pulmonary oedema, profound vasoplegia, hypothermia and coagulopathy. After 5 days in the ICU, the patient was stable enough to be transferred to the ward, with a persistent sinus tachycardia, and was discharged 3 days later with cardiology and psychiatry follow-up.
Background
Survival of a massive overdose of caffeine is rare with only one other reported survival of 50 g caffeine ingestion; hence, detailing the natural history and successful management of such a case is a useful addition to the medical literature. This case illustrates the life-threatening consequences of severe caffeine poisoning. It highlights the typical symptoms at presentation and the effective management of a life-threatening dose of caffeine.
Case presentation
A 27-year-old woman with a history of depression but no other significant medical, social or family history attempted suicide by ingesting 50 g of caffeine powder. When attended by paramedics, the history of caffeine overdose was obtained. Her initial observations were as follows: the patient appeared unwell and sweaty, Glasgow Coma Scale 15/15, respiratory rate 20 with normal depth, oxygen saturations 100% on air, pulse 179 bpm, blood pressure (BP) 100/51, blood sugar 7.4, temperature 35.6°C. The patient arrived in the accident and emergency department (A&E) within an hour of ingestion of the caffeine powder. Soon after arrival, the patient had a brief seizure followed by a ventricular fibrillation (VF) arrest requiring cardiopulmonary resuscitation (CPR) and defibrillation to return to spontaneous circulation.
Investigations
The initial ECG showed a broad complex tachycardia, a ventricular alternans rhythm (figure 1).
Figure 1.
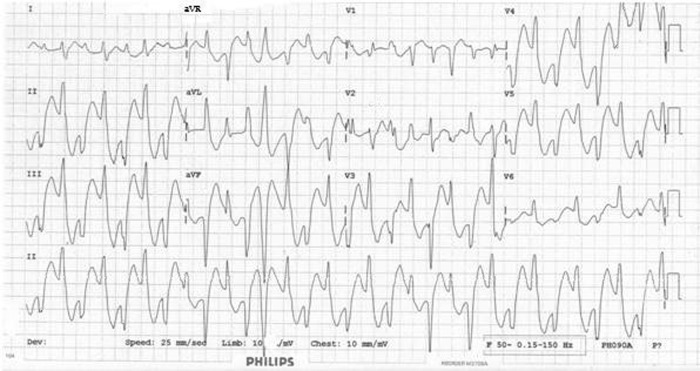
Broad complex tachycardia, constant R–R interval with alternans of the QRS axis and morphology.
The initial cardiac arrest arterial blood gas (ABG) showed: pH 7.05, pCO2 5.68, pO2 6.73, K+ 2.8, lactate 11.3, base excess 16.6 and bicarbonate 10.9.
Initial venous blood results: Na+ 149 mmol/l, K+ 4.4 mmol/l, Mg2+ 1.24 mmol/l, bicarbonate 8 mmol/l, urea 4.0 mmol/l, creatine 86μmol/l, C reactive protein <4 mg/l, glucose 11.9 mmol/l, bilirubin 6 μmol/l, alanine transaminase 75 u/l, alkaline phosphatase 76 u/l, albumin 47 g/l, haemoglobin 14.5 g/dl, mean cell volume 93.6 fl, white cell count 21.3×109/l, and platelets 409×109/l.
An initial toxicology screen for salicylates and paracetamol was ordered: salicylate, not detected; paracetamol, not detected.
Unfortunately, no serum caffeine concentration sample was obtained.
Differential diagnosis
The paramedics obtained a history of caffeine powder overdose from the patient. She denied any other substance use and alcohol ingestion with the overdose.
The differential diagnosis for a patient presenting with tachycardia, hypotension and metabolic acidosis with a raised lactate would include sepsis, diabetic ketoacidosis, mesenteric ischaemia or any other source of significant ischaemia, hypovolaemia, for example, from haemorrhage leading to organ hypoperfusion, a cocaine, amphetamine or tricyclic antidepressant overdose. Given the fact that the patient was female and of childbearing age, a ruptured ectopic pregnancy would need to be considered.
Treatment
The patient had five further VF arrests, in A&E and then in the intensive care unit (ICU), over the following 3 h, with 8 cycles of CPR in total and multiple defibrillations. Amiodarone 300 mg was used initially in an attempt to stabilise the cardiac rhythm but was ineffective. Given the patient's critical condition, and under cardiology specialist's advice, a further membrane-stabilising agent was used in 90 mg of 1% intravenous lidocaine. Sodium bicarbonate could also have been used in this context to help stabilise the ventricular arrhythmia secondary to caffeine overdose.
Potassium was replaced intravenously and a magnesium infusion started on the advice of the toxicology department.
The patient had no further VF 4 h after admission; however, while intubated and ventilated in the ICU, there were multiple complications of the overdose and cardiac arrest. Hypothermic at 31°C, the patient was rewarmed slowly. A central line was placed for continuous venovenous haemodiafiltration due to the profound metabolic acidaemia and rhythm instability. The patient's BP was persistently low with a systolic in the 80s, and poorly responsive to noradrenaline infusion; hence, terlipressin was used with greater success. While in the ICU, the patient had a high oxygen requirement and a few episodes of acute pulmonary oedema. This was thought to be a postcardiac arrest systemic inflammatory response syndrome. Such was the respiratory instability that transfer to an extracorporeal membrane oxygenation centre was considered. The ECG showed sinus tachycardia with episodes of ventricular bigeminy and frequent ventricular ectopics.
Outcome and follow-up
One day after admission to the ICU, the patient's condition had stabilised with an ABG on FiO2 0.5 showing: pH 7.32, pO2 8.4, pCO2 5.7, base excess −3.3, bicarbonate 21.3, and lactate 3.7.
On the following day, the patient was extubated successfully. By now, the ventricular ectopics had settled, but the patient had a persistent sinus tachycardia (figure 2). With a low-grade fever, worsening hypoxia and bibasal consolidation on a chest x-ray, intravenous tazocin was started for a hospital acquired pneumonia.
Figure 2.
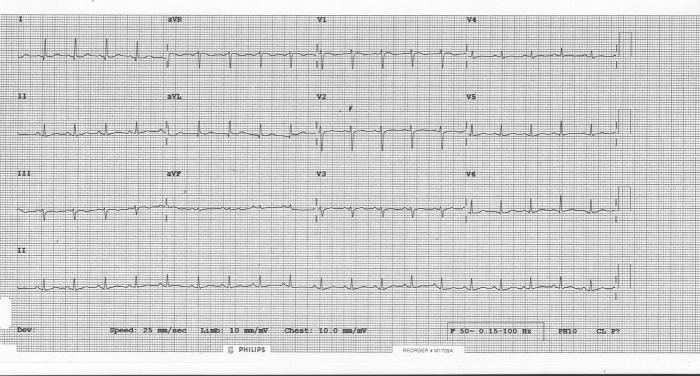
Sinus tachycardia, normal axis, normal QTc.
Her stay in the ward was uneventful and she was discharged 3 days later with psychiatry and cardiology follow-up. The patient has remained well and was discharged from the clinic 8 months postevent.
Discussion
Caffeine is a naturally occurring substance commonly used as a stimulant, taken either as part of a drink, for example, coffee, tea or energy drink or as a tablet. It is a methylxanthine mediating its effects through adenosine receptor antagonism at a moderate dose, phosphodiesterase inhibition at a high dose and direct intracellular calcium release at a very high dose.1 The overall effect of caffeine is linked to the dose of caffeine ranging from a negative inotropic and chronotropic effect at low dose to a positive inotropic and chronotropic effect at high dose to the direct release of calcium from the sarcoplasmic reticulum mediating significant arrhythmogenic effects at a very high dose. Other mechanisms for arrhythmia are most likely mediated through increased catecholamine release, stimulating β1 receptors, thus having positive inotropic and chronotropic effects, as well as phosphodiesterase inhibition, which increases the availability of cyclic adenosine monophosphate, thereby augmenting the sympathetic mediated effects. There is also thought to be a block of the antiarrhythmic properties of cardiac adenosine A2 receptors by caffeine.2
Common symptoms of overdose have previously been documented in the literature. They include nausea, vomiting, restlessness,3 altered mental state, anxiety, diaphoresis,4 dizziness5 and palpitations. Less commonly documented are muscle twitching, opisthotonus, myoclonic jerks and seizures.6
Initially, observations commonly reveal tachycardia, normotension or hypertension followed by hypotension and fever. Initial blood tests show little abnormality but may show hypokalaemia, hyponatraemia and metabolic acidosis.1 Severe overdose often leads to dysrhythmia including bradycardia, atrioventricular block, supraventricular tachycardia, ventricular tachycardia and VF. Perfusing rhythms may then deteriorate to circulatory collapse and cardiac arrest.1 6 Dysrhythmia has been treated in a variety of ways including esmolol alone,5 procainamide plus propranolol with electrolyte correction6 and a combination of lidocaine, phenylephrine and haemodialysis.4 In the event of cardiac arrest precipitated by dysrhythmia, return of spontaneous circulation is often followed by further arrest as seen in our case. Thus, in addition to antidysrhythmic medication, haemodialysis and inotropic support have been used successfully to remove caffeine from the circulation, maintain adequate organ perfusion and reduce rhythm instability.1 2 5 6
Holstege et al encountered a scenario similar to that of our patient's following a similarly massive caffeine overdose of 50 g. They similarly used amiodarone, lidocaine and electrolyte correction initially with little success. However, following haemodialysis and inotropic support with vasopressin, the patient stabilised with regard to cardiac rhythm. Our patient was stabilised following CVVHDF and terlipressin. This adds weight to the use of haemodialysis and inotropes in massive caffeine overdose. In this case, terlipressin was used. To our knowledge, this is the first reported use of terlipressin in caffeine overdose.
Apart from dysrhythmia, rhabdomyolysis and myocardial infarction have both been documented in the literature.3 7 Neither of these outcomes was documented in the case of our patient. Her urea and electrolytes remained stable, and she had a mild troponin and creatine kinase rise, which was most likely secondary to her cardiac arrest and subsequent resuscitation. A stress echocardiogram performed in an outpatient setting due to chest pain and non-specific T-wave changes showed normal left ventricular size and systolic function, no regional wall motion abnormality and no inducible ischaemia. The right heart size and function were normal.
Learning points.
Caffeine overdose can be life-threatening.
Arrhythmia is a common complication that needs prompt management to avert circulatory collapse, particularly in significant overdose.
Haemodialysis and inotropic support (in this case terlipressin) are important steps in the management of massive caffeine overdose.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Rudolph T, Knudsen K. A case of fatal caffeine poisoning. Acta Anaesthesiol Scand 2010;54:521–3 [DOI] [PubMed] [Google Scholar]
- 2.Holstege CP, Hunter Y, Baer AB, et al. Massive caffeine overdose requiring vasopressin infusion and haemodialysis. J Toxicol Clin Toxicol 2003;41:1003–7 [DOI] [PubMed] [Google Scholar]
- 3.Wrenn KD, Oschner I. Rhabdomyolysis induced by a caffeine overdose. Ann Emerg Med 1989;18:94–7 [DOI] [PubMed] [Google Scholar]
- 4.Kapur R, Smith MD. Treatment of cardiovascular collapse from caffeine overdose with lidocaine, phenylephrine, and hemodialysis. Am J Emerg Med 2009;27:253, .e3–6 [DOI] [PubMed] [Google Scholar]
- 5.Price KR, Fligner DJ. Treatment of caffeine toxicity with Esmolol. Ann Emerg Med 1990;19:44–6 [DOI] [PubMed] [Google Scholar]
- 6.Zimmerman M, Pulliam J, Schwengels J, et al. Caffeine intoxication: a near fatality. Ann Emerg Med 1985;14:1227–9 [DOI] [PubMed] [Google Scholar]
- 7.Forman J, Aizer A, Young CR, et al. Myocardial infarction resulting from caffeine overdose in an anorectic woman. Ann Emerg Med 1997;29:178–80 [DOI] [PubMed] [Google Scholar]


