Abstract
Lipoma is a painless soft tissue tumour of the mesenchymal origin, which is slow growing and well circumscribed. The occurrence of lipoma is rare in the oral cavity (1–4%); however, the frequency is much higher in the head and neck region. The tumour is mostly present in the buccal mucosa, lips, tongue, palate, buccal sulcus and floor of the mouth. Sometimes the tumour becomes large enough to cause difficulty in speech and mastication. Histologically, lipoma is composed of mature fat cells, surrounded by normal fat. We present two cases of intraoral lipoma in two female patients.
Background
Lipomas are the most common soft tissue mesenchymal neoplasms, with 15–20% of cases involving the head and neck region and only 1–4% affecting the oral cavity.1 The first description of oral lipomas was given by Roux in 1848 in a review of alveolar mass; he referred it as a ‘yellow epulis’.2 3 Their aetiology and pathogenesis remain unclear, although mechanical, endocrine and inflammatory influences have been reported.4
Generally intraoral lipomas are slow growing, well circumscribed and painless soft tissue tumours that may be superficially or more deeply located, but has a malignant counterpart called liposarcoma. The most frequent sites of their presentation are buccal mucosa, lips, tongue, palate, buccal sulcus and floor of the mouth.4 Because pain is not a symptom, patients may not be aware of the lesions; but those who are aware, report a slow-growing mass that may have been present from 1 month to 30 years.5
The lipoma usually occurs as a solitary lesion that may be sessile, pedunculated or submerged.6 It ranges in size from a small lesion approximately 1 cm in diameter to a massive tumour of 5 cm×3 cm×2 cm in dimension. Deeper lesions vary in contour and shape ranging from a well-defined, round contoured swelling to a large ill-defined lobulated mass. The colour, often yellow in tone, depends on the thickness of the overlying mucosa. The surface is typically smooth and non-ulcerated except when traumatised.5
Histologically, lipomas can be classified into the following microscopic subtypes: simple lipomas, fibrolipomas, spindle cell lipomas, intramuscular or infiltrating lipomas, salivary gland lipomas, myxoid lipomas and atypical lipomas. Multiple head and neck lipomas have been observed in neurofibromatosis, Gardner syndrome, encephalocraniocutaneous lipomatosis, multiple familial lipomatosis and Proteus syndrome.2
Case presentation
Case 1
A 27-year-old female patient came with the chief complaint of swelling in the left anterior region for 2.5 years. Medical and dental history were insignificant. On extraoral examination, the swelling was non-tender, soft and mobile. On intra oral examination, the swelling was on left buccal mucosa adjacent to canine measuring about 2 cm×2 cm×1 cm (figure 1).
Figure 1.

Case 1: intraoral presentation of the swelling.
Case 2
A 35-year-old female patient reported with the chief complaint of painless swelling on the right side of the cheek since 4 years. The history revealed that the swelling was small before and increased in size within 4 years. Medical and dental history revealed no significant findings except that the patient had frequent cheek biting during mastication due to swelling. On extraoral examination, the swelling was about 3 cm×2 cm×2 cm, soft and mobile (figure 2). On intraoral examination, the swelling was in the right buccal mucosa with the presence of cheek bite at the region of swelling (figure 3).
Figure 2.

Case 2: extraoral appearance of the swelling.
Figure 3.

Case 2: intraoral swelling with cheek biting.
Differential diagnosis
The principal differential diagnosis of lipoma includes fibroma, which is composed of fibrous tissue and is much more firm than lipoma. The differential diagnosis also includes tumours like granular cell tumour, liposarcoma, neurofibroma, mixed tumours, traumatic fibroma and mucocele.
Treatment
Case 1
Routine blood examination of the patient was within normal limits. A written consent form was obtained prior to surgery. An incision was made to expose the lesion (figure 4), the tissue was excised completely (figure 5) and was sent for histopathological examination.
Figure 4.

Case 1: intraoperative view of the swelling.
Figure 5.

Case 1: the excised tissue.
Case 2
After obtaining the patient consent, routine blood examination was done, which was within normal limits. The swelling was operated with complete excision of the tissue (figure 6), which was sent for histopathological examination.
Figure 6.

Case 2: the excised tissue.
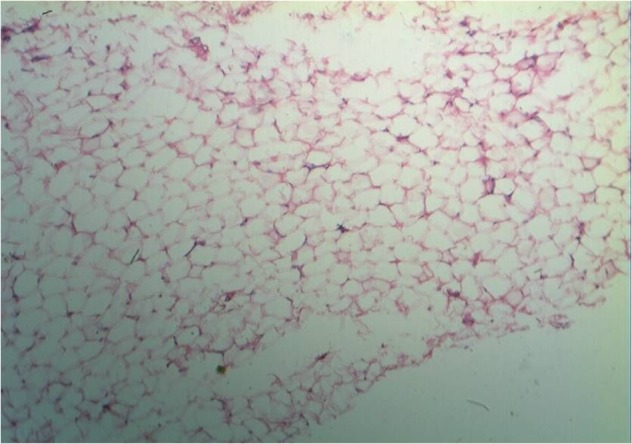
On histopathological examination, both the given H&E-stained soft tissue sections revealed mature fat cells that differed little in the microscopic appearance of the surrounding normal fat. The tumour was well circumscribed and demonstrated a thin fibrous capsule which made the diagnosis of fibrolipoma for both the patients (figures 7 and 8).
Figure 7.
Case 1: microphotograph showing mature fat cells surrounded by normal fat (H&E, ×10).
Figure 8.

Case 2: microphotograph showing mature fat cells with surrounding normal fat (H&E, ×10).
Outcome and follow-up
In both the patients, healing was uneventful and the patients were well satisfied with the surgical results. Follow-up examination of both the patients was done up to 6 months; during this period, no recurrence of the lesion was seen.
Discussion
Lipomas are adipose mesenchymal neoplasms that rarely occur within the oral cavity (1–4%).
Lipids unavailable for metabolism coupled with autonomous growth of lipoma have rendered to be a true benign neoplasm.1 No consensus exists till date regarding the pathogenesis of oral lipoma, where heredity, fatty degeneration, trauma, hormonal basis, infection, infarction, metaphase of muscle cells, lipoblastic embryonic cell nest in origin and chronic irritation are pleasable representative theories to elucidate the pattern of lipoma.6 7 The most common locations of lipoma in the oral cavity have been reported to be in the buccal mucosa followed by tongue,8 which is consistent with our two patients having the lesion in buccal mucosa. The hard palate has very little fatty tissue and the incidence of a lesion here is quite low.2
Occasionally, the lipoma may invade muscles or grow between them, the so-called infiltrating lipoma. It is an uncommon mesenchymal neoplasm that characteristically infiltrates adjacent tissues and tends to recur after excision. This type of lipoma is extremely rare in the head and neck region, and its congenital type is rare.2 They are usually non-tender, soft and almost ‘cheesy’ in the consistency, but may be fluctuant. It is typically superficial in depth; but may infiltrate the muscle, become fixed to surrounding tissues and therefore unmovable. Deeply occurring lesions may produce only a slight surface elevation and may be well encapsulated, more diffuse and less delineated than the superficial variety. Thus, more diffuse form generates the clinical impression of a fluctuant tumour.5
In some cases, lipomas of the buccal mucosal region cannot be distinguished from a herniated buccal fat pad without a history of sudden-onset post-trauma being non-evident. Lipomas of the oral and pharyngeal regions are otherwise simple to differentiate from other lesions, although spindle cell and pleomorphic types must be distinguished from liposarcoma. When metaplastic calcified tissue is present, the lesion may be confused with soft tissue chondroma or osteoma.5
Microscopically it is difficult to differentiate between normal adipose tissue and lipomas; therefore, a clinician sending a surgical specimen to the pathologist for microscopic analysis must provide accurate clinical and surgical information in order to make a definitive diagnosis. The microscopic appearance of a circumscribed but not encapsulated aggregate of mature adipocytes with large clear cytoplasm in the absence of vascularity, atypia or metaplasia is diagnostic of a classical lipoma,9 which is consistent with microscopic findings in our cases. Microscopically, lipomas can be classified into various subtypes; both the our cases were fibrolipomas.
Learning points.
Lipomas found in the oral and maxillofacial region are usually slow-growing lesions.
The clinical course is usually asymptomatic until they get larger in size.
Most of the lipomas develop in subcutaneous tissues but deeper tissues may involve as well, the oral cavity is not commonly affected.
Surgical resection is the main treatment for lipoma. The complete resection should be emphasised during the first surgical operation, which is the key factor in order to avoid recurrence.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Kaur RP, Kler S, Bhullar A. Intra oral lipoma: report of 3 cases. Dent Res J 2011;8:48–51 [PMC free article] [PubMed] [Google Scholar]
- 2.Sekar B, Augustine D, Murli S. Lipoma, a rare intraoral tumor—a case report with review of literature. Oral Maxillofac Pathol J 2011;2:174–7 [Google Scholar]
- 3.Shetty L, Kshirsagar K, Kulkarni D. Lipoma in retromolar area: a case report with review. Med J Dr D Y Patil Univ 2012;5:79–82 [Google Scholar]
- 4.Filho GAN, Caputo BV, Santos CC dos, et al. Diagnosis & treatment of intraoral lipoma: a case report. J Health Sci Inst 2010;282:129–31 [Google Scholar]
- 5.Venkateswarlu M, Geetha P, Srikanth M. A rare case of intraoral lipoma in a six year old child: a case report. Int J Oral Sci 2011;3:43–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Santos LC, Wanderley Rocha SM, Carvalho CN. Intraoral lipoma: an atypical case. Braz J Otorhinolaryngol 2011;77:676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ranginwala A, kale H, Modi T, et al. Intraoral lipoma. J Int Clin Dent Res Organ 2010;23:157–60 [Google Scholar]
- 8.Nayak S, Nayak P. Lipoma of the oral mucosa: a case report. Arch Orofacial Sci 2011;61:37–9 [Google Scholar]
- 9.Adoga AA, Nimkur TL, Manesseh AN. Buccal soft tissue lipoma in an adult Nigerian: a case report and literature review. J Med Case Rep 2008;2:382. [DOI] [PMC free article] [PubMed] [Google Scholar]


