Abstract
Infertility affects about 8% to 12% of couples, with male infertility being responsible for about 30% of cases. Sexually transmitted infections (STIs) are known to cause complications of pregnancy and are associated with tubal infertility in females, but the association with male fertility is still controversial. The prevalence of curable STIs has risen to an estimated 448 million a year with the number of people living with human immunodeficiency virus (HIV) at 34 million. This review looks at the evidence available to date, regarding the effect of STIs and male accessory gland infections on markers of male fertility and the evidence that STIs negatively affect sexual functioning, thus adversely affecting the ability to conceive. The review will also cover new developments in the use of medications and fertility treatments as an aid to conception in couples serodiscordant for HIV.
Keywords: Fertility, Male accessory gland infections, Men, Sexual function, Sexually transmitted infections
INTRODUCTION
Sexually transmitted infections (STIs) are common worldwide. There were an estimated 34 million people living with human immunodeficiency virus (HIV) in 2010 [1] and the estimated number of new infections with curable STIs has risen to 448 million per year [2]. Pelvic inflammatory disease (PID), a complication of chlamydia and gonorrhoea, is associated with female tubal infertility. STIs are known to cause complications in pregnancy including miscarriage, preterm labour and still birth. Some STIs can also have a significant effect on the morbidity and mortality of the neonate. However, the effect of these infections on male fertility is less clear.
The medical definition of infertility is the failure to conceive after 12 months of unprotected intercourse. This condition is estimated to affect about 8% to 12% of couples [3] with an estimated 48.5 million couples worldwide unable to have a child after five years [4]. Though often perceived as a female disorder, male infertility is thought to be responsible for around 30% of cases with an additional 20% to 30% caused by combined male and female factors. Infertility is a very emotive condition and has significant impact on the psychological health of the couples involved. The World Health Organization (WHO) definition of health is "a state of complete physical, mental and social well-being, and not merely the absence of disease or infirmity." Thus, infertility does adversely affect health.
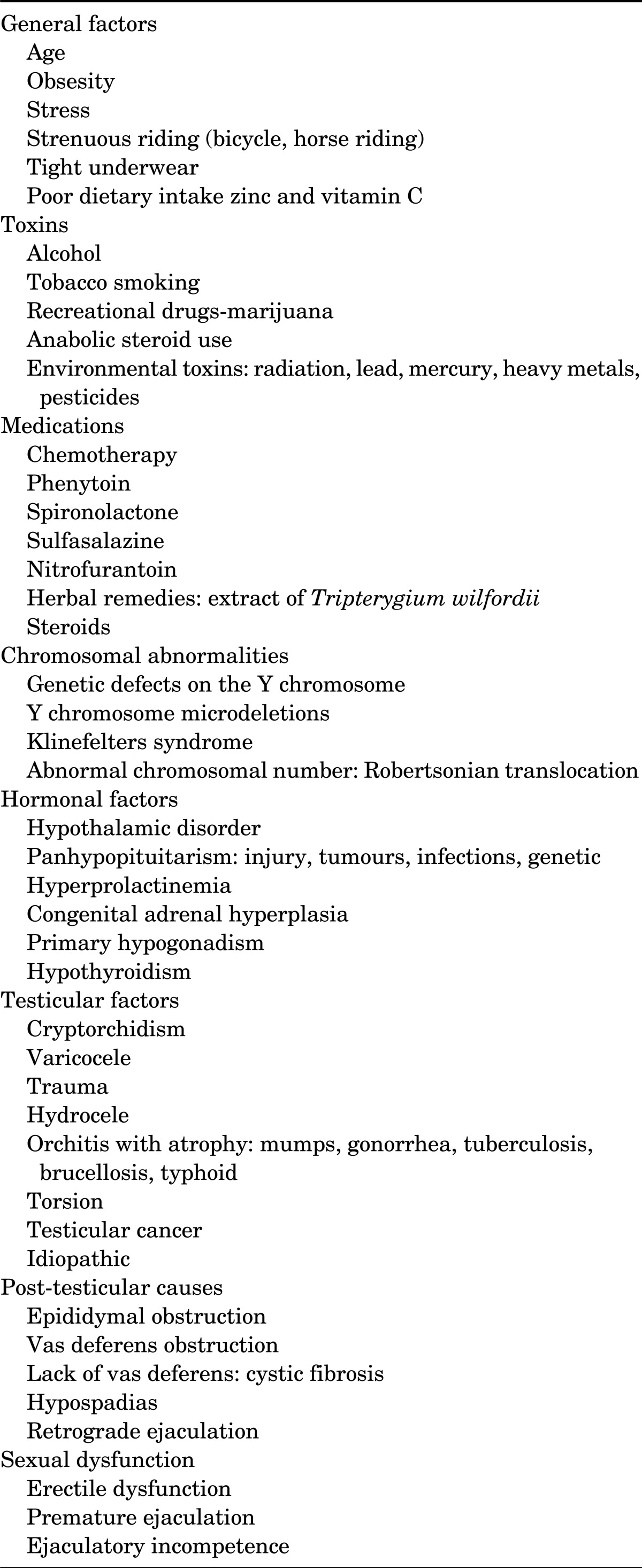
There are many factors that affect male fertility (Table 1). We review the available evidence linking male infertility and sexual function with STIs. Another important factor to consider when assessing fertility is sexual function. Men with erectile dysfunction tend to have problems with penetrative sex. The psychological effect of a sexual infection may impact on sexual functioning. Addressing such issues may alleviate symptoms and allow natural conception.
TABLE 1.
Causes of male infertility
MALE ACCESSORY GLAND INFECTIONS
Male accessory gland infections (MAGIs) include prostatitis, urethritis, epididymitis and orchitis. These infections are potentially curable causes of male infertility, though studies so far have not been conclusive in showing an effect on sperm quality and male fertility. Comhaire et al. [5] performed a double blind prospective study looking at the effect of doxycycline in infertile couples with MAGI. Only 1.6% of infertile couples evaluated had abnormal semen quality with the presence of MAGI as the only demonstrable cause. Sperm motility and morphology showed improvement over time, whether treated or not, but this improvement did not seem to enhance the probability of conception.
Prostatitis is often listed as a cause of male infertility, but the evidence for this is inconclusive. Nonetheless, it is logical to consider that any disease process that affects prostate function may affect spermatozoa and fertility.
Prostatitis has recently been classified into four distinct conditions by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) of the National Institutes of Health. Acute bacterial prostatitis, chronic bacterial prostatitis, chronic prostatitis/chronic pelvic pain (this may be inflammatory or noninflammatory) and, finally, asymptomatic inflammatory prostatitis, which is often found coincidentally when investigating other urological conditions or fertility issues. Hopefully, with this clear definition of chronic prostatitis that can be used worldwide, it will be easier to compare studies in the future, allowing categorization and evaluation of chronic prostatitis and its relationship with male fertility.
A study by Christiansen et al. [6] published in 1991 compared patients with a diagnosis of chronic abacterial prostatovesiculitis (current NIDDK classification of chronic prostatitis/chronic pelvic pain) with age-matched asymptomatic controls. The patients in the prostatitis group all had ultrasound evidence of chronic inflammatory changes. The study showed that patients in this group had an increased incidence of disturbed sperm quality and azoospermia, though some were normospermic. Not all patients in the prostatitis group had leukospermia and the degree of the leukospermia did not predict the extent of the disturbance of semen quality. Giamarellou et al. [7] investigated 30 men with chronic prostatitis and leukocytosis who had been treated with long term antimicrobials. There was an improvement or normalization of the sperm count in 70% of these men. Chronic prostatitis is associated with several pathogens, and it is possible that some pathogens may have a greater effect on fertility than others. For example, a study by Mazzoli et al. [8] compared the effect of chronic prostatitis due to Chlamydia trachomatis with chronic prostatitis due to other uropathogens. In this study, chronic prostatitis associated with chlamydia caused lower sperm concentration, poor motility and affected morphology more than the effect of prostatitis due to other uropathogens.
Urethritis is most commonly caused by infections with C. trachomatis, Neisseria gonorrhea, Ureaplasma urealyticum or Mycoplasma genitalium. Other less common causes are Trichomonas vaginalis (TV), Herpes simplex virus (HSV), allergic reactions and trauma. There have been several studies investigating the effect on sperm quality and fertility of these bacterial pathogens. Rybar et al. [9] demonstrated that semen contaminations with Mycoplasma spp. and chlamydia were associated with decreased sperm concentrations, with mycoplasma having the greatest adverse effect on sperm quality (concentration, motility, morphology and DNA condensation). However, despite successful antibiotic treatment, semen quality parameters did not improve at 3 months post treatment. When assessing sperm chromatin integrity by the presence of DNA breaks, there was no evidence that this was associated with either Mycoplasma spp. or chlamydia. A study in the United Kingdom (UK) recently found that there were more abnormalities of semen parameters in attendees of Genitourinary clinics, especially those patients with asymptomatic, chlamydia negative, nonspecific urethritis than in men seeing a general practioner for evaluation of possible infertility [10]. Contradictory to this, Gunyeli et al. [11] found no difference in the prevalence of the pathogens associated with urethritis, when comparing fertile and infertile couples. It is possible that the coexistence of other factors simultaneously present with an infection may lead to impaired fertility.
C. trachomatis is one of the most common STIs worldwide and the most commonly reported bacterial STI in England and the United State (US). The majority of cases in males are asymptomatic. Possible infertility is a common anxiety when given a diagnosis of chlamydial infection. Chlamydia is associated with PID and female tubal infertility, although the connection is less clear in relation to male fertility where the research has been contradictory and inconclusive.
Several studies over the years have shown that the detection of Chlamydia in either semen or urine has been associated with a reduction in some of the parameters of sperm function and number. Rybar et al. [9] showed a reduction in sperm numbers. Separate studies by Cengiz et al. [12], Gallegos et al. [13], Gdoura et al. [14], and Kokab et al. [16] all confirm that the presence of Chlamydia is indeed associated with a reduction of the percentage of progressively motile sperm with Cengiz et al. [12] also demonstrating abnormal morphology and reduced viability. Gallegos et al. [13], reported sperm DNA fragmentation that improved when the Chlamydia infection was treated, this is contradictory to the findings of Gdoura et al. [14], who found no evidence of DNA fragmentation. Despite showing a reduced percentage of progressively motile sperm Kokab et al. [15], found no evidence of an effect on the percentage of immotile or viable sperm and Vigi et al. [16], showed no significant effect on sperm concentration, motility and/or morphology at all. Contradictory findings have also occurred in studies looking at the effect of the presence of C. trachomatis antibodies on fertility, with Joki-Korpela et al. [17] suggesting an association, whereas Ochsendorf et al. [18] found that, despite an associated inflammatory response, there was no effect on sperm parameters. It has been shown that the presence of elementary bodies of C. trachomatis serovar E within the lab setting caused a significant decrease in motile sperm with an increase in dead spermatozoa [19], thus suggestive of some direct effect of Chlamydia on sperm.
There are several theories as to how Chlamydia may affect male fertility. These include a direct effect of the Chlamydia organism, the presence of associated inflammation, or the development of antisperm antibodies triggered by Chlamydia. The results of studies to date have been inconclusive in determining whether there is any effect on male fertility due to Chlamydia and if there is such an effect, whether it is resolved by treatment.
Gonorrhea is caused by N. gonorrheae, a gram-negative diplococcus. Worldwide, there are an estimated 62 million people infected annually [20]. It is the second most common STI in the UK and a common cause of urethritis. In England, there were 20,965 cases in 2011, a 25% rise from 2010 [21]. In 10% of cases of gonorrhoea, there is concurrent chlamydial infection. If not promptly or adequately treated, the subsequent scarring and obliteration of the epididymal canal following an acute infection is usually persistent even after cure. If bilateral, the infection will result in obstructive azoospermia [22]. With increasing multi drug resistance gonorrhea, this complication may become more prevalent in the future.
Acute epididymitis is most commonly caused by bacterial infection. A STI such as chlamydia or gonorrhea is the most common cause in men less than 35 years of age. In older men, especially those with a history of bladder outlet obstruction, Escherichia coli is more common. Rarer causes of epididymitis include Mycobaterium tuberculosis. Non infectious causes include Behcet's disease, urethral manipulation, post vasectomy, and as an adverse effect of amiodorone. Syphilitic epididymitis has also been described and classified into three forms: acute diffuse interstitial, chronic diffuse interstitial, and gummatous [23]. With any chronic inflammatory process, there is a risk of fibrosis and scarring with the potential to cause obstruction of the epididymis. Though uncommon, bilateral occlusion of the epididymides is a cause of azoospermia and, therefore, male infertility.
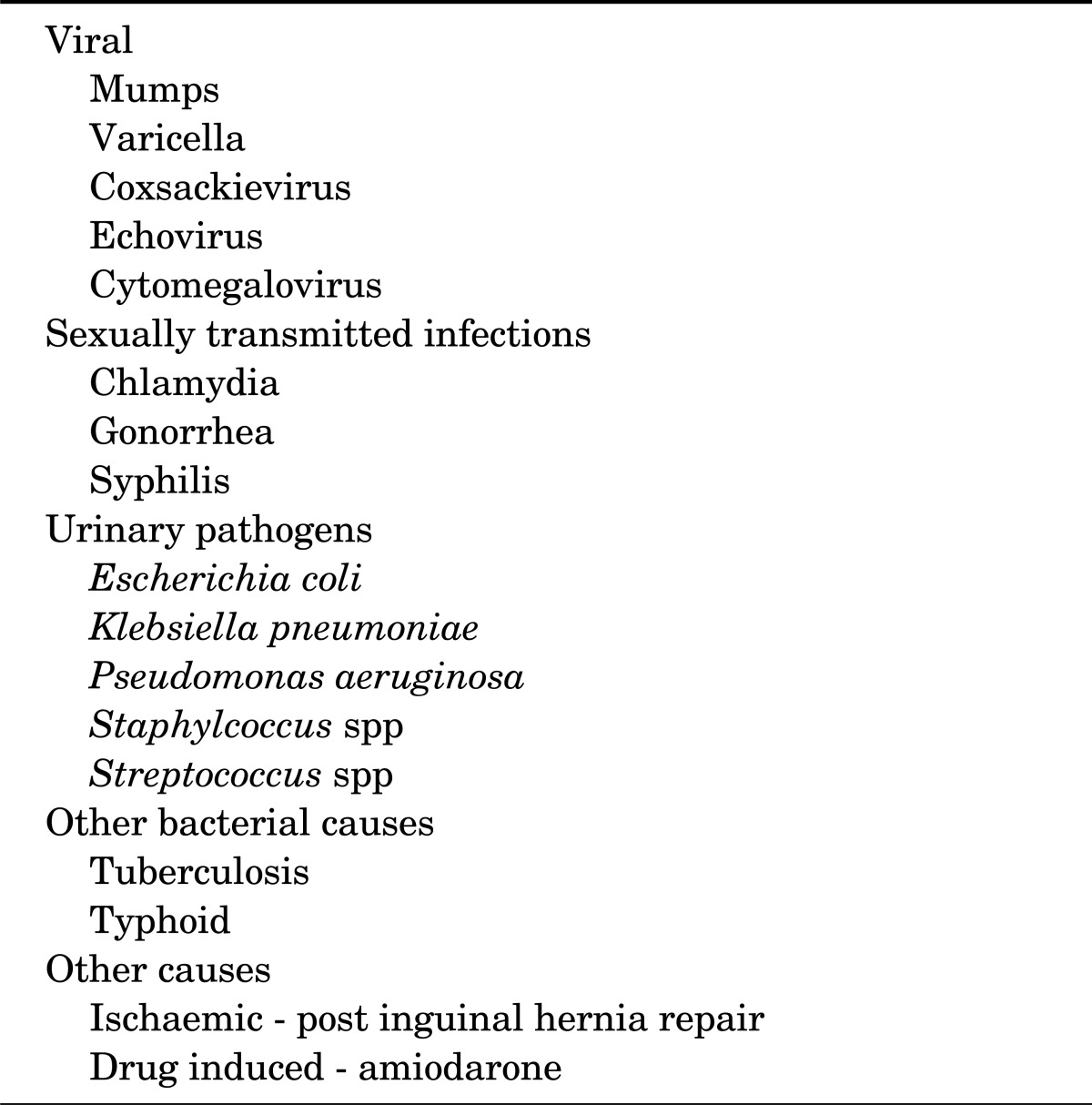
Orchitis may be caused by a variety of viral or bacterial infections (Table 2). The most well known cause is mumps, which is commonly associated with unilateral or bilateral orchitis if it occurs after puberty. This can cause reduced fertility. Though uncommon, complications of orchitis include testicular atrophy or infarction and may affect fertility.
TABLE 2.
Causes of orchitis
VIRAL STIs
Genital herpes is caused by HSV type 1 and 2. After initial inoculation, the virus travels continuously between the skin or mucous membrane and the sensory nerve bodies. Schiffer et al. [24] recently demonstrated that recurrence occurs only when the virus is no longer controlled by the CD8 dermal cells. Previously it was postulated that transmission only occurred with active disease, but although transmission is most likely during periods of activity, Wald et al. [25] demonstrated that asymptomatic shedding of the virus does occur without evidence of lesions. Fleming et al. [26] found that, in the US, up to 90% of people who are HSV type 2 antibody positive have never knowingly had an outbreak of genital herpes. With the development of polymerase chain reaction (PCR) techniques, the diagnosis of active HSV has improved. Serum antibody tests can be performed, but only confirm previous exposure to HSV 1 or 2.
Conclusive evidence for the association of HSV 1 and 2 with infertility is lacking. El Borai et al. [27] did show that HSV DNA has been found more frequently in infertile men. Regarding the effect on sperm count and motility, the results of studies are very contradictory. Several studies have shown a significant effect of HSV [28-30], specifically on sperm count and motility, whereas many other studies dispute this association [27,31]. Bezold et al. [28] have shown that HSV positive men have a reduction in citrate and alpha glucosidase levels, which is associated with impaired prostate and epididymal function and may well be postulated as a causative link to abnormal semen parameters. Kundsin et al. [32] and El Borai et al. [33] have both observed that treating couples for HSV with acyclovir has led to pregnancy, though these studies were on a small number of couples.
The frequency of sexual activity is important, especially in subfertile couples. If either partners is suffering from frequent bouts of HSV, this may affect the frequency and timing of unprotected sexual intercourse. Suppressive treatment with antivirals is known to reduce the clinical episodes of HSV infection and also asymptomatic shedding of the virus. Corey et al. [34] demonstrated that daily suppressive treatment with valaciclovir reduced transmission rates in serodiscordant couples. Reducing the frequency of episodes of HSV, allowing more frequent unprotected sex, and with the reassurance of a lowered transmission risk, conception rates may be improved.
There are more than 30-40 types of human papillomavirus (HPV) that are known to affect the genital region. Dunne et al. [35] recently published US prevalence rates of 26.8% among females aged 14 to 59 years.
Studies of HPV and male fertility have tended to focus on subtypes 16 and 18, the high grade oncogenic viruses. The studies to date are conflicting in their findings, and it is not clear that HPV affects fertility. Bezold et al. [28], showed that the presence of HPV significantly reduced total sperm count, with Lai et al. [36] demonstrating associated asthenospermia. A trend towards impaired sperm function was seen in several other studies, though the results were not statistically significant. [35-37] In contrast, Rintala et al. [37] and Tanaka et al. [38] saw no effect on sperm volume, sperm concentration or vitality of sperm, nor any associated oligospermia or asthenospermia. Rintala et al. [37] postulate that it is unclear whether HPV has a direct effect on the sperm or if the presence of HPV alters the pH of the semen, thus impairing sperm motility.
Although the global epidemic of HIV seems to have stabilised with only an estimated 2.7 million new infections per year compared to the peak of 3.2 million in 1997, more people worldwide are living with HIV infection due to the development and increased availability of highly active antiretroviral therapy (HAART). In 2010, UNAIDS (Joint United Nations Programme on HIV/acquired immune deficiency syndrome [AIDS]) estimated 34 million people were living with HIV infection [1]. Most people, if diagnosed early in the disease, should expect a near to normal life expectancy. This, with the reduction of mother to child transmission with HAART to 0.1% [39] has changed people's perceptions of conceiving with HIV.
HIV has been shown to impact on male fertility. Shevchuk et al. [40] showed that with prolongation of survival in AIDS patients, there was a more pronounced loss of germ cells within the testes. Several studies have shown abnormal sperm parameters, while others, such as Crum-Crianflone et al. [41], suggest that HIV is a known cause of secondary hypogonadism and thus a low testosterone level. Low testosterone is associated with a reduced sperm count. Crittenden et al. [42] showed that HIV positive men have more viscous semen containing fewer motile sperm and more round cells. Nicopoullos et al. [43] also described a significant alteration in sperm parameters in HIV positive men, with reduced ejaculate volume, sperm concentration, progressive motility and total count. Less normal morphology was seen. There was a positive correlation observed between CD4 count and sperm concentration, total count, motility, progressive motility type 'a'+'b' and postpreparation concentration, and also a significant negative correlation with normal sperm morphology. Nicopoullos et al. [43] went on to show that taking HAART with a HIV viral load of <1,000 copies/mL is associated with a significantly improved intrauterine in semination (IUI) outcome.
HIV-positive status and conception is a challenging problem when dealing with serodiscordant couples. If one partner is HIV positive and the other is HIV negative, how does a couple conceive when we promote safe sex and condom use to prevent transmission? If it is only the female that is HIV positive, this is easily overcome by using self-insemination. Untreated HIV infection is associated with an increased risk of spontaneous abortion, stillbirth and prematurity. Antenatal screening and the use of HAART has reduced these risks but despite treatment HIV positive women are still less likely to conceive than HIV negative women.
If the male is HIV positive in the serodiscordant couple, sperm washing is the ideal way to conceive. Unfortunately, not all couples have access to sperm washing, but other options are now available. Sperm washing has been shown to be safe in protecting the female partner and child from HIV infection. Bujan et al. [44] reported that in over 3,390 cycles of sperm washing, there has been no documented seroconversion of the child or female partner. The technique used separates the sperm from the seminal fluid and non germinal cells that potentially carry HIV. The process uses centrifugation and a "swim up" method that has been shown by Kato et al. [45] to provide spermatozoa that are HIV-1 RNA and proviral DNA negative. This sperm is then used to fertilize the woman during ovulation via IUI or, if needed, in vitro fertilization or intracytoplasmic sperm injection.
ARVs can be used to reduce transmission risk and is an option for couples who do not have access to sperm washing. Though these methods do not guarantee transmission prevention, it is thought to be a safe option to consider. Pre-exposure chemoprophylaxis (PrEP) is the use of daily antiretroviral medication in HIV seronegative people to reduce the risk of becoming HIV seropositive through sexual exposure. The 'Partners in PrEP Study', led by the University of Washington's International Clinical Research Center, showed a reduction in risk of HIV transmission by 75% (95% confidence interval, 55 to 87; p<0.001) using once daily tenofovir-emtricitabine (Truvada) [46]. The Food and Drug Administration has recently approved the combination of tenovofir and emtricitabine for use in PrEP. An alternative is to treat the HIV positive partner with HAART and obtain an sustained undetectable viral load in the plasma. In 2008, "The Swiss statement" published by the Swiss Federal Commission on AIDS Related Issues, stated clearly after reviewing the literature that an HIV-infected individual is sexually noninfectious provided the individual complies with antiretroviral therapy (ART), the viral load has been nondetectable for at least six months, and there are no additional sexually transmitted diseases present [47]. A report from the HPTN 052 study of heterosexual couples was subsequently released and showed that early initiation of ART led to a 96 percent reduction in HIV transmission to the HIV uninfected partner [48]. For serodiscordant couples who wish to conceive naturally, the BHIVA (British HIV Association) recommends undergoing fertility testing before commencing unprotected sexual intercourse in order to assess whether natural conception is an option [49].
TRICHOMONAS VAGINALIS
WHO figures estimate 173.46 million cases of TV in 1999, the most common STI worldwide. The estimated prevalence in the US is 3.1% [50]. Infection tends to be asymptomatic, only causing symptoms in about 30% of cases. The association of TV and infertility is controversial. Tuttle et al. [51] demonstrated in vitro mixing of sperm with trichomonas reduced sperm activity. Jarecki-Black et al. [52] reported that a proteinaeous substance produced by TV kills sperm rapidly. Gopalkrishnan et al. [53] showed that the presence of trichomonas was associated with reduced sperm motility and viability with a reduction in the percentage of normal morphology. Treatment significantly improved these parameters in 50% of men after one dose of metronidazole. Conversely, a study by Daly et al. [54] showed no effect on sperm number or motility in the presence of trichomonas in vitro. Though inconclusive, the evidence suggests that if there is an effect on sperm due to the presence of trichomonas, it should in theory be reversible.
SYPHILIS
There are an estimated 12 million new infections reported annually worldwide [55]. In the UK, the Health Protection Agency publishes yearly rates of infectious syphilis (primary, secondary or early latent). After a peak in 2005, the rates have reduced slightly to 5.6 per 100,000 in 2011 [56]. There were 45,834 reported cases of syphilis in 2010 in the US, at a rate of 14.9 per 100,000 [57]. Disturbingly, some countries have seen a dramatic rise in reported syphilis. The newly independent states of the former Soviet Union had an estimated rate of 120-170 per 100,000 in 1999, compared to 5-15 per 100,000 in 1990 [55].
Although a direct toxic effect of syphilis on male fertility has not been reported in the literature, complications of syphilis can affect fertility. Syphilitic epididymitis has the potential to cause obstruction of the epididymis. Chronic obliterative endarteritis and interstitial inflammation can occur in congenital or tertiary syphilis and lead to small, fibrotic testes [58]. Gummatous lesions cause destruction of the local tissue and, if occurring in the testicles, may have an impact on testicular function and fertility. There can also be an indirect effect: tabes dorsalis, a form of neurosyphilis, can cause erectile dysfunction.
Much more common than the complications of syphilis are the devastating effects of untreated infectious syphilis on pregnancy and the newborn. Spontaneous abortion and still birth occur in 50% of pregnancies, with mortality of infected infants being over 10% [59]. Before proceeding with any form of fertility treatment, it is imperative that both partners should be tested for syphilis and treated when indicated.
STIs AND SEXUAL FUNCTION
In addition to any physical effect, the psychological effect of having an STI may also have an adverse impact on both male sexual function and fertility and therefore should not be overlooked. Specifically, psychological stress is common in patients with prostatitis. 43% of men with symptomatic prostatitis complain of erectile dysfunction and 24% report low libido [60], thus adversely affecting the ability to conceive. HSV is a very stigmatizing disease, in part due to the incurable nature of the virus. The psychological distress and psychosexual problems associated with a diagnosis of HSV infection and recurrent HSV infections have been well described in the literature, though there is some debate as to whether these are due to long term effects of HSV infection or whether some patients are predisposed to anxiety [61-63], Carney demonstrated that suppressive therapy for HSV can result in reduction in anxiety [64]. As previously suggested, suppressive treatment in serodiscordant couples for HSV may not only increase the frequency of sex by reducing episodes of HSV, but also improve the psychological impact of HSV and concern regarding transmission, thereby improving sexual function. In practice, we often see young men complaining of sexual dysfunction after a diagnosis of HPV infection has been made, although research data is conflicting as to whether HPV causes psychological problems affecting sexual enjoyment and frequency of intercourse [65-68]. Lamba et al. [69] showed that HIV positive males were more likely to suffer from erectile dysfunction and low sexual desire. Furthermore, patients on HAART were found to have raised estradiol levels that were associated with low sexual desire [69,70].
CONCLUSIONS
Whether STIs affect male fertility is still open to debate. There are historical issues when comparing these studies. Different methods of reporting sperm abnormalities continue to be used, despite the WHO having set standards for the examination and processing of human semen in 1980. The fifth edition, published in 2010 has addressed such issues and provides more practical guidance for laboratories and technicians [71]. Hopefully this will allow a standardized approach pertaining to methods of sperm collection, measurement, and interpretation worldwide and enable a more robust comparison of results. There is also the practical difficulty of obtaining normal control samples of sperm in large enough numbers to provide significant results.
Diagnostic criteria are also being clarified. For example, the NIDDK have recategorized prostatitis. Additionally, there are national and international guidelines for diagnosis and treatment of STIs which should provide a basis for comparable research in the future.
Another critical aspect of any study design is the diagnosis of infection. Over the last few years, there has been a dramatic change in commonly used diagnostic testing with the increasing use of NAATS and PCR techniques. The newer tests tend to be easier to perform and also have better sensitivities when compared to those previously available. Older studies may have found a lower prevalence of infection due to the lack of positive diagnosis. It must also be considered that most tests performed are for acute/active disease. It would be ideal when studying infertility and the long term sequelae of STIs if there were markers of previous infection. Immunoglobulin G (IgG) for HSV indicates previous exposure to the virus, but not the site of infection, nor the current clinical state of infection. Although markers (i.e., serum IgG for chlamydia) for previous infection are used in the research setting, these markers are generally not specific for genital infections. At present, not all STIs have markers for previously acquired infection. Consequently, the infectious agent itself, the inflammatory response provoked, the physical damage, the duration of untreated disease and the psychological effect of having an STI may all play a part in any resultant infertility, making it difficult to exclude the effect of confounding variables and influences when designing and comparing studies. In the meantime, the screening and treatment of both those at risk of STIs and infertile couples will help reduce the risk of infertility and the known complications of pregnancy.
Footnotes
The authors have nothing to disclose.
References
- 1.UNAIDS. UNAIDS world AIDS day report 2011 [Internet] Geneva: Joint United Nations Programme on HIV/AIDS (UNAIDS); [cited 2013 Jan 30]. Available from: http://www.unaids.org/en/media/unaids/contentassets/documents/unaidspublication/2011/JC2216_WorldAIDSday_report_2011_en.pdf. [Google Scholar]
- 2.World Health Organization (WHO) Sexually transmitted infections Fact sheet N°110 August 2011 [Internet] Geneva: WHO; c2013. [cited 2013 Jan 16]. Available from: http://www.who.int/mediacentre/factsheets/fs110/en/ [Google Scholar]
- 3.World Health Organization (WHO) Infertility: a tabulation of available data on prevalence of primary and secondary infertility. WHO/MCH/91.9 [Internet] Geneva: WHO, Division of Family Health, Programme on Maternal and Child Health and Family Planning; c2013. [cited 2013 Jan 16]. Available from: http://whqlibdoc.who.int/hq/1991/WHO_MCH_91.9.pdf. [Google Scholar]
- 4.Mascarenhas MN, Flaxman SR, Boerma T, Vanderpoel S, Stevens GA. National, regional, and global trends in infertility prevalence since 1990: a systematic analysis of 277 health surveys. PLoS Med. 2012;9:e1001356. doi: 10.1371/journal.pmed.1001356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Comhaire FH, Rowe PJ, Farley TM. The effect of doxycycline in infertile couples with male accessory gland infection: a double blind prospective study. Int J Androl. 1986;9:91–98. doi: 10.1111/j.1365-2605.1986.tb00871.x. [DOI] [PubMed] [Google Scholar]
- 6.Christiansen E, Tollefsrud A, Purvis K. Sperm quality in men with chronic abacterial prostatovesiculitis verified by rectal ultrasonography. Urology. 1991;38:545–549. doi: 10.1016/0090-4295(91)80175-7. [DOI] [PubMed] [Google Scholar]
- 7.Giamarellou H, Tympanidis K, Bitos NA, Leonidas E, Daikos GK. Infertility and chronic prostatitis. Andrologia. 1984;16:417–422. doi: 10.1111/j.1439-0272.1984.tb00388.x. [DOI] [PubMed] [Google Scholar]
- 8.Mazzoli S, Cai T, Addonisio P, Bechi A, Mondaini N, Bartoletti R. Chlamydia trachomatis infection is related to poor semen quality in young prostatitis patients. Eur Urol. 2010;57:708–714. doi: 10.1016/j.eururo.2009.05.015. [DOI] [PubMed] [Google Scholar]
- 9.Rybar R, Prinosilova P, Kopecka V, Hlavicova J, Veznik Z, Zajicova A, et al. The effect of bacterial contamination of semen on sperm chromatin integrity and standard semen parameters in men from infertile couples. Andrologia. 2012;44(Suppl 1):410–418. doi: 10.1111/j.1439-0272.2011.01198.x. [DOI] [PubMed] [Google Scholar]
- 10.Carne CA, Chilcott S, Palmer C, Green O, Bridge S, Walsh R, et al. Low sperm counts in genitourinary medicine clinic attendees: results from a case-control study. Sex Transm Infect. 2012;88:422–426. doi: 10.1136/sextrans-2011-050310. [DOI] [PubMed] [Google Scholar]
- 11.Gunyeli I, Abike F, Dunder I, Aslan C, Tapısız OL, Temizkan O, et al. Chlamydia, Mycoplasma and Ureaplasma infections in infertile couples and effects of these infections on fertility. Arch Gynecol Obstet. 2011;283:379–385. doi: 10.1007/s00404-010-1726-4. [DOI] [PubMed] [Google Scholar]
- 12.Cengiz T, Aydoganli L, Baykam M, Mungan NA, Tuncbilek E, Dincer M, et al. Chlamydial infections and male infertility. Int Urol Nephrol. 1997;29:687–693. doi: 10.1007/BF02552187. [DOI] [PubMed] [Google Scholar]
- 13.Gallegos G, Ramos B, Santiso R, Goyanes V, Gosalvez J, Fernandez JL. Sperm DNA fragmentation in infertile men with genitourinary infection by Chlamydia trachomatis and Mycoplasma. Fertil Steril. 2008;90:328–334. doi: 10.1016/j.fertnstert.2007.06.035. [DOI] [PubMed] [Google Scholar]
- 14.Gdoura R, Keskes-Ammar L, Bouzid F, Eb F, Hammami A, Orfila J. Chlamydia trachomatis and male infertility in Tunisia. Eur J Contracept Reprod Health Care. 2001;6:102–107. [PubMed] [Google Scholar]
- 15.Kokab A, Akhondi MM, Sadeghi MR, Modarresi MH, Aarabi M, Jennings R, et al. Raised inflammatory markers in semen from men with asymptomatic chlamydial infection. J Androl. 2010;31:114–120. doi: 10.2164/jandrol.109.008300. [DOI] [PubMed] [Google Scholar]
- 16.Vigil P, Morales P, Tapia A, Riquelme R, Salgado AM. Chlamydia trachomatis infection in male partners of infertile couples: incidence and sperm function. Andrologia. 2002;34:155–161. doi: 10.1046/j.1439-0272.2002.00472.x. [DOI] [PubMed] [Google Scholar]
- 17.Joki-Korpela P, Sahrakorpi N, Halttunen M, Surcel HM, Paavonen J, Tiitinen A. The role of Chlamydia trachomatis infection in male infertility. Fertil Steril. 2009;91(4 Suppl):1448–1450. doi: 10.1016/j.fertnstert.2008.06.051. [DOI] [PubMed] [Google Scholar]
- 18.Ochsendorf FR, Ozdemir K, Rabenau H, Fenner T, Oremek R, Milbradt R, et al. Chlamydia trachomatis and male infertility: chlamydia-IgA antibodies in seminal plasma are C. trachomatis specific and associated with an inflammatory response. J Eur Acad Dermatol Venereol. 1999;12:143–152. [PubMed] [Google Scholar]
- 19.Hosseinzadeh S, Brewis IA, Eley A, Pacey AA. Co-incubation of human spermatozoa with Chlamydia trachomatis serovar E causes premature sperm death. Hum Reprod. 2001;16:293–299. doi: 10.1093/humrep/16.2.293. [DOI] [PubMed] [Google Scholar]
- 20.World Health Organization (WHO) Initiative for vaccine research (IVR): sexually transmitted diseases [Internet] Geneva: WHO; c2013. [cited 2013 Jan 30]. Available from http://www.who.int/vaccine_research/diseases/soa_std/en/index2.html. [Google Scholar]
- 21.Health Protection Agency. Health protection report (weekly report). Volume 6 Number 22 Published on: 1 June 2012 [Internet] London: Health Protection Agency; c2013. [cited 2013 Jan 30]. Available from: http://www.hpa.org.uk/hpr/archives/2012/hpr2212.pdf. [Google Scholar]
- 22.Harkness AH. The pathology of gonorrhoea. Br J Vener Dis. 1948;24:137–147. [PMC free article] [PubMed] [Google Scholar]
- 23.Michelson HE. Syphilis of the epididymis. JAMA. 1919;73:1431–1433. [Google Scholar]
- 24.Schiffer JT, Abu-Raddad L, Mark KE, Zhu J, Selke S, Koelle DM, et al. Mucosal host immune response predicts the severity and duration of herpes simplex virus-2 genital tract shedding episodes. Proc Natl Acad Sci U S A. 2010;107:18973–18978. doi: 10.1073/pnas.1006614107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wald A, Zeh J, Selke S, Warren T, Ryncarz AJ, Ashley R, et al. Reactivation of genital herpes simplex virus type 2 infection in asymptomatic seropositive persons. N Engl J Med. 2000;342:844–850. doi: 10.1056/NEJM200003233421203. [DOI] [PubMed] [Google Scholar]
- 26.Fleming DT, McQuillan GM, Johnson RE, Nahmias AJ, Aral SO, Lee FK, et al. Herpes simplex virus type 2 in the United States, 1976 to 1994. N Engl J Med. 1997;337:1105–1111. doi: 10.1056/NEJM199710163371601. [DOI] [PubMed] [Google Scholar]
- 27.el Borai N, Inoue M, Lefevre C, Naumova EN, Sato B, Yamamura M. Detection of herpes simplex DNA in semen and menstrual blood of individuals attending an infertility clinic. J Obstet Gynaecol Res. 1997;23:17–24. doi: 10.1111/j.1447-0756.1997.tb00799.x. [DOI] [PubMed] [Google Scholar]
- 28.Bezold G, Politch JA, Kiviat NB, Kuypers JM, Wolff H, Anderson DJ. Prevalence of sexually transmissible pathogens in semen from asymptomatic male infertility patients with and without leukocytospermia. Fertil Steril. 2007;87:1087–1097. doi: 10.1016/j.fertnstert.2006.08.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kapranos N, Petrakou E, Anastasiadou C, Kotronias D. Detection of herpes simplex virus, cytomegalovirus, and Epstein-Barr virus in the semen of men attending an infertility clinic. Fertil Steril. 2003;79(Suppl 3):1566–1570. doi: 10.1016/s0015-0282(03)00370-4. [DOI] [PubMed] [Google Scholar]
- 30.Kotronias D, Kapranos N. Detection of herpes simplex virus DNA in human spermatozoa by in situ hybridization technique. In Vivo. 1998;12:391–394. [PubMed] [Google Scholar]
- 31.Bezold G, Schuster-Grusser A, Lange M, Gall H, Wolff H, Peter RU. Prevalence of human herpesvirus types 1-8 in the semen of infertility patients and correlation with semen parameters. Fertil Steril. 2001;76:416–418. doi: 10.1016/s0015-0282(01)01920-3. [DOI] [PubMed] [Google Scholar]
- 32.Kundsin RB, Falk L, Hertig AT, Horne HW., Jr Acyclovir treatment of twelve unexplained infertile couples. Int J Fertil. 1987;32:200–204. [PubMed] [Google Scholar]
- 33.El Borai N, LeFevre C, Inoue M, Naumova EN, Sato K, Suzuki S, et al. Presence of HSV-1 DNA in semen and menstrual blood. J Reprod Immunol. 1998;41:137–147. doi: 10.1016/s0165-0378(98)00054-0. [DOI] [PubMed] [Google Scholar]
- 34.Corey L, Wald A, Patel R, Sacks SL, Tyring SK, Warren T, et al. Once-daily valacyclovir to reduce the risk of transmission of genital herpes. N Engl J Med. 2004;350:11–20. doi: 10.1056/NEJMoa035144. [DOI] [PubMed] [Google Scholar]
- 35.Dunne EF, Unger ER, Sternberg M, McQuillan G, Swan DC, Patel SS, et al. Prevalence of HPV infection among females in the United States. JAMA. 2007;297:813–819. doi: 10.1001/jama.297.8.813. [DOI] [PubMed] [Google Scholar]
- 36.Lai YM, Lee JF, Huang HY, Soong YK, Yang FP, Pao CC. The effect of human papillomavirus infection on sperm cell motility. Fertil Steril. 1997;67:1152–1155. doi: 10.1016/s0015-0282(97)81454-9. [DOI] [PubMed] [Google Scholar]
- 37.Rintala MA, Grenman SE, Pollanen PP, Suominen JJ, Syrjanen SM. Detection of high-risk HPV DNA in semen and its association with the quality of semen. Int J STD AIDS. 2004;15:740–743. doi: 10.1258/0956462042395122. [DOI] [PubMed] [Google Scholar]
- 38.Tanaka H, Karube A, Kodama H, Fukuda J, Tanaka T. Mass screening for human papillomavirus type 16 infection in infertile couples. J Reprod Med. 2000;45:907–911. [PubMed] [Google Scholar]
- 39.Townsend CL, Cortina-Borja M, Peckham CS, de Ruiter A, Lyall H, Tookey PA. Low rates of mother-to-child transmission of HIV following effective pregnancy interventions in the United Kingdom and Ireland, 2000-2006. AIDS. 2008;22:973–981. doi: 10.1097/QAD.0b013e3282f9b67a. [DOI] [PubMed] [Google Scholar]
- 40.Shevchuk MM, Pigato JB, Khalife G, Armenakas NA, Fracchia JA. Changing testicular histology in AIDS: its implication for sexual transmission of HIV. Urology. 1999;53:203–208. doi: 10.1016/s0090-4295(98)00463-4. [DOI] [PubMed] [Google Scholar]
- 41.Crum-Cianflone NF, Bavaro M, Hale B, Amling C, Truett A, Brandt C, et al. Erectile dysfunction and hypogonadism among men with HIV. AIDS Patient Care STDS. 2007;21:9–19. doi: 10.1089/apc.2006.0071. [DOI] [PubMed] [Google Scholar]
- 42.Crittenden JA, Handelsman DJ, Stewart GJ. Semen analysis in human immunodeficiency virus infection. Fertil Steril. 1992;57:1294–1299. [PubMed] [Google Scholar]
- 43.Nicopoullos JD, Almeida PA, Ramsay JW, Gilling-Smith C. The effect of human immunodeficiency virus on sperm parameters and the outcome of intrauterine insemination following sperm washing. Hum Reprod. 2004;19:2289–2297. doi: 10.1093/humrep/deh426. [DOI] [PubMed] [Google Scholar]
- 44.Bujan L, Hollander L, Coudert M, Gilling-Smith C, Vucetich A, Guibert J, et al. Safety and efficacy of sperm washing in HIV-1-serodiscordant couples where the male is infected: results from the European CREAThE network. AIDS. 2007;21:1909–1914. doi: 10.1097/QAD.0b013e3282703879. [DOI] [PubMed] [Google Scholar]
- 45.Kato S, Hanabusa H, Kaneko S, Takakuwa K, Suzuki M, Kuji N, et al. Complete removal of HIV-1 RNA and proviral DNA from semen by the swim-up method: assisted reproduction technique using spermatozoa free from HIV-1. AIDS. 2006;20:967–973. doi: 10.1097/01.aids.0000222067.07255.2d. [DOI] [PubMed] [Google Scholar]
- 46.Baeten JM, Donnell D, Ndase P, Mugo NR, Campbell JD, Wangisi J, et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N Engl J Med. 2012;367:399–410. doi: 10.1056/NEJMoa1108524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Vernazza P, Hirschel B, Bernasconi E, Flepp M. Les personnes séropositives ne souffrant d’aucune autre MST et suivant un traitment antirétroviral efficace ne transmettent pas le VIH par voie sexuelle. Bulletin des médecins suisses. Schweizerische Ärztezeitung Bollettino dei medici svizzeri. 2008;89:5. English translation [Internet]. [cited 2013 Jan 30]. Available from: http://www.edwinjbernard.com/pdfs/Swiss%20Commission%20statement_May%202008_translation%20EN.pdf. [Google Scholar]
- 48.National Institutes of Health. Treating HIV-infected people with antiretrovirals protects partners from infection: findings result from NIH-funded International Study [Internet] Bethesda: National Institutes of Health; [cited 2013 Jan 30]. Available from: http://www.niaid.nih.gov/news/newsreleases/2011/Pages/HPTN052.aspx. [Google Scholar]
- 49.Fakoya A, Lamba H, Mackie N, Nandwani R, Brown A, Bernard E, et al. British HIV Association, BASHH and FSRH guidelines for the management of the sexual and reproductive health of people living with HIV infection 2008. HIV Med. 2008;9:681–720. doi: 10.1111/j.1468-1293.2008.00634.x. [DOI] [PubMed] [Google Scholar]
- 50.Sutton M, Sternberg M, Koumans EH, McQuillan G, Berman S, Markowitz L. The prevalence of Trichomonas vaginalis infection among reproductive-age women in the United States, 2001-2004. Clin Infect Dis. 2007;45:1319–1326. doi: 10.1086/522532. [DOI] [PubMed] [Google Scholar]
- 51.Tuttle JP, Jr, Holbrook TW, Derrick FC. Interference of human spermatozoal motility by trichomonas vaginalis. J Urol. 1977;118:1024–1025. doi: 10.1016/s0022-5347(17)58285-3. [DOI] [PubMed] [Google Scholar]
- 52.Jarecki-Black JC, Lushbaugh WB, Golosov L, Glassman AB. Trichomonas vaginalis: preliminary characterization of a sperm motility inhibiting factor. Ann Clin Lab Sci. 1988;18:484–489. [PubMed] [Google Scholar]
- 53.Gopalkrishnan K, Hinduja IN, Kumar TC. Semen characteristics of asymptomatic males affected by Trichomonas vaginalis. J In Vitro Fert Embryo Transf. 1990;7:165–167. doi: 10.1007/BF01135682. [DOI] [PubMed] [Google Scholar]
- 54.Daly JJ, Sherman JK, Green L, Hostetler TL. Survival of Trichomonas vaginalis in human semen. Genitourin Med. 1989;65:106–108. doi: 10.1136/sti.65.2.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.World Health Organisation (WHO) Global prevalence and incidence of selected curable sexually transmitted infections overview and estimates [Internet] Geneva: WHO; c2013. [cited 2012 Jul 24]. Available from: http://www.who.int/hiv/pub/sti/who_hiv_aids_2001.02.pdf. [Google Scholar]
- 56.Health Protection Agency. Sexually transmitted infections annual data [Internet] London: Health Protection Agency; c2013. [cited Jan 30]. Available from: http://www.hpa.org.uk/web/HPAweb&Page&HPAwebAutoListName/Page/1201094610372. [Google Scholar]
- 57.Centers for Disease Control and Prevention. 2010 sexually transmitted diseases surveillance [Internet] Atlanta: Centers for Disease Control and Prevention; [cited 2013 Jan 30]. Available from: http://www.cdc.gov/std/stats10/syphilis.htm. [Google Scholar]
- 58.Cheng L, Bostwick DG, editors. Essentials of anatomic pathology. Totowa: Humana Press; 2002. [Google Scholar]
- 59.World Health Organisation (WHO) Standards for maternal and neonatal care. Prevention of mother-to-child transmission of syphilis. Integrated management of pregnancy and childbirth (IMPAC) [Internet] Geneva: WHO; c2013. [cited Jan 30]. Available from http://www.who.int/reproductivehealth/publications/maternal_perinatal_health/prevention_mtct_syphilis.pdf. [Google Scholar]
- 60.Mehik A, Hellstrom P, Sarpola A, Lukkarinen O, Jarvelin MR. Fears, sexual disturbances and personality features in men with prostatitis: a population-based cross-sectional study in Finland. BJU Int. 2001;88:35–38. doi: 10.1046/j.1464-410x.2001.02259.x. [DOI] [PubMed] [Google Scholar]
- 61.Brookes JL, Haywood S, Green J. Adjustment to the psychological and social sequelae of recurrent genital herpes simplex infection. Genitourin Med. 1993;69:384–387. doi: 10.1136/sti.69.5.384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Catotti DN, Clarke P, Catoe KE. Herpes revisited. Still a cause of concern. Sex Transm Dis. 1993;20:77–80. [PubMed] [Google Scholar]
- 63.Rosenthal SL, Zimet GD, Leichliter JS, Stanberry LR, Fife KH, Tu W, et al. The psychosocial impact of serological diagnosis of asymptomatic herpes simplex virus type 2 infection. Sex Transm Infect. 2006;82:154–157. doi: 10.1136/sti.2005.016311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Carney O, Ross E, Ikkos G, Mindel A. The effect of suppressive oral acyclovir on the psychological morbidity associated with recurrent genital herpes. Genitourin Med. 1993;69:457–459. doi: 10.1136/sti.69.6.457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Conaglen HM, Hughes R, Conaglen JV, Morgan J. A prospective study of the psychological impact on patients of first diagnosis of human papillomavirus. Int J STD AIDS. 2001;12:651–658. doi: 10.1258/0956462011923877. [DOI] [PubMed] [Google Scholar]
- 66.Maw RD, Reitano M, Roy M. An international survey of patients with genital warts: perceptions regarding treatment and impact on lifestyle. Int J STD AIDS. 1998;9:571–578. doi: 10.1258/0956462981921143. [DOI] [PubMed] [Google Scholar]
- 67.Reed BD, Ruffin MT, Gorenflo DW, Zazove P. The psychosexual impact of human papillomavirus cervical infections. J Fam Pract. 1999;48:110–116. [PubMed] [Google Scholar]
- 68.Clarke P, Ebel C, Catotti DN, Stewart S. The psychosocial impact of human papillomavirus infection: implications for health care providers. Int J STD AIDS. 1996;7:197–200. doi: 10.1258/0956462961917618. [DOI] [PubMed] [Google Scholar]
- 69.Lamba H, Goldmeier D, Mackie NE, Scullard G. Antiretroviral therapy is associated with sexual dysfunction and with increased serum oestradiol levels in men. Int J STD AIDS. 2004;15:234–237. doi: 10.1258/095646204773557749. [DOI] [PubMed] [Google Scholar]
- 70.Goldmeier D, Scullard G, Kapembwa M, Lamba H, Frize G. Does increased aromatase activity in adipose fibroblasts cause low sexual desire in patients with HIV lipodystrophy? Sex Transm Infect. 2002;78:64–66. doi: 10.1136/sti.78.1.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.World Health Organisation (WHO) WHO laboratory manual for the examination and processing of human semen. Fifth edition [Internet] Geneva: WHO; c2013. [cited 2013 Jan 30]. Available from: http://whqlibdoc.who.int/publications/2010/9789241547789_eng.pdf. [Google Scholar]


