Abstract
Purpose
Percutaneous nephrolithotomy (PCNL) has been the preferred procedure for the removal of large renal stones in Iran since 1990. Recently, we encountered a series of devastating neurologic complications during PCNL, including paraplegia and hemiplegia. There are several reports of neurologic complications following PCNL owing to paradoxical air emboli, but there are no reports of paraplegia following PCNL.
Materials and Methods
We retrospectively reviewed the medical records of patients who had undergone PCNL in 13 different endourologic centers and retrieved data related to neurologic complications after PCNL, including coma, paraplegia, hemiplegia, and quadriplegia.
Results
The total number of PCNL procedures in these 13 centers was 30,666. Among these procedures, 11 cases were complicated by neurologic events, and four of these cases experienced paraplegia. All events happened with the patient in the prone position with the use of general anesthesia and in the presence of air injection. There were no reports of neurologic complications in PCNL procedures performed with the patient under general anesthesia and in the prone position and with contrast injection.
Conclusions
It can be assumed that using room air to opacify the collecting system played a major role in the occurrence of these complications. Likewise, the prone position and general anesthesia may predispose to these events in the presence of air injection.
Keywords: Complications, Nephrolithotomy, Neurologic deficits, Paraplegia
INTRODUCTION
Percutaneous nephrolithotomy (PCNL), first reported in 1976 [1], is a minimally invasive surgery for the treatment of renal stones [2]. It has been the preferred procedure for the removal of large renal stones in Iran since 1990. During these years, Iranian endourologists have encountered some complications during or after PCNL.
We encountered an unknown and devastating complication during PCNL last year: a female patient became paraplegic following an uneventful PCNL. We reviewed the medical literature, but we did not find reports of any similar complications. With consideration of the ethical issues surrounding this event, the Urology and Nephrology Research Center, which is affiliated with the Shahid Beheshti University of Medical Sciences, planned a widespread research project to study the possible etiologies of this event. Questionnaires consisting of a series of questions about the occurrence of neurologic complications following PCNL were sent to all Iranian endourologists. Surprisingly, we encountered new cases of neurologic complications following PCNL that had not been reported as PCNL complications by endourologists because they had found no logical link between the complications and the PCNL. There are several reports of nonparaplegic neurologic complications following PCNL owing to paradoxical air emboli [3-7], but to the best of our knowledge, there are no reports of paraplegia following PCNL. The cases of paraplegia in this study are therefore the first such cases to be presented.
MATERIALS AND METHODS
We retrospectively reviewed the medical records for PCNL in 13 different endourologic centers and retrieved data related to neurologic complications, including coma, paraplegia, hemiplegia, and quadriplegia. With the exception of a few differences, all of the endourologists generally performed PCNL in a similar manner.
After the induction of general anesthesia, the patient was located in the lithotomy position and a 5- or 6-Fr ureteral catheter, without a ureteropelvic junction occlusion balloon, was inserted through the ipsilateral ureter. Then, the position of the patient was changed to the prone position. Iodinated contrast materials were the most widely used means of opacifying the collecting system, but some endourologists preferred room air. PCNL was usually performed through the antegrade percutaneous access; once the targeted calyx was identified with fluoroscopy, an 18-gauge needle directed to the aforementioned calyx and a J-tip guidewire were passed. The most widely used methods of tract dilatation were metal telescoping and semi-rigid Amplatz dilatators. After tract dilatation, a rigid nephroscope was inserted through an open, low-pressure system; thereafter, lithotripsy was performed by use of ballistic lithotripters.
In two centers (Yasooj and Jahrom), PCNL was routinely performed under spinal anesthesia. In one center (Rasht), it was generally performed in the supine position (complete supine PCNL). The amount of air injection for opacifying the collecting system often varied between 20 and 50 mL, but some endourologists used room air in amounts much greater than this range. With the exception of one center, transverse rolls were located under the shoulders and anterior superior iliac spines of the patients who were in the prone position. In one center, a wedge foam pad was put under the thorax and abdomen in such a manner that the stone-containing side would be elevated at approximately 30 degrees. With the exception of one center in which half-saline solution was used as the irrigant solution, distilled water was the irrigant solution of choice. It is worth mentioning that the irrigant solution was provided at room temperature. In pediatrics, only normal saline was used in all centers.
To investigate the possible causes of serious neurologic complications, we classified the cases into 4 groups (A, B, C, and D) according to their clinical manifestations and positive findings.
RESULTS
The total number of PCNL procedures in these 13 centers was 30,666. Among these procedures, 11 cases were complicated by neurologic events, and 4 of these cases experienced paraplegia. The pathogenic region in these four patients was determined to be in the spinal cord. The others had pathogenic regions in the upper parts of the nervous system. The data retrieved from the medical records of these cases are presented in Tables 1, 2.
TABLE 1.
Detailed information about PCNL in different centers
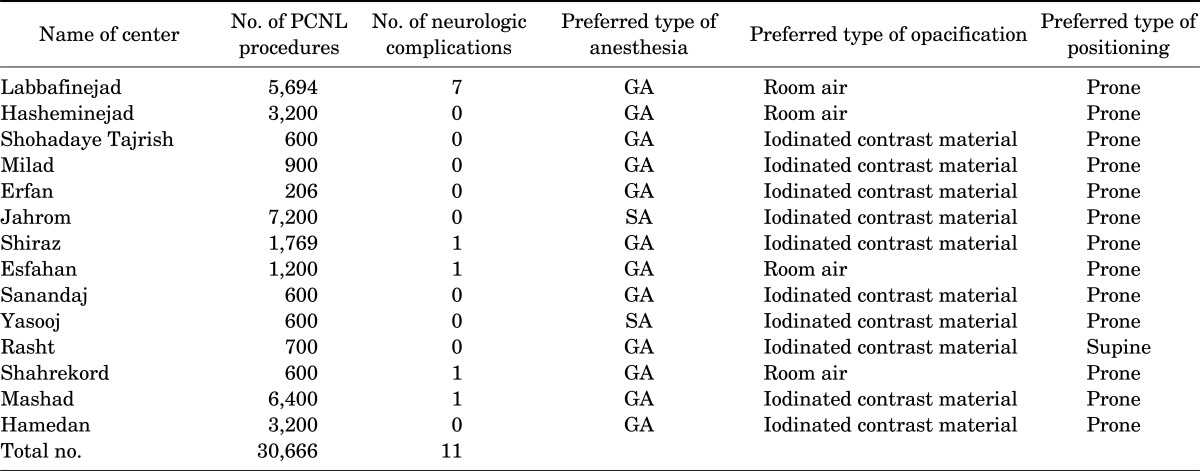
PCNL, percutaneous nephrolithotomy; GA, general anesthesia; SA, spinal anesthesia.
TABLE 2.
Retrieved data from the medical records of cases with neurologic complications after PCNL
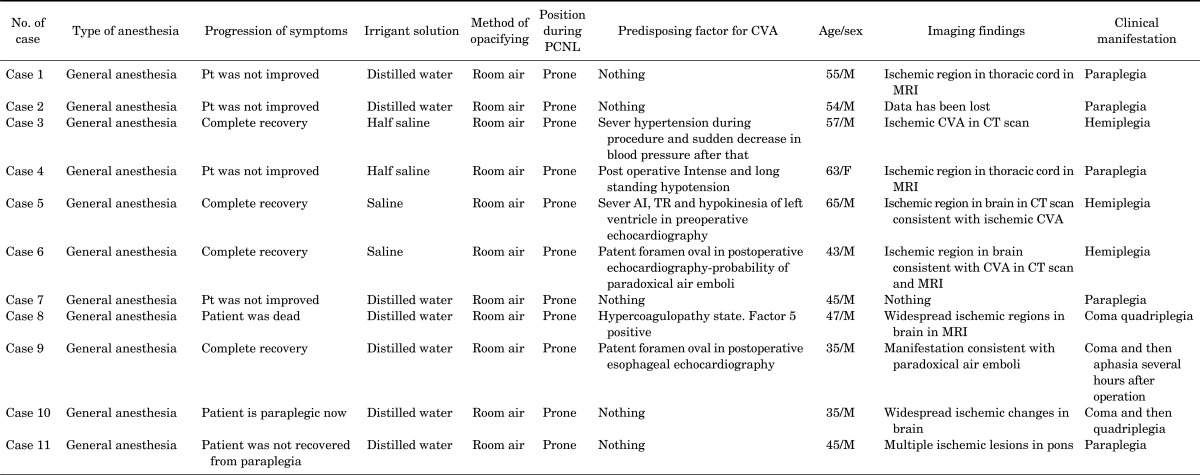
PCNL, percutaneous nephrolithotomy; CVA, cereberovascular accident; Pt, patient; MRI, magnetic resonance imaging; CT, computed tomography; AI, aortic insufficiency; TR, tricuspid regurgitation.
Group A (consisted of cases 1, 2, 4, and 7): In these cases, PCNL was performed with the patients under general anesthesia in the prone position. The endourologists used room air to opacify the collecting system. The irrigant solution in cases 1, 2, and 4 was half-saline solution and that in case 7 was distilled water. Magnetic resonance imaging in cases 1 and 4 revealed ischemic regions in the thoracic cord.
Group B (consisted of cases 6 and 9): These two patients were young and had no risk factors for cerebrovascular accident (CVA). PCNL was performed with the patients under general anesthesia and in the prone position. Room air was used to opacify the collecting system. The irrigant solution was half-saline solution and distilled water in cases 6 and 9, respectively. Case 6 became hemiplegic after the operation, which was a transient complication. In case 9, after injection of 17 mL room air during the pyelography, cardiovascular collapse and arrhythmia occurred; thus, the operation was terminated and the patient became conscious. After several hours, the patient went into a coma, and following coma remission, he became aphasic for several days. Investigations in these two cases revealed a patent foramen oval in postoperative echocardiography, which was a predisposing factor for paradoxical air emboli.
Group C (consisted of cases 3 and 5): In these two cases, in which CVA occurred following PCNL, the procedure was performed with the patients under general anesthesia and in the prone position. The irrigant solution was half-saline solution, and room air was used to opacify the collecting system. In these two cases, a predisposing factor for CVA was present. In case 3, who was a known case of hypertension, a marked reduction in blood pressure following severe intraoperative hypertension led to an ischemic stroke. In case 5, in whom a thromboembolic stroke occurred after PCNL, preoperative echocardiography revealed severe aortic valve insufficiency and the presence of a hypokinetic region in the left ventricular wall, which could be the cause of the cerebral thromboemboli in this patient.
Group D (consisted of cases 8, 10, and 11): We could not categorize these cases in the above-mentioned groups. In these three cases, no predisposing factor for CVA was present. The pathogenic region in these cases was located in areas above the spinal cord. We found no evidence for paradoxical air emboli in these cases. However, surprisingly, as in other the cases, PCNL in all of these patients was performed with the patients under general anesthesia in the prone position, and room air was used to opacify the collecting system.
DISCUSSION
Although neurologic defects including paraplegia, hemiplegia, and quadriplegia are rare during or after PCNL, these events can occur and can result in devastation to the patient and noticeable financial and emotional pressures on the patient's relatives. With consideration of the ethical issues related to this event, we designed a widespread study to recognize the possible etiologies of neurologic complications during or after PCNL.
We could not find any cases similar to group A in the medical literature following PCNL, but there are comparable case reports for other types of surgery that are performed in the prone position [8-10]. A case series by Bhardwaj et al. [8] reported new neurologic deficits that were known to happen after spine surgery. They presented four patients with cervical myeloradiculopathy who had undergone cervical laminectomy or fusion or both in the prone position, supported by chest rolls. Three cases were intubated and positioned while they were conscious, whereas the fourth case was positioned after induction. The procedures were successfully concluded, except for temporary episodes of hypotension intraoperatively. In the recovery room, all cases had new neurologic deficits. Nothing was found on urgent computed tomography myelography or re-exploration. The cases all progressively improved with high-dose steroids and induction of hypertension. The authors concluded that the prone position in conjunction with compression on the abdomen can compromise the spinal cord perfusion and cause spinal cord ischemia. They recommended using a frame that prevents abdominal compression and perioperative hypotension so as to maintain sufficient spinal cord perfusion during and after the surgery.
In another case report, Langmayr et al. [9] presented a 33-year-old man undergoing surgery for a unilateral single-level disc herniation at L4 to L5. He developed quadriplegia and signs of occipital lobe dysfunction in a few hours after the procedure. Magnetic resonance imaging demonstrated intramedullary ischemic changes in the cervical spinal cord. These authors concluded that a short-term mechanical occlusion of a vertebral artery can cause stasis, thrombi, and then embolism in the vertebrobasilar vessels; therefore, surgeons should avoid excessive head rotation and neck extension in the prone position.
We reviewed the literature for case reports of air emboli (group B) during PCNL. There were several reports of cases with suspicious air emboli during PCNL [3-7]. Manifestations and findings in these case reports were similar to those of group B.
For example, in a case report by Song et al. [5], a 37-year-old man was referred for right calyceal diverticulum with milk of calcium. After induction of general anesthesia, the patient was put in the lithotomy position. A 6-Fr ureteral catheter with ureteropelvic junction occlusion balloon was inserted through the right ureter, and the case was rotated to the prone position. The authors performed pyelography by injecting contrast media and a small volume of air into the right pelvocaliceal system. The total volume of air injected through the operation was about 25 mL. Six hours after the surgery, the patient complained of weakness of his right leg. He experienced a sudden tonic seizure and then became unconscious after 8 hours. Magnetic resonance imaging of the brain was negative. He recovered after 24 hours and became conscious. Transesophageal echocardiography showed air bubbles in the left atrium revealing that the patient had a right to left shunt due to the patent foramen oval. They concluded that the clinical manifestations were strongly suggestive of paradoxical air embolism.
Droghetti et al. [6] presented a similar case of paradoxical air emboli with an important difference: there was no report of air pyelography in that case. The authors presumed that the prone position of the case produced a considerable gravitational gradient along the right side of the heart and the renal pelvis. Hence, negative pressure could have drawn air into the open veins.
There were obvious predisposing factors related to the neurologic complications in the two cases in group C. Probable neurologic complications in such cases were seen in all procedure types. Therefore, it seems that these events may have no relationship to PCNL. We have no hypothesis to explain these phenomena following the PCNL procedure in the cases of group D.
Overall, we assume that these rare but devastating complications have multiple etiologies. In all of these cases, PCNL was performed with the patient under general anesthesia and in the prone position and with the use of room air to opacify the collecting system. Therefore, each of these factors could be presumed to be a cause of these complications. Use of the prone position in conjunction with compression on the abdomen can compromise the spinal cord perfusion and cause spinal cord ischemia. On the other hand, excessive head rotation and neck extension in the prone position, especially in patients with atherosclerotic vessels, may lead to a short-term mechanical occlusion of the vertebral or carotid artery, which can cause stasis, thrombi, and then embolism in the cerebrovascular system. The prone position produces a considerable gravitational gradient along the right side of the heart and the renal pelvis; thus, negative pressure could have drawn air into open veins. In these circumstances, injection of air potentially makes the patient at risk of air emboli that may be concomitant with neurological complications in the presence of a patent foramen oval.
Conversely, most of the PCNL procedures in Iran are performed with the patient under general anesthesia in the prone position, and iodinated contrast materials are the most widely used means of opacifying the collecting system. There were no reports of neurologic complications in cases with contrast agent instillation for opacifying the collecting system; all of these complications happened after injection of room air. There were also no reports of neurologic complications following PCNL procedures performed with the patient under spinal anesthesia or in the supine position. Consequently, it can be assumed that the use of room air to opacify the collecting system plays a major role in the occurrence of these complications and, likewise, that the prone position and general anesthesia may predispose to these events in the presence of air injection.
This article is a descriptive study and was designed to introduce vigilance. Endourologists should pay attention to these complications and properly assess for predisposing factors. We do not claim that the aforementioned etiologies are the main causes of neurologic complications, because recognition of the original causes requires more comprehensive evaluation between advanced referral centers in different countries.
CONCLUSIONS
To avoid neurologic complications in PCNL, we recommend the following:
1) Use of air during PCNL should be limited if not abandoned.
2) Use of spinal anesthesia and the supine position in simple cases are recommended if possible.
3) Use of a frame that prevents abdominal compression and perioperative hypotension to maintain sufficient spinal cord perfusion during and after the surgery is suggested.
4) Excessive head rotation and neck extension in the prone position should be avoided.
Footnotes
The authors have nothing to disclose.
References
- 1.Fernstrom I, Johansson B. Percutaneous pyelolithotomy: a new extraction technique. Scand J Urol Nephrol. 1976;10:257–259. doi: 10.1080/21681805.1976.11882084. [DOI] [PubMed] [Google Scholar]
- 2.Vicentini FC, Gomes CM, Danilovic A, Neto EA, Mazzucchi E, Srougi M. Percutaneous nephrolithotomy: current concepts. Indian J Urol. 2009;25:4–10. doi: 10.4103/0970-1591.44281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Miller RA, Kellett MJ, Wickham JE. Air embolism, a new complication of percutaneous nephrolithotomy. What are the implications? J Urol (Paris) 1984;90:337–339. [PubMed] [Google Scholar]
- 4.Hobin FP. Air embolism complicating percutaneous ultrasonic lithotripsy. J Forensic Sci. 1985;30:1284–1286. [PubMed] [Google Scholar]
- 5.Song SH, Hong B, Park HK, Park T. Paradoxical air embolism during percutaneous nephrolithotomy: a case report. J Korean Med Sci. 2007;22:1071–1073. doi: 10.3346/jkms.2007.22.6.1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Droghetti L, Giganti M, Memmo A, Zatelli R. Air embolism: diagnosis with single-photon emission tomography and successful hyperbaric oxygen therapy. Br J Anaesth. 2002;89:775–778. [PubMed] [Google Scholar]
- 7.Varkarakis J, Su LM, Hsu TH. Air embolism from pneumopyelography. J Urol. 2003;169:267. doi: 10.1016/S0022-5347(05)64084-0. [DOI] [PubMed] [Google Scholar]
- 8.Bhardwaj A, Long DM, Ducker TB, Toung TJ. Neurologic deficits after cervical laminectomy in the prone position. J Neurosurg Anesthesiol. 2001;13:314–319. doi: 10.1097/00008506-200110000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Langmayr JJ, Ortler M, Obwegeser A, Felber S. Quadriplegia after lumbar disc surgery. A case report. Spine (Phila Pa 1976) 1996;21:1932–1935. doi: 10.1097/00007632-199608150-00021. [DOI] [PubMed] [Google Scholar]
- 10.Turker RJ, Slack C, Regan Q. Thoracic paraplegia after lumbar spinal surgery. J Spinal Disord. 1995;8:195–200. doi: 10.1097/00002517-199506000-00003. [DOI] [PubMed] [Google Scholar]


