Abstract
The widespread use of imaging technology as a diagnostic tool has resulted in the identification of many previously unknown, clinically benign lesions. The current era of easy access to imaging studies places physicians in a difficult position, since many lesions are not precisely diagnosed by imaging. For example, the accurate diagnosis of non-functioning adrenal lesions remains a clinical challenge. This report describes a patient with the incidental CT finding of an uncommon adrenal ganglioneuroma. Clinical and radiological findings can guide suspicion towards this rare lesion; however, the actual diagnosis is based on histological findings. Specific characteristics of adrenal ganglioneuromas that would allow their diagnosis without invasive procedures have not been established. This case report is an attempt to add more data that will help to establish diagnostic criteria for this rare disease.
Background
The routine use of sophisticated imaging techniques has resulted in a problem, increasingly recognised in current medical practice. The unexpected discovery of a clinically silent adrenal tumour is a result of this modern medical technology.1 Although radiological evaluation is crucial in guiding the differential diagnosis of benign and malignant adrenal tumours, it produces a diagnosis problem for clinicians when they are presented with presumably benign, non-functional adrenal masses. Adrenal ‘incidentalomas’ are being discovered in the course of work-ups or treatments of conditions not related to adrenal disease.2 We report a patient with an incidental adrenal mass that was managed laparoscopically and diagnosed as an adrenal ganglioneuroma. The present case brings into focus the idea that, even in an era of advanced healthcare technology, some diagnoses are only possible through the use of invasive approaches; this particularly applies to rare lesions such as that presented here. This case report confirms the known clinical and radiological data that should guide the diagnosis when the uncommon adrenal ganglioneuroma is suspected.
Case presentation
A woman presented to our hospital with a history of unstable angina and left bundle branch block. She did not have any other known medical conditions, such as hypertension, or any stigmata of hypercortisolism or hyperaldosteronism. As part of her cardiology work-up, the patient underwent a coronary angiography guided by CT. The CT identified a nodular lesion in the right adrenal gland, measuring 4.3×2.9 cm and appearing heterogeneous with coarse calcifications. The lesion displayed non-enhanced attenuation values of less than 40 Hounsfield units (figure 1). Functional evaluation showed a non-functioning tumour; all laboratory tests were normal, including free cortisol in a 24-hour urine sample, 1 mg dexamethasone suppression testing, serum testing for basal cortisol, adrenocorticotropic hormone and renin, plasma testing for aldosterone, and blood and urine testing for catecholamines (epinephrine and norepinephrine) and their metabolites. Neither clinical nor radiological assessment could confirm the nature of the mass; a laparoscopic right adrenal excision was therefore performed. Pathology revealed a right adrenal ganglioneuroma (figures 2 and 3).
Figure 1.
Angio CT: nodular lesion of the right adrenal gland with 4.3×2.9 cm, heterogeneous with coarse calcifications and non-enhanced attenuation (less than 40 Hounsfield units).
Figure 2.
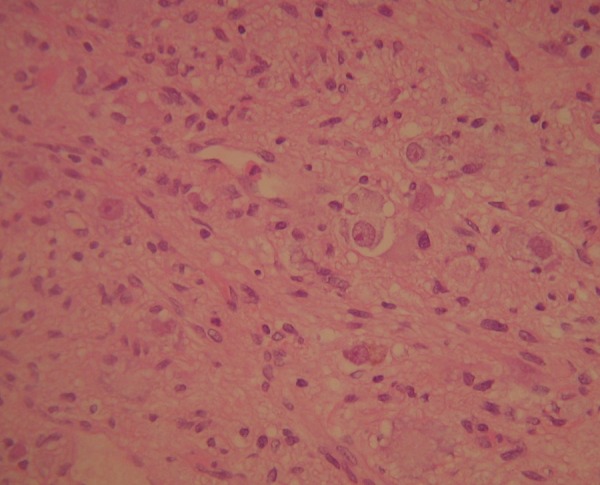
Adrenal ganglioneuroma. Microscopic aspects: Schwan elongated cells, with regular nuclei without atypia or mitotic activity visible, scattered. Mature ganglion cells, arranged in an isolated or forming small aggregates.
Figure 3.
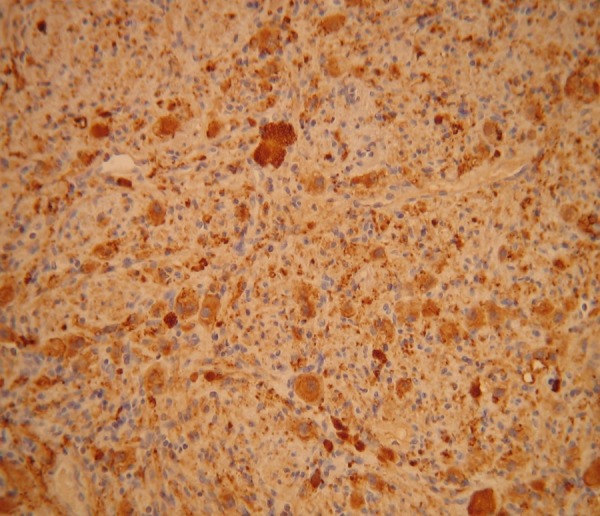
Immunohistochemistry. Positivity of the spindle celss (Schwan cells) for S100. Ganglion cells are positive for synaptophysin, neuron specific enolase and chromogranin.
Investigations
CT is an effective diagnostic tool for asymptomatic cortical lesions, such as myelolipomas or adenomas, but not for ganglioneuromas. However, it may help to support or at least suggest the diagnosis of ganglioneuroma by identifying typical characteristics as a round-to-lobulated shape or a solid heterogeneous mass without evidence of tumour invasion. Punctate calcifications are identified in 2.4% to 60% of cases;3 4 this finding is also seen in adrenal carcinoma. MRI typically reveals a low non-enhanced T1-weighted signal, a slightly high and heterogeneous T2-weighted signal and a late, gradual enhancement on dynamic MRI.4 These findings, however, are shared by other lesions and can lead away from the correct diagnosis.
Macroscopically, these lesions are frequently large, non-encapsulated, gelatinous tumours. Pathological examination gives the definitive diagnosis, revealing a predominance of neurofibroma-like areas composed of Schwann cells that exhibit scant-spindled cytoplasm, curly dark nuclei and discrete nucleoli. These Schwann cells appear mixed together with ganglion cells that exhibit abundant eosinophilic cytoplasm and large vesicular nuclei with prominent nucleoli; the ganglion cells may be isolated or may form small aggregates (figure 2).3 Immunohistochemistry reveals that the ganglion cells are positive for synaptophysin, neuron-specific enolase, CD56 and the neuron-specific protein 9.5, and the Schwann cells are positive for CD100 (figure 3).
Differential diagnosis
Although these tumours carry an excellent prognosis, they are a diagnostic challenge for physicians.
Adrenal incidentalomas are clinically relevant when hormone overproduction is present or radiological findings indicate a risk of malignancy. The most common incidentalomas are non-functioning cortical adenomas, followed by pheochromocytomas, cortisol-secreting adenomas and aldosteronomas. A thorough radiological and functional evaluation of any incidentaloma is mandatory.
Adrenal ganglioneuromas are rare, benign, slow-growing tumours that arise from the primary sympathetic neurons of the neural crest. Tumours derived from the sympathetic chain may occur along the paravertebral sympathetic ganglia, from the neck to the pelvis. They are more common in the posterior retroperitoneum (40%) and rarely found in the adrenal gland.5 6 Adrenal tumours are found incidentally in 1–10% of abdominal CT scans; of these, 1% to 6% are ganglioneuromas.6 Ganglioneuromas do not seem to exhibit a preference for either gender, but are more common in the fourth and fifth decades of life.3
Ganglioneuromas are usually non-functioning, but approximately 37% can secrete catecholamines and their metabolites, including vasoactive intestinal peptide. When hormone activity exists, the patient may experience diarrhoea from vasoactive intestinal peptide release,3 sweating or high blood pressure.5 Although most ganglioneuromas occur sporadically, familial dispositions have been reported, as has an association with Turner syndrome and multiple endocrine neoplasia II.3 7 Unlike other adrenal lesions such as ganglioblastomas and neuroblastomas, ganglioneuromas have no documented malignant potential.
Treatment
Clinical and radiographic monitoring is usually performed in patients with non-functioning lesions less than 4 cm in size; however, some authors advise surgical excision in young patients because of the very long follow-up period that would otherwise be required.8 The indication for surgery in patients with incidental, non-functioning adrenal tumours is not clearly defined, and treatment for lesions from 4 to 6 cm is controversial; both surgical excision and monitoring have been recommended. Laparoscopy is the procedure of choice when excision is performed.6 8 9 The present patient was submitted to a transperitoneal laparoscopic right adrenal excision.
Outcome and follow-up
Four years after surgery, the patient has not had any local or distant recurrence.
Discussion
Adrenal ganglioneuromas are uncommon, benign, non-functioning adrenal masses. Most published series of adrenal lesions describe tumours discovered by routine imaging studies. It is crucial to identify specific criteria that could facilitate the correct preoperative diagnosis. This report aims to shed some light on the clinical, laboratory and histological characteristics of this benign lesion.
Learning points.
In our opinion, it is very important to be aware of adrenal ganglioneuromas. As radiological ‘incidentalomas’ are more frequently found, clinically irrelevant adrenal ganglioneuromas may be increasingly diagnosed.
The diagnosis of adrenal ganglioneuromas constitutes a clinical challenge. Since it is a rare entity, there are insufficient data to allow a precise preoperative diagnosis. The results of radiological studies and the patient's clinical presentation permit a diagnosis of suspicion, based on a pattern found in other patients and described in this report.
Histological examination remains the mainstay of diagnosis and should be thorough to exclude malignant foci that portend a worse outcome.
Although suspicion for an adrenal ganglioneuroma can be based on previously published data, there is a need for specific findings and characteristics that will lead to a non-invasive, accurate diagnosis.
Footnotes
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Terzolo M, Bovio S, Pia A, et al. Management of adrenal incidentaloma. Best Pract Res Clin Endocrinol Metab 2009;23:233–43 [DOI] [PubMed] [Google Scholar]
- 2.Grumbach MM, Biller BM, Braunstein GD, et al. Management of the clinically inapparent adrenal mass (‘incidentaloma’). Ann Intern Med 2003;138:424–9 [DOI] [PubMed] [Google Scholar]
- 3.Allende DS, Hansel DE, MacLennan GT. Ganglioneuroma of the adrenal gland. J Uro 2009;182:714–15 [DOI] [PubMed] [Google Scholar]
- 4.Maweja S, Materne R, Detrembleur N, et al. Adrenal ganglioneuroma. Am J Surg 2007;194:683–4 [DOI] [PubMed] [Google Scholar]
- 5.Garcia A Titos, Plaza CP Ramirez, Dieguez P Ruiz, et al. [Ganglioneuroma as an uncommon cause of adrenal tumour]. Endocrinol Nutr: Organo Soc Espanola Endocrinol Nutr 2011;58:443–5 [DOI] [PubMed] [Google Scholar]
- 6.Zografos GN, Kothonidis K, Ageli C, et al. Laparoscopic resection of large adrenal ganglioneuroma. JSLS 2007;11:487–92 [PMC free article] [PubMed] [Google Scholar]
- 7.Kamoun M, Mnif MF, Rekik N, et al. Ganglioneuroma of adrenal gland in a patient with Turner syndrome. Ann Diagn Pathol 2010;14:133–6 [DOI] [PubMed] [Google Scholar]
- 8.Yamaguchi K, Hara I, Takeda M, et al. Two cases of ganglioneuroma. Urology 2006;67:622 e1–4 [DOI] [PubMed] [Google Scholar]
- 9.Martinez F Arredondo, Delgado M Soto, Fernandez A Benavente, et al. [Adrenal ganglioneuroma. Report of a new case]. Actas urol espanolas 2003;27:221–5 [DOI] [PubMed] [Google Scholar]



