Abstract
Gaseous molecules continue to hold new promise in molecular medicine as experimental and clinical therapeutics. The low molecular weight gas carbon monoxide (CO), and similar gaseous molecules (e.g., H2S, nitric oxide) have been implicated as potential inhalation therapies in inflammatory diseases. At high concentration, CO represents a toxic inhalation hazard, and is a common component of air pollution. CO is also produced endogenously as a product of heme degradation catalyzed by heme oxygenase enzymes. CO binds avidly to hemoglobin, causing hypoxemia and decreased oxygen delivery to tissues at high concentrations. At physiological concentrations, CO may have endogenous roles as a signal transduction molecule in the regulation of neural and vascular function and cellular homeostasis. CO has been demonstrated to act as an effective anti-inflammatory agent in preclinical animal models of inflammation, acute lung injury, sepsis, ischemia/reperfusion injury, and organ transplantation. Additional experimental indications for this gas include pulmonary fibrosis, pulmonary hypertension, metabolic diseases, and preeclampsia. The development of chemical CO releasing compounds constitutes a novel pharmaceutical approach to CO delivery with demonstrated effectiveness in sepsis models. Current and pending clinical evaluation will determine the usefulness of this gas as a therapeutic in human disease.
Keywords: Acute lung injury, Carbon monoxide, Heme oxygenase (decyclizing), Reperfusion injury, Sepsis
INTRODUCTION
Over the last two decades, gaseous molecules have joined the ranks of experimental therapeutics with potential applications in the treatment of pulmonary or systemic diseases. The principle advantage of gases in therapy is in their mode of administration (i.e., inhalation), which is practical for clinical use and noninvasive [1]. Gases which have known medical applications include a number of low molecular weight substances (e.g., H2, O2, N2O, CO2, He, Xe, N2, O3) [2,3]. In addition to these, three gases have gained widespread attention as novel therapeutics with anti-inflammatory and vasoregulatory properties: nitric oxide (NO) [4,5], carbon monoxide (CO) [5-11], and hydrogen sulfide (H2S) (Table 1; for chemical physical properties of these gases) [5,12-16]. In addition to their presence as ubiquitous contaminants of indoor and outdoor air, these three gases share an important similarity in that they are all produced in the body as the natural products of enzymatic reactions (Table 2) [13-15,17-23].
Table 1.
Chemical and physical properties of the medicinal gases
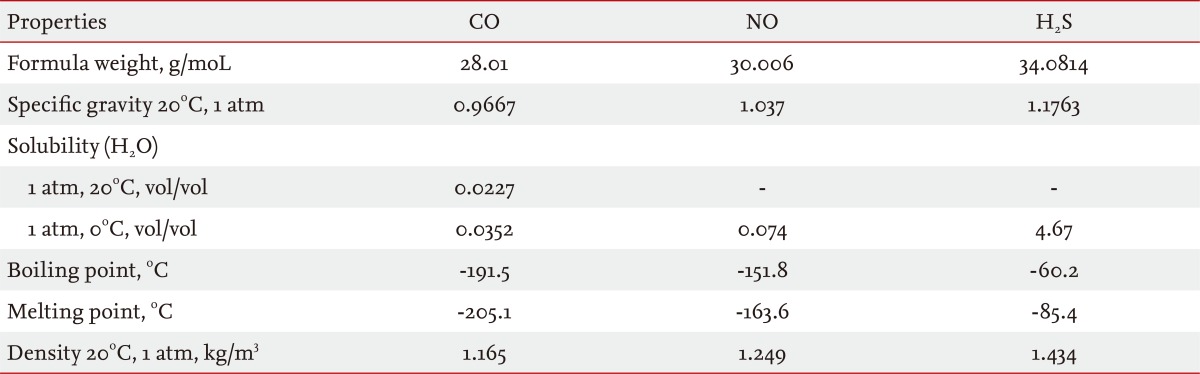
CO, carbon monoxide; NO, nitric oxide; H2S, hydrogen sulfide.
Table 2.
Enzymatic generation of small gaseous mediators
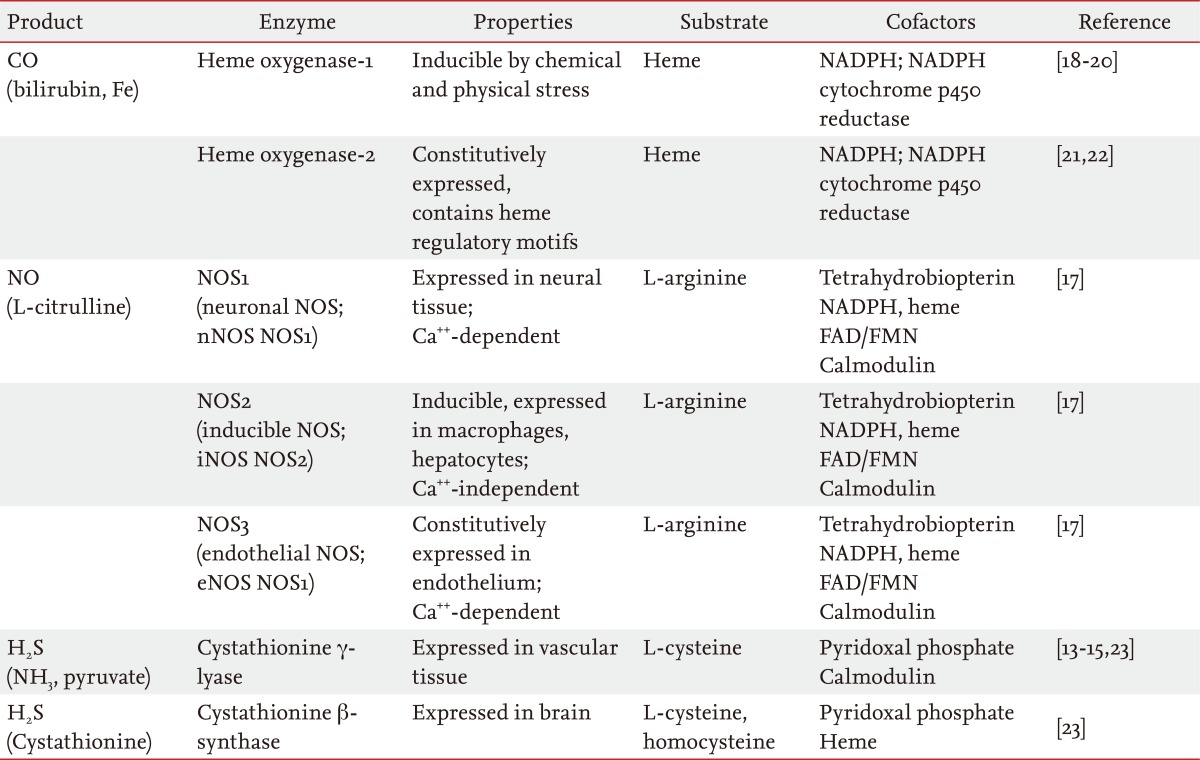
CO, carbon monoxide; NADPH, nicotinamide adenine dinucleotide phosphate; NO, nitric oxide; NOS, nitric oxide synthase; FAD, flavin adenine dinucleotide; FMN, flavin mononucleotide; H2S, hydrogen sulfide.
The recognition that gases could exert physiological functions began with the identification of NO as an endogenously-produced regulator of vasodilatation and vascular cell proliferation [24-26]. These effects of NO are mediated by the binding of this gas to the heme moiety of soluble guanylate cyclase (sGC), which stimulates the production of 3',5'-cyclic guanosine monophosphate (cGMP) [27-29]. NO is a reactive free radical that can participate in oxygen and metal-dependent redox reactions, which arises as the product of constitutive and inducible nitric oxide synthase (NOS) enzymes [17]. Inhaled NO, which acts as a selective pulmonary vasodilator [30,31], has been investigated for its therapeutic potential in several diseases including acute respiratory distress syndrome and pulmonary hypertension [31-33].
CO, a diatomic low molecular weight gas, shares similarities with NO in terms of molecular size and structure [34]. CO however, is a relatively stable non-radical gas that typically reacts in biological systems with metal centers of hemoproteins [35]. The endogenous production of CO as the natural product of hemoglobin turnover has been recognized since the middle of the twentieth century [36-38]. However the production of CO in biological systems was previously regarded by the scientific community as a metabolic elimination product. In 1968 to 1969, the heme oxygenase (HO) enzyme system responsible for the catalytic turnover of heme, was characterized and identified as a major source of CO in the body [18,19,39]. The inducible form of this enzyme, HO-1, was identified as identical to the major 32 to 34 kDa stress protein responsive to xenobiotic stress [20,40]. Importantly, further studies established an association between the heme metabolic pathway and the cellular stress response involving HO-1, which contributes to cellular adaptation to toxic environmental challenges [20,41,42]. Subsequent investigations sought to determine the physiological function of endogenously produced CO, as well as its role as a mediator of the cytoprotective properties of HO-1 [7,43-46]. Although many investigations have employed exogenous CO at low concentration, they revealed an impact of this gas on intracellular signaling pathways [43-46]. These studies identified new roles of CO on the regulation of several fundamental biological processes, including vascular tone [47,48], inflammation [43], neurotransmission [44], cell proliferation [49], programmed cell death [45], mitochondrial biogenesis [50], and autophagy [51].
The current prospective status of CO as an inhaled therapeutic is based on extensive preclinical animal testing: reviewed in references [7,11], in models of acute lung injury (ALI) [52-54], ischemia/reperfusion (I/R) injury [55,56], sepsis [57], vascular injury, organ transplantation [58-60]; and others, reviewed in references [5-7,61]. Protective effects of CO have been attributed to several mechanisms, including the regulation of inflammation and innate immune responses, apoptosis, as well as effects on microcirculation and cellular redox balance [5-7,11].
In addition to NO and CO, a third endogenously-produced gaseous molecule H2S has recently emerged as a physiological mediator and candidate therapeutic agent [12-16,62]. H2S which induces a suspended animation-like state in rodents can exert effects on the regulation of vascular tone, inflammation, myocardial contractility, neurotransmission, and insulin secretion [62-66]. H2S has been demonstrated to confer anti-inflammatory properties in several preclinical models, including ALI, and sepsis [67-69].
This review will focus primarily on the therapeutic potential of CO, with an emphasis on mechanistic studies and preclinical animal studies in models of ALI, sepsis, and organ transplantation, as well as its future prospect for clinical use. The pharmacological application of CO in therapy through the use of donor compounds will also be discussed [11]. The reader is referred to other reviews for recent perspectives on the therapeutic potential of NO [4,5], H2S [13,62] and of the other clinically relevant gases [3].
ENVIRONMENTAL AND CLINICAL TOXICOLOGY OF CO EXPOSURE
Environmental CO occurs in the atmosphere from man-made and natural sources, as a by-product of organic combustion. CO is a toxic inhalation hazard, and a common contaminant of indoor and outdoor air [70]. Environmental CO arises primarily as the product of the incomplete oxidation of fossil fuels (e.g., wood, coal, kerosene, and natural gas), and is present at high concentrations in automobile exhaust and tobacco smoke [70].
Indoor levels of CO range from 0.5 to 5 parts per million (ppm) but may reach much higher values (e.g., 100 ppm) with inefficient heating or ventilation, or in the presence of environmental tobacco smoke [71]. In urban areas, ambient levels are typically 20 to 40 ppm, but may peak at much higher levels in heavily congested areas or alongside highways [72].
Inhaled CO diffuses rapidly across alveolar and capillary membranes, with the majority forming a tight binding complex with the oxygen carrier protein hemoglobin to form carboxyhemoglobin (COHb), with a binding affinity for hemoglobin approximately 200 to 250 times that of oxygen [70,73,74]. Partial occupation of CO at the O2 binding sites of hemoglobin inhibits the release of O2 from the remaining heme groups. These effects of CO impair the capacity of the blood to deliver O2, leading to tissue hypoxia [70,73]. The formation of COHb is reversible by removal of the CO source in favor of O2 inspiration. Thus, oxygen therapy is a common antidote for CO poisoning [74,75]. The basal COHb level in man is ~0.1% to 1% in the absence of environmental contamination or smoking. Habitation of heavily populated urban areas with high levels of ambient CO, such as originating from automobile exhaust, or smoking, may increase this background [76,77].
COHb levels of greater than 20% are typically associated with symptoms of clinical toxicity. Acute signs of CO poisoning include dizziness, shortness of breath, and headache. Elevated or chronic exposures may lead to neurotoxicity, cognitive impairment, visual impairment, and unconsciousness, with death occurring in the range of 50% to 80% COHb [74,75]. Recent studies have also identified chronic exposure to elevated ambient CO as a cardiovascular risk factor [78]. The proposed mechanisms for cardiotoxicity associated with chronic low level exposure have been reviewed elsewhere [79].
Although hemoglobin represents the primary systemic target of CO, a direct toxicity of CO has also been described, associated with impaired functioning of cellular hemoprotein targets (e.g., myoglobin, cytochrome c oxidase and cytochrome p450), resulting in the impairment of respiration and other metabolic functions. However, the contribution of these additional cellular and tissue targets to systemic toxicity, usually associated with hypoxemia, remains unclear [74].
THE HO ENZYME SYSTEM: A SOURCE OF BIOLOGICAL CO
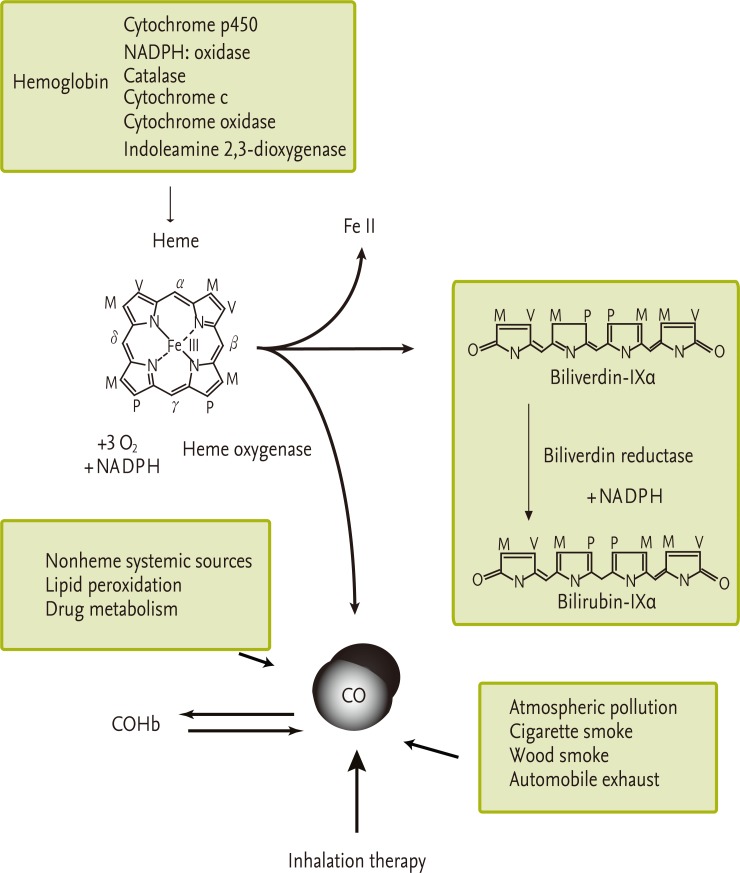
The majority of endogenously produced CO (estimated at 85%) arises as the natural product of heme degradation, most of which originates systemically from hemoglobin turnover (Fig. 1) [36-38]. However, the heme pool subject to degradation may also originate from the turnover of other cellular hemoproteins in which it is utilized as cofactor, including cytochrome p450 and other cytochromes [21,80]. Heme is degraded enzymatically by the HOs (EC 1:14:99:3) [18,19,21]. The HO enzymes catalyze the oxidative cleavage of heme at the α-methene bridge carbon atom, to generate biliverdin-IXα, ferrous iron and CO. The HO reaction requires three moles of molecular oxygen for each heme molecule oxidized, and electrons from nicotinamide adenine dinucleotide phosphate (NADPH) cytochrome p450 reductase [19]. Bilirubin-IXα is reduced to biliverdin-IXα by NADPH: biliverdin reductase [81]. Although the HO reaction represents the major enzymatic source of CO, a minor component of endogenous CO may also arise from poorly defined nonheme sources. CO may arise as a by-product of lipid oxidation or as the product of cytochrome p450-dependent metabolism of xenobiotics (e.g., methylene chloride) [82].
Figure 1.
Sources of biological carbon monoxide (CO). CO is naturally produced in the human body, primarily as the product of the turnover of hemoglobin and cellular hemoproteins. Heme, which is used as a prosthetic cofactor for hemoproteins, is degraded by the heme oxygenase (HO) (EC 1:14:99:3) enzyme system. HO catalyzes the rate limiting step in heme degradation, to generate biliverdin-IXα, CO, and ferrous iron (Fe II), and requires 3 mol molecular oxygen and nicotinamide adenine dinucleotide phosphate (NADPH). Biliverdin-IXα produced in the HO reaction is reduced to bilirubin-IXα by biliverdin reductase (side chains are labeled as M, methyl; V, vinyl; P, propionate). Nonheme sources may make a minor contribution to exogenous CO production. In the blood, CO binds hemoglobin to form carboxyhemoglobin (COHb). CO may also be inhaled with ambient air, in the context of smoking, accidental or occupational exposure, or as a component of therapy, as discussed in this review.
HOs consist of two major isozymes (HO-1 and HO-2), each the product of distinct genes [21,22,83]. The constitutive isozyme HO-2 is expressed in most tissues, with particular abundance in testis and brain tissue [21]. HO-1, the inducible isozyme, represents a major cellular and tissue homeostatic response to environmental stress signals [20]. HO-1 expression responds to many diverse chemical and physical stimuli, including the natural enzymatic substrate heme, a pro-oxidant compound, oxidants (e.g., H2O2), heavy metals and thiol (SH)-reactive substances, natural antioxidants, deviations in ambient oxygen tension, as well as heat shock (in rodents) [7,20,41,42,84-87]. The induction of HO-1 is mediated primarily by transcriptional regulation [87,88]. The mouse HO-1 (hmox-1) gene 5' regulatory region contains two upstream enhancers occurring at -4 and -10 kb relative to the transcriptional start site [89,90]. These enhancers contain sequences homologous to the antioxidant responsive element (ARE) [89,90]. The NF-E2-related factor-2 (Nrf2) represents the major transcriptional regulator of hmox-1 in response to many inducing stimuli [91,92]. Following cellular stimulation, Nrf2 migrates to the nucleus where it recognizes ARE binding sites in the hmox-1 promoter [93]. Nrf2 is inactivated by a cytoplasmic anchor, Keap-1 [93,94], and antagonized in the nucleus by a heme-sensitive transcriptional repressor, Bach-1 [95,96]. Additionally, a number of diverse transcriptional regulators can regulate hmox-1 in a cell-type and inducer-specific fashion [97,98]. These include hypoxia-inducible factor-1, heat shock factor-1 (HSF-1), activator protein-1, early growth response factor-1 (Egr-1), nuclear factor kappa-B (NF-κB), and others [7,84,97,98].
CO AS AN EFFECTOR OF INTRACELLULAR SIGNAL TRANSDUCTION PATHWAYS
Despite the known toxicity of CO at high concentration, recent research has revealed that low concentrations of CO may influence intracellular signal transduction pathways. CO can exert vasoregulatory properties [47], as well as modulate inflammation, apoptosis, and cell proliferation in vitro and in vivo [7,11,46].
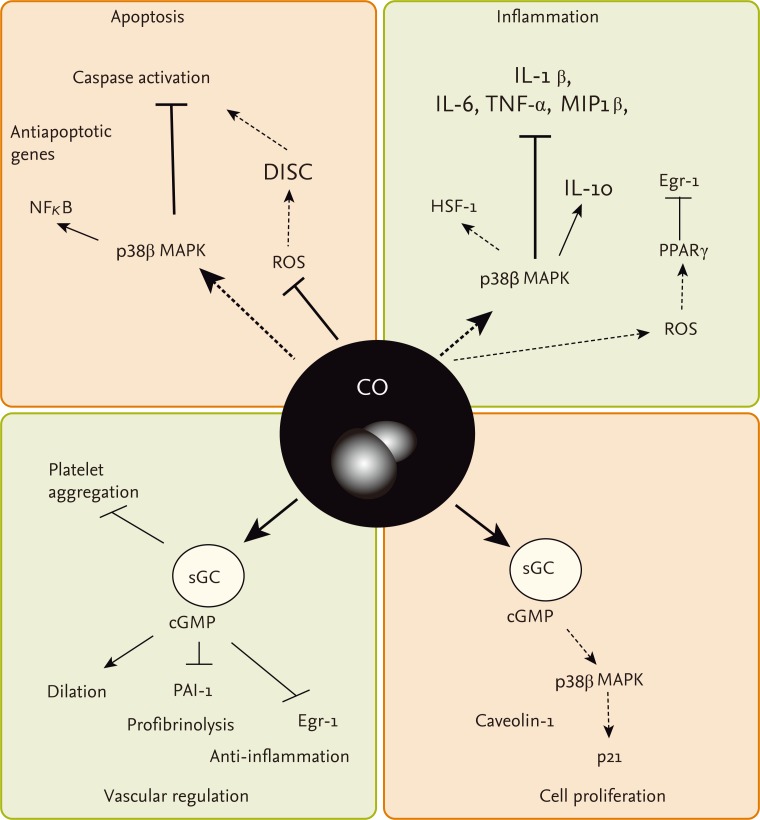
Cellular exposure to CO has been shown to directly or indirectly modulate the activity of several intracellular signaling molecules (Fig. 2). Similar to NO, CO can act as a heme-ligand and activator of sGC, to increase the production of cGMP [99]. Experimental evidence indicates that NO activates sGC in vitro and corresponding vasodilatory action in vivo with greater potency [100].
Figure 2.
Signaling pathways regulated by carbon monoxide (CO). CO can confer modulatory effects on the regulation of vascular function, inflammation, apoptosis, and cell proliferation, through stimulation of several signaling pathways. The sGC/cGMP axis has been implicated in vascular effects of CO with respect to vessel dilation, regulation of platelet aggregation, and regulation of fibrinolysis through PAI-1. The sGC/cGMP axis has also been implicated in downregulation of cell proliferation by CO, through upregulation of p38 mitogen activated protein kinase (MAPK) and p21Waf1/CIP1. Anti-inflammatory and antiapoptotic effects of CO, including downregulation of proinflammatory cytokines production are also thought to be mediated by p38 MAPK. Additional mechanisms involving the inhibition of cytosolic reactive oxygen species (ROS) may play a role in regulation of apoptosis through inhibiting death-inducing signal complex (DISC) formation. Stimulation of mitochondrial ROS may upregulate PPARγ leading to downregulation of the proinflammatory factor Egr-1. Additional signaling molecules such as heat shock factor-1 (HSF-1) and caveolin-1 have been shown to mediate the anti-inflammatory and antiproliferative effects of CO, respectively. IL, interleukin; TNF, tumor necrosis factor; MIP1, macrophage inflammatory protein 1; NF-κB, nuclear factor kappa-B; Egr, early growth response; PPAR, peroxisome proliferator-activated receptor; sGC, soluble guanylate cyclase; cGMP, cyclic guanosine monophosphate.
CO was first implicated as a regulator of the sGC/cGMP axis in the context of olfactory neurotransmission [44]. CO can exert vasorelaxant effects of CO in the liver and other vascular beds which are believed to be dependent of cGMP [47,48,101]. Alternatively, CO may also regulate vascular function through additional proposed mechanisms including inhibition of cytochrome p450, and the activation of calcium-dependent potassium channels Kca in vascular smooth muscle cells [102].
CO can modulate the activation of the mitogen activated protein kinases (MAPK), which are important mediators of inflammatory and stress responses [43,45,53,55,56]. A potent anti-inflammatory effect of CO was demonstrated in bacterial lipopolysaccharide (LPS)-stimulated macrophages, that depended on the modulation of mitogen activated protein kinase kinase-3 (MKK3)/p38 MAPK pathway [43]. The anti-inflammatory effects of CO also may depend on the downregulation of Toll-like receptor trafficking and activation, the inhibition of NADPH: oxidase dependent signaling [103], and additional signal transduction pathway molecules including HSF-1, and Egr-1/PPARγ [104,105].
CO has been shown to modulate apoptotic signaling pathways in cultured cells [45,55,56]. When applied at low concentration, CO inhibited cell death caused by proapoptotic agents (e.g., tumor necrosis factor-α [TNF-α]) in endothelial cells, which required the p38 MAPK pathway, and modulation of NF-κB signalling [106]. Additional targets for CO-dependent regulation of apoptosis in cells subjected to oxygen-dependent stress include the STAT3 and phosphatidylinositol-3-kinase/Akt pathways [107], downregulation of NADPH: oxidase dependent reactive oxygen species formation [108], and modulation of Fas-initiated extrinsic apoptotic pathways [55,108,109].
CO also has been shown to exert antiproliferative effects in vitro, with respect to the proliferation of vascular smooth muscle cells (SMCs) [49,110,111]. In SMC, both sGC/cGMP and p38 MAPK signaling pathways have been implicated in the antiproliferative effects of CO these cells [49,58,110,111].
Additional signaling mechanisms potentially involved in CO-dependent regulation of cell proliferation, include the regulation of the lipid-raft associated signaling protein caveolin-1 [112], and modulation of NADPH oxidase [113]. More recent studies have implicated the NOX1 isoform of NADPH oxidase in CO dependent inhibition of SMC migration [114]. Taken together, these modulatory effects of CO on the signal transduction pathways that culminate in the regulation of inflammation, apoptosis, cell proliferation, and vascular function all may contribute to the proposed therapeutic effects of this gas.
CO AS AN INHALATION THERAPEUTIC: PRECLINICAL STUDIES
The therapeutic benefit of CO inhalation has been shown in a number of preclinical animal models of lung and vascular disease, as outlined in the following sections.
Endotoxin challenge
Anti-inflammatory effects of CO have been demonstrated in a mouse model of endotoxin exposure [43]. CO preconditioning reduced the production of serum TNF-α, interleukin (IL)-1β, IL-6, whereas increased the production of the anti-inflammatory cytokine IL-10; reduced organ injury and prolonged survival following LPS challenge [43,115]. Anti-inflammatory effects of CO with respect to modulation of pro or anti-inflammatory cytokines production were diminished in HSF-1 knockout (hsf1-/-) mice, implicating a role of the heat shock response in vivo [104].
Anti-inflammatory effects of CO have been recently documented in higher mammals including swine. CO reduced the development of disseminated intravascular coagulation and inhibited serum levels of the proinflammatory IL-1β in response to LPS, while inducing the anti-inflammatory cytokine IL-10 after LPS challenge [116]. Similar, though less significant effects were noted in a nonhuman primate model of Cynomolgous macaques subjected to LPS challenge [117]. CO exposure (500 ppm, 6 hours) following LPS inhalation decreased TNF-α release in broncoalveolar lavage fluid (BALF), but had no apparent effect on IL-6 and IL-8 release, in addition to reducing pulmonary neutrophilia (not observed at lower concentrations of CO). This reduction of pulmonary neutrophilia was comparable to pretreatment with a well characterized inhaled corticosteroid budesonide. However, the therapeutic efficacy of CO required relatively high doses that resulted in elevated COHb levels (>30%). This work highlights the complexity of interspecies variation in lung responses to CO, and of dose-response relationships of CO to COHb levels and anti-inflammatory effects [117]. This study was the first to examine the therapeutic index and dose-response relationships of CO therapy in nonhuman primates [117].
ALI
Low doses of CO have been shown to provide protection against ALI in rodent models. The administration of CO (250 ppm) during hyperoxia exposure prolonged the survival of rats and mice subjected to a lethal dose of hyperoxia, and dramatically reduced histological indices of lung injury, including airway neutrophil infiltration, fibrin deposition, alveolar proteinosis, pulmonary edema, and apoptosis, relative to animals exposed to hyperoxia without CO [52,53]. In mice, hyperoxia was shown to induce the expression of proinflammatory cytokines (i.e., TNF-α, IL-1β, IL-6) and activate major MAPK pathways in lung tissue. The protection afforded by CO treatment against the lethal effects of hyperoxia correlated with the inhibited release of proinflammatory cytokines in the BALF. The protective effects of CO in this model were found to depend on the MKK3/p38β MAPK pathway [53]. It should be noted that some studies have reported negative findings with respect to protective effects of CO in rodent ALI models [118,119]. More recent studies report protective effects of HO-1 or CO in a model of hyperoxia-induced bronchopulmonary dysplasia in neonatal mice [120]. Lung specific transgenic overexpression of HO-1 alleviated hyperoxia-induced lung inflammation, edema, arterial remodeling, and right ventricular hypertrophy. Similar protective responses were elicited by intermittent CO inhalation in this model. However, neither CO nor HO-1 expression prevented alveolar simplification in this model [120].
Ventilator-induced lung injury (VILI)
The therapeutic potential of CO has been shown in a specialized clinically-relevant model of VILI [54,121-123]. Rats ventilated with an injurious (high tidal volume) ventilator setting in combination with LPS injection, exhibited lung injury. The inclusion of CO (250 ppm) during mechanical ventilation reduced the inflammatory cell infiltration in BALF. In the absence of cardiovascular effects, CO dose-dependently decreased TNF-α and increased IL-10 in the BALF [54]. CO application has also been reported to confer tissue protection in a mouse model of VILI, at moderate tidal volume ventilation [121-123]. In this model, mechanical ventilation caused significant lung injury reflected by increases in protein concentration, total cell and neutrophil counts in BALF. CO reduced mechanical ventilation-induced cytokine and chemokine production and prevented lung injury during ventilation, involving the inhibition of mechanical ventilation-induced increases in BALF protein concentration and cell count, lung neutrophil recruitment, and pulmonary edema [121-123]. To date, these effects of CO were associated with the activation of caveolin-1 [121], activation of PPARγ, and the inhibition of Egr-1 signaling [122]. These studies, taken together, suggest that mechanical ventilation in the presence of CO may provide protection in animal models of VILI. However, more studies are required to determine the exact mechanisms underlying the therapeutic potential of CO in VILI models.
Organ ischemia reperfusion injury and transplantation
Tissue protective effects of CO have been shown experimentally in rodent models of organ I/R injury. Lung I/R caused by occlusion of the pulmonary artery causes lung apoptosis, involving caspase activation, expression changes in Bcl2 family proteins, cleavage of PARP, and mitochondrial cytochrome c release [55]. CO conferred tissue protection in rodents subjected to lung I/R injury, as evidenced by reduced markers of apoptosis, which depended on activation of the MKK3/p38α MAPK pathway [56]. In vivo studies using homozygous HO-1 knockout mice (hmox-1-/-) demonstrated that HO-1 deficiency conferred sensitivity to the lethal effects of lung I/R injury. Application of exogenous CO by inhalation compensated for the HO-1 deficiency in hmox-1-/- mice, and improved survival during pulmonary I/R [124]. The protection provided by CO involved activation of fibrinolysis. This effect of CO depended on activation of the sGC/cGMP axis, and downstream inhibition of plasminogen activator inhibitor-1, a macrophage-derived activator of SMC proliferation [124]. CO also inhibited fibrin deposition and improved circulation in ischemic lungs [125], involving the downregulation of the proinflammatory transcription factor Egr-1 [125]. Recent studies in a retinal I/R injury model, suggest that postinjury application of CO can inhibit injury of retinal ganglion cells through antiapoptotic and anti-inflammatory effects [126].
In organ transplantation models, I/R injury subsequent to transplantation, may play a major role in graft failure. In this regard, CO has been intensively studied as an anti-inflammatory therapeutic in experimental organ transplantation. CO has a demonstrated potential for reducing transplant associated I/R injury and also reducing the probability of graft rejection when applied at low concentration, as an adjuvant to organ preservation fluid or when applied to donors and/or recipients in gaseous form at low concentration. The application of CO has now been shown to confer protection during transplantation of several organs, including vascular tissue [58], heart [59], small intestine [127], kidney, [128], liver [129], and lung [60,130,131]. During orthotopic left lung transplantation in rats, exogenous application of CO (500 ppm), significantly protected the graft, and reduced hemorrhage, fibrosis, and thrombosis after transplantation [60]. Furthermore, CO inhibited lung cell apoptosis and downregulated lung and systemic proinflammatory cytokine production which were induced during transplantation [60]. Furthermore, protection against I/R injury was conferred in syngeneic rat orthotopic lung transplantation by inhaled CO administered to either the donor or the recipient [130]. Delivery of CO to lung grafts by saturation of the preservation media reduced I/R injury and inflammation in syngeneic rat orthotopic lung transplantation [131]. In a vascular transplantation model, when transplant recipients of aortic grafts were maintained in a CO environment (250 ppm) with preconditioning, these animals displayed reduced intimal hyperplasia, and reduced leukocyte, macrophage, and T cell infiltration in the graft [58]. Saturation of the organ buffer with CO gas also prevented cold I/R injury during subsequent intestinal transplantation [132]. The inhibition of apoptosis and inflammation may represent the primary mechanisms by which CO protects transplanted organs from dysfunction and failure [133], though improvement of blood circulation by CO within the reperfused transplanted organ [58,133,134], as well as antiproliferative [58] effects may contribute.
Pulmonary hypertension
Pulmonary arterial hypertension (PAH) is a terminal disease characterized by a progressive increase in pulmonary vascular resistance leading to right ventricular failure. Several previous studies have demonstrated that HO-1 expression can exert a protective effect in animal models of pulmonary hypertension, and in the regulation of hypoxic pulmonary vasoconstriction [135-137]. Administration of CO was shown to provide protection in rodent models of monocrotaline-induced and hypoxia-induced PAH. Exposure to CO (1 hr/day) reversed established PAH and right ventricular hypertrophy, restored right ventricular and pulmonary arterial pressures, as well as pulmonary vascular morphology, to that of controls. The ability of CO to reverse PAH was dependent on endothelial NOS3 and NO generation, since CO failed to reverse chronic hypoxia-induced PAH in mice genetically deficient for eNOS (nos3-/-). The protective effect of CO was endothelial cell-dependent, and associated with increased apoptosis and decreased cellular proliferation of vascular SMCs [138]. Additional studies have shown that CO decreased pulmonary artery vascular resistance and inhibited hypoxic vasoconstriction, through activation of the sGC/cGMP, and the hyperpolarization of potassium channels [139].
Fibrotic lung disease
Idiopathic pulmonary fibrosis (IPF) is a terminal disease characterized by scarring or thickening of lung tissues associated with fibroblast hyperproliferation and extracellular matrix remodeling with no known etiology or effective treatment [140]. IPF affects primarily the lower respiratory tract resulting in compromised efficiency of alveolar gas exchange [140]. Bleomycin, a redox cycling compound that generates O2- and H2O2, causes lesions in mouse lung after intratracheal administration, is used to model IPF in animals. Exogenous CO treatment can provide protection against bleomycin-induced fibrotic lung injury in mice [141]. In mice treated with bleomycin intratracheally and then exposed to CO or ambient air, the lungs from CO-treated animals displayed reduced lung hydroxyproline, collagen, and fibronectin levels relative to air-treated bleomycin-injured controls. The protective effect of CO in this model was associated with an anti-proliferative effect of CO on fibroblast proliferation associated with the increased expression of p21Waf1/Cip1 and inhibition of cyclins A/D expression [141].
Diabetes and metabolic syndrome
To date, only few studies have examined the direct therapeutic effects of CO in diabetes-related models. Diabetic gastroparesis is a condition where gastric emptying time is delayed, which is associated with increased oxidative stress, and injury to interstitial cells of Cajal in the stomach [142]. Nonobese diabetic mice with a gastric delay phenotype were subjected to inhaled CO therapy (100 ppm, 8 hr/day for 16 days), which reduced serum oxidative stress markers, restored expression of Kit, a marker of interstitial cells of Cajal, and ameliorated gastric delay in this model [143]. Similar effects were previously observed in this model with HO-1 overexpression [142]. Previous studies have suggested an antioxidative role for CO (administered as donor compound) in preventing hyperglycemia-induced endothelial cell sloughing in streptozotocin-induced diabetes [144].
In a type 1 diabetes models, ex vivo treatment of dendritic cells with gaseous CO was shown to augment dendritic-cell based therapy. Application of CO-conditioned dendritic cells was shown to effectively impair the accumulation and pathogenic activity of autoreactive CD8+ T cells in the pancreas [145].
CO exposure inhibited apoptosis in cultured pancreatic β-cells exposed to proapoptotic stimuli, through activation of the sGC/cGMP axis [146]. Similar to results reported in other transplantation models, CO preconditioning of mouse islets or treatment of donors improved viability and reduced graft rejection during allogeneic islet transplantation [146,147].
In models of metabolic disease, inhalation of CO gas reduced hepatic steatosis in mice subjected to 30% fructose or methionine-deficient and choline-deficient diets [148]. CO exposure (administered as donor compound) was shown to confer cardioprotection and restore mitochondrial function in a high fat diet induced model of metabolic syndrome [149]. Taken together, these studies are suggestive of a potential for CO therapy of metabolic disorders, though further investigation is needed.
Preeclampsia
Preeclampsia is a condition associated with pregnancy involving abnormal placentation, hypertension, and proteinuria. Although the condition is thought to involve increased oxidative stress in the placental circulation, women who smoke during pregnancy have a significantly reduced risk of developing this condition [150]. Previous studies have suggested that deficiency in the HO-1/CO system may be associated with placental dysfunction and susceptibility to preeclampsia [151]. HO-1 expression was found to be reduced in placenta from pregnancies complicated by preeclampsia [151]. Consistently, blood COHb levels were found to be significantly lower in women with preeclampsia compared with normal pregnancies [152]. Ex vivo application of CO to placental villous extracts reduced I/R associated apoptosis in the syncytiotrophoblast layer [153]. Intriguingly, recent clinical studies have described ambient CO as an inverse risk factor for preeclampsia. Maternal exposure to moderate ambient CO was associated independently with a decreased risk of preeclampsia [154]. Current views implicate the HO-1/CO system as an essential procirculatory factor in the placenta, though more studies are needed.
PHARMACOLOGICAL APPLICATION OF CO USING DONOR COMPOUNDS
As an alternative approach to the administration of CO gas by inhalation, chemical CO-donor compounds termed carbon monoxide releasing compounds (CORMs) have been developed as experimental therapeutics over the last decade [11].
Several prototypical CORMs have been extensively tested in experimental models, including the original Mn2CO10 (CORM-1) and the ruthenium compounds tricarbonyldichlororuthenium-(II)-dimer (CORM-2) and tricarbonylchoro (glycinato)-ruthenium (II) (CORM-3) [155,156].
CORM-1 and CORM-2 are hydrophobic, while CORM-3 is water-soluble and rapidly releases CO in physiological fluids. A water-soluble boron-containing CORM (CORM-A1) has also been developed, which slowly releases CO in a pH and temperature-dependent fashion [157]. A new CORM (CORM-S1) based on iron and cysteamine has recently been synthesized, which is soluble in water and releases CO under irradiation with visible light, while it is stable in the dark [158]. Micellar forms of metal carbonyl complexes have been developed that display slower kinetics of CO release and enhanced ability to target distal tissue drainage sites [159]. Furthermore, novel hydrophobic and hydrophilic CORMs based on iron carbonyls have been recently described [160].
CORMs have demonstrated vasoactive effects with CORM-3 shown to produce a rapid vasodilatory response [161]. Similar to inhalation CO, cytoprotective effects have been obtained in various injury and disease models with pharmacological application of CORMs. CORMs can be used to deliver small amounts of CO to biological systems in a controlled manner and are emerging as an experimental therapy for sepsis and inflammatory disorders. An advantage of CORMs is that they deliver CO to tissues with less COHb buildup typical of inhalation CO [11].
CORMs have been shown to inhibit proinflammatory cytokine production in LPS-stimulated macrophages [162], and decrease the inflammatory response and oxidative stress in LPS-stimulated endothelial cells [163]. In vivo, CORMs attenuate systemic inflammation and proadhesive vascular cell properties in septic and thermally injured mice by reducing nuclear factor-κB activation, protein expression of ICAM-1, and tissue granulocyte infiltration [164,165]. CORM-3 has been shown to prevent reoccurrence of sepsis, CORM-2 prolongs survival and reduces inflammation and CORM-3 reduces liver injury after CLP [165,166]. Recent studies on the protective effects of CORMs in murine sepsis were related to stimulation of mitochondrial biogenesis through the Nrf2/Akt axis [167]. Furthermore, in cardiac transplantation model, inclusion of CORM-3 in the preservation fluid improved cardiac function following transplantation [168].
These studies taken together have demonstrated that the CORM dependent release of CO can confer protection in models of inflammation and sepsis, suggesting that CORMs could be used therapeutically to prevent organ dysfunction and death in sepsis.
CO AS AN INHALATION THERAPEUTIC: CLINICAL STUDIES
To date, inhalation CO has been administered to humans in but a few published experimental studies. CO inhalation was administered to healthy human subjects to examine systemic inflammation during experimental endotoxemia. In a randomized, double-blinded, placebo-controlled, two-way cross-over trial, experimental endotoxemia was induced in healthy volunteers by injection of 2 ng/kg LPS. The potential anti-inflammatory effects of CO inhalation were investigated by inhalation of 500 ppm CO (associated with an increase in COHb from 1.2% to 7%) versus synthetic air as a placebo for 1 hour. In this study, CO inhalation had no effect on the inflammatory response as measured by systemic cytokine production (TNF-α, IL-6, IL-8, IL-1α, and IL-1β), although no adverse side effects of CO inhalation were observed [169]. However, given the limited scope of this initial trial, and the protective characteristics of CO application in many animal models of sepsis, further more detailed clinical trials are required to reach a verdict on the efficacy of CO for reducing inflammation in septic patients. In contrast, a recent clinical study demonstrates the feasibility of administering inhaled CO to humans with COPD [170]. In this study, exsmoking patients with stable COPD were subjected to CO inhalation (100 to 125 ppm for 2 hr/day for 4 days), which increased COHb levels to 4.5%. Inhalation of CO by patients with stable COPD led to trends in reduction of sputum eosinophils and improvement of methacholine responsiveness [170].
CONCLUSIONS
Gaseous molecules continue to show future promise as they join the armamentarium of experimental and clinical therapeutics. Among the known medical gases, CO inhalation has been demonstrated to have potential applications in pulmonary diseases and other inflammatory diseases. To date, salutary effects of CO have been demonstrated in a number rodent model studies, though recent studies have attempted to recapitulate findings in larger animals such as monkeys and swine [5,7,116,117]. Differences in lung physiological responses to CO between rodents, large animals (e.g., nonhuman primates) and humans require further investigation. Additional studies will be required to confirm the safety and efficacy of CO inhalation as a treatment for inflammatory lung diseases. Pharmacological application of CO using CORM technology provides an attractive alternative to inhalation gas [11]. However, further understanding of the pharmacokinetics and toxicological responses of CORMs, including hemodynamic effects, must be achieved before employing CORMs as clinical therapy. The effectiveness of inhaled CO as a therapeutic in human diseases including sepsis, renal transplantation, pulmonary fibrosis, and pulmonary hypertension, awaits the outcome of additional planned preclinical testing and clinical trials. The next decade should yield a resolution on the feasibility and efficacy of exploiting the therapeutic index of CO in human disease.
Acknowledgments
This work was funded by NIH grants P01 HL108801 and R01 HL079904 to A.M.K. Choi. S.W. Ryter received additional salary support from the Brigham and Women's Hospital and Lovelace Respiratory Research Institute Consortium for Lung Research.
Footnotes
No potential conflict of interest relevant to this article is reported.
References
- 1.Gentile MA. Inhaled medical gases: more to breathe than oxygen. Respir Care. 2011;56:1341–1357. doi: 10.4187/respcare.01442. [DOI] [PubMed] [Google Scholar]
- 2.Kashiba M, Kajimura M, Goda N, Suematsu M. From O2 to H2S: a landscape view of gas biology. Keio J Med. 2002;51:1–10. doi: 10.2302/kjm.51.1. [DOI] [PubMed] [Google Scholar]
- 3.Nakao A, Sugimoto R, Billiar TR, McCurry KR. Therapeutic antioxidant medical gas. J Clin Biochem Nutr. 2009;44:1–13. doi: 10.3164/jcbn.08-193R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bloch KD, Ichinose F, Roberts JD, Jr, Zapol WM. Inhaled NO as a therapeutic agent. Cardiovasc Res. 2007;75:339–348. doi: 10.1016/j.cardiores.2007.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ryter SW, Choi AM. Gaseous therapeutics in acute lung injury. Compr Physiol. 2011;1:105–121. doi: 10.1002/cphy.c090003. [DOI] [PubMed] [Google Scholar]
- 6.Ryter SW, Choi AM. Heme oxygenase-1/carbon monoxide: from metabolism to molecular therapy. Am J Respir Cell Mol Biol. 2009;41:251–260. doi: 10.1165/rcmb.2009-0170TR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ryter SW, Alam J, Choi AM. Heme oxygenase-1/carbon monoxide: from basic science to therapeutic applications. Physiol Rev. 2006;86:583–650. doi: 10.1152/physrev.00011.2005. [DOI] [PubMed] [Google Scholar]
- 8.Ryter SW, Morse D, Choi AM. Carbon monoxide: to boldly go where NO has gone before. Sci STKE. 2004;2004:RE6. doi: 10.1126/stke.2302004re6. [DOI] [PubMed] [Google Scholar]
- 9.Wu L, Wang R. Carbon monoxide: endogenous production, physiological functions, and pharmacological applications. Pharmacol Rev. 2005;57:585–630. doi: 10.1124/pr.57.4.3. [DOI] [PubMed] [Google Scholar]
- 10.Ryter SW, Otterbein LE. Carbon monoxide in biology and medicine. Bioessays. 2004;26:270–280. doi: 10.1002/bies.20005. [DOI] [PubMed] [Google Scholar]
- 11.Motterlini R, Otterbein LE. The therapeutic potential of carbon monoxide. Nat Rev Drug Discov. 2010;9:728–743. doi: 10.1038/nrd3228. [DOI] [PubMed] [Google Scholar]
- 12.Kashfi K, Olson KR. Biology and therapeutic potential of hydrogen sulfide and hydrogen sulfide-releasing chimeras. Biochem Pharmacol. 2013;85:689–703. doi: 10.1016/j.bcp.2012.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wagner F, Asfar P, Calzia E, Radermacher P, Szabo C. Bench-to-bedside review: hydrogen sulfide: the third gaseous transmitter: applications for critical care. Crit Care. 2009;13:213. doi: 10.1186/cc7700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu YH, Yan CD, Bian JS. Hydrogen sulfide: a novel signaling molecule in the vascular system. J Cardiovasc Pharmacol. 2011;58:560–569. doi: 10.1097/FJC.0b013e31820eb7a1. [DOI] [PubMed] [Google Scholar]
- 15.Wang R. Two's company, three's a crowd: can H2S be the third endogenous gaseous transmitter? FASEB J. 2002;16:1792–1798. doi: 10.1096/fj.02-0211hyp. [DOI] [PubMed] [Google Scholar]
- 16.Moody BF, Calvert JW. Emergent role of gasotransmitters in ischemia-reperfusion injury. Med Gas Res. 2011;1:3. doi: 10.1186/2045-9912-1-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wink DA, Mitchell JB. Chemical biology of nitric oxide: insights into regulatory, cytotoxic, and cytoprotective mechanisms of nitric oxide. Free Radic Biol Med. 1998;25:434–456. doi: 10.1016/s0891-5849(98)00092-6. [DOI] [PubMed] [Google Scholar]
- 18.Tenhunen R, Marver HS, Schmid R. The enzymatic conversion of heme to bilirubin by microsomal heme oxygenase. Proc Natl Acad Sci U S A. 1968;61:748–755. doi: 10.1073/pnas.61.2.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tenhunen R, Marver HS, Schmid R. Microsomal heme oxygenase: characterization of the enzyme. J Biol Chem. 1969;244:6388–6394. [PubMed] [Google Scholar]
- 20.Keyse SM, Tyrrell RM. Heme oxygenase is the major 32-kDa stress protein induced in human skin fibroblasts by UVA radiation, hydrogen peroxide, and sodium arsenite. Proc Natl Acad Sci U S A. 1989;86:99–103. doi: 10.1073/pnas.86.1.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maines MD. The heme oxygenase system: a regulator of second messenger gases. Annu Rev Pharmacol Toxicol. 1997;37:517–554. doi: 10.1146/annurev.pharmtox.37.1.517. [DOI] [PubMed] [Google Scholar]
- 22.Maines MD, Trakshel GM, Kutty RK. Characterization of two constitutive forms of rat liver microsomal heme oxygenase: only one molecular species of the enzyme is inducible. J Biol Chem. 1986;261:411–419. [PubMed] [Google Scholar]
- 23.Vandiver M, Snyder SH. Hydrogen sulfide: a gasotransmitter of clinical relevance. J Mol Med (Berl) 2012;90:255–263. doi: 10.1007/s00109-012-0873-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ignarro LJ, Buga GM, Wood KS, Byrns RE, Chaudhuri G. Endothelium-derived relaxing factor produced and released from artery and vein is nitric oxide. Proc Natl Acad Sci U S A. 1987;84:9265–9269. doi: 10.1073/pnas.84.24.9265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ignarro LJ, Byrns RE, Buga GM, Wood KS. Endothelium-derived relaxing factor from pulmonary artery and vein possesses pharmacologic and chemical properties identical to those of nitric oxide radical. Circ Res. 1987;61:866–879. doi: 10.1161/01.res.61.6.866. [DOI] [PubMed] [Google Scholar]
- 26.Moncada S, Palmer RM, Higgs EA. Nitric oxide: physiology, pathophysiology, and pharmacology. Pharmacol Rev. 1991;43:109–142. [PubMed] [Google Scholar]
- 27.Ignarro LJ. Nitric oxide: a unique endogenous signaling molecule in vascular biology. Biosci Rep. 1999;19:51–71. doi: 10.1023/a:1020150124721. [DOI] [PubMed] [Google Scholar]
- 28.Snyder SH, Bredt DS. Biological roles of nitric oxide. Sci Am. 1992;266:68–77. doi: 10.1038/scientificamerican0592-68. [DOI] [PubMed] [Google Scholar]
- 29.Derbyshire ER, Marletta MA. Structure and regulation of soluble guanylate cyclase. Annu Rev Biochem. 2012;81:533–559. doi: 10.1146/annurev-biochem-050410-100030. [DOI] [PubMed] [Google Scholar]
- 30.Ichinose F, Roberts JD, Jr, Zapol WM. Inhaled nitric oxide: a selective pulmonary vasodilator: current uses and therapeutic potential. Circulation. 2004;109:3106–3111. doi: 10.1161/01.CIR.0000134595.80170.62. [DOI] [PubMed] [Google Scholar]
- 31.Frostell C, Fratacci MD, Wain JC, Jones R, Zapol WM. Inhaled nitric oxide: a selective pulmonary vasodilator reversing hypoxic pulmonary vasoconstriction. Circulation. 1991;83:2038–2047. doi: 10.1161/01.cir.83.6.2038. [DOI] [PubMed] [Google Scholar]
- 32.Rossaint R, Falke KJ, Lopez F, Slama K, Pison U, Zapol WM. Inhaled nitric oxide for the adult respiratory distress syndrome. N Engl J Med. 1993;328:399–405. doi: 10.1056/NEJM199302113280605. [DOI] [PubMed] [Google Scholar]
- 33.Porta NF, Steinhorn RH. Pulmonary vasodilator therapy in the NICU: inhaled nitric oxide, sildenafil, and other pulmonary vasodilating agents. Clin Perinatol. 2012;39:149–164. doi: 10.1016/j.clp.2011.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hartsfield CL. Cross talk between carbon monoxide and nitric oxide. Antioxid Redox Signal. 2002;4:301–307. doi: 10.1089/152308602753666352. [DOI] [PubMed] [Google Scholar]
- 35.Piantadosi CA. Biological chemistry of carbon monoxide. Antioxid Redox Signal. 2002;4:259–270. doi: 10.1089/152308602753666316. [DOI] [PubMed] [Google Scholar]
- 36.Sjostrand T. The formation of carbon monoxide by the decomposition of haemoglobin in vivo. Acta Physiol Scand. 1952;26:338–344. doi: 10.1111/j.1748-1716.1952.tb00915.x. [DOI] [PubMed] [Google Scholar]
- 37.Sjostrand T. Endogenous production of carbon monoxide in man under normal and pathophysiological conditions. Scand J Clin Lab Invest. 1949;1:201–214. [Google Scholar]
- 38.Coburn RF, Blakemore WS, Forster RE. Endogenous carbon monoxide production in man. J Clin Invest. 1963;42:1172–1178. doi: 10.1172/JCI104802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tenhunen R, Marver HS, Schmid R. The enzymatic catabolism of hemoglobin: stimulation of microsomal heme oxygenase by hemin. J Lab Clin Med. 1970;75:410–421. [PubMed] [Google Scholar]
- 40.Kageyama H, Hiwasa T, Tokunaga K, Sakiyama S. Isolation and characterization of a complementary DNA clone for a Mr 32,000 protein which is induced with tumor promoters in BALB/c 3T3 cells. Cancer Res. 1988;48:4795–4798. [PubMed] [Google Scholar]
- 41.Keyse SM, Tyrrell RM. Both near ultraviolet radiation and the oxidizing agent hydrogen peroxide induce a 32-kDa stress protein in normal human skin fibroblasts. J Biol Chem. 1987;262:14821–14825. [PubMed] [Google Scholar]
- 42.Applegate LA, Luscher P, Tyrrell RM. Induction of heme oxygenase: a general response to oxidant stress in cultured mammalian cells. Cancer Res. 1991;51:974–978. [PubMed] [Google Scholar]
- 43.Otterbein LE, Bach FH, Alam J, et al. Carbon monoxide has anti-inflammatory effects involving the mitogen-activated protein kinase pathway. Nat Med. 2000;6:422–428. doi: 10.1038/74680. [DOI] [PubMed] [Google Scholar]
- 44.Verma A, Hirsch DJ, Glatt CE, Ronnett GV, Snyder SH. Carbon monoxide: a putative neural messenger. Science. 1993;259:381–384. doi: 10.1126/science.7678352. [DOI] [PubMed] [Google Scholar]
- 45.Brouard S, Otterbein LE, Anrather J, et al. Carbon monoxide generated by heme oxygenase 1 suppresses endothelial cell apoptosis. J Exp Med. 2000;192:1015–1026. doi: 10.1084/jem.192.7.1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kim HP, Ryter SW, Choi AM. CO as a cellular signaling molecule. Annu Rev Pharmacol Toxicol. 2006;46:411–449. doi: 10.1146/annurev.pharmtox.46.120604.141053. [DOI] [PubMed] [Google Scholar]
- 47.Durante W, Johnson FK, Johnson RA. Role of carbon monoxide in cardiovascular function. J Cell Mol Med. 2006;10:672–686. doi: 10.1111/j.1582-4934.2006.tb00427.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Suematsu M, Kashiwagi S, Sano T, Goda N, Shinoda Y, Ishimura Y. Carbon monoxide as an endogenous modulator of hepatic vascular perfusion. Biochem Biophys Res Commun. 1994;205:1333–1337. doi: 10.1006/bbrc.1994.2811. [DOI] [PubMed] [Google Scholar]
- 49.Morita T, Mitsialis SA, Koike H, Liu Y, Kourembanas S. Carbon monoxide controls the proliferation of hypoxic vascular smooth muscle cells. J Biol Chem. 1997;272:32804–32809. doi: 10.1074/jbc.272.52.32804. [DOI] [PubMed] [Google Scholar]
- 50.Suliman HB, Carraway MS, Tatro LG, Piantadosi CA. A new activating role for CO in cardiac mitochondrial biogenesis. J Cell Sci. 2007;120(Pt 2):299–308. doi: 10.1242/jcs.03318. [DOI] [PubMed] [Google Scholar]
- 51.Lee SJ, Ryter SW, Xu JF, et al. Carbon monoxide activates autophagy via mitochondrial reactive oxygen species formation. Am J Respir Cell Mol Biol. 2011;45:867–873. doi: 10.1165/rcmb.2010-0352OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Otterbein LE, Mantell LL, Choi AM. Carbon monoxide provides protection against hyperoxic lung injury. Am J Physiol. 1999;276(4 Pt 1):L688–L694. doi: 10.1152/ajplung.1999.276.4.L688. [DOI] [PubMed] [Google Scholar]
- 53.Otterbein LE, Otterbein SL, Ifedigbo E, et al. MKK3 mitogen-activated protein kinase pathway mediates carbon monoxide-induced protection against oxidant-induced lung injury. Am J Pathol. 2003;163:2555–2563. doi: 10.1016/S0002-9440(10)63610-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Dolinay T, Szilasi M, Liu M, Choi AM. Inhaled carbon monoxide confers antiinflammatory effects against ventilator-induced lung injury. Am J Respir Crit Care Med. 2004;170:613–620. doi: 10.1164/rccm.200401-023OC. [DOI] [PubMed] [Google Scholar]
- 55.Zhang X, Shan P, Alam J, Davis RJ, Flavell RA, Lee PJ. Carbon monoxide modulates Fas/Fas ligand, caspases, and Bcl-2 family proteins via the p38alpha mitogen-activated protein kinase pathway during ischemia-reperfusion lung injury. J Biol Chem. 2003;278:22061–22070. doi: 10.1074/jbc.M301858200. [DOI] [PubMed] [Google Scholar]
- 56.Zhang X, Shan P, Otterbein LE, et al. Carbon monoxide inhibition of apoptosis during ischemia-reperfusion lung injury is dependent on the p38 mitogen-activated protein kinase pathway and involves caspase 3. J Biol Chem. 2003;278:1248–1258. doi: 10.1074/jbc.M208419200. [DOI] [PubMed] [Google Scholar]
- 57.MacGarvey NC, Suliman HB, Bartz RR, et al. Activation of mitochondrial biogenesis by heme oxygenase-1-mediated NF-E2-related factor-2 induction rescues mice from lethal Staphylococcus aureus sepsis. Am J Respir Crit Care Med. 2012;185:851–861. doi: 10.1164/rccm.201106-1152OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Otterbein LE, Zuckerbraun BS, Haga M, et al. Carbon monoxide suppresses arteriosclerotic lesions associated with chronic graft rejection and with balloon injury. Nat Med. 2003;9:183–190. doi: 10.1038/nm817. [DOI] [PubMed] [Google Scholar]
- 59.Sato K, Balla J, Otterbein L, et al. Carbon monoxide generated by heme oxygenase-1 suppresses the rejection of mouse-to-rat cardiac transplants. J Immunol. 2001;166:4185–4194. doi: 10.4049/jimmunol.166.6.4185. [DOI] [PubMed] [Google Scholar]
- 60.Song R, Kubo M, Morse D, et al. Carbon monoxide induces cytoprotection in rat orthotopic lung transplantation via anti-inflammatory and anti-apoptotic effects. Am J Pathol. 2003;163:231–242. doi: 10.1016/S0002-9440(10)63646-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ryter SW, Choi AM. Heme oxygenase-1/carbon monoxide: novel therapeutic strategies in critical care medicine. Curr Drug Targets. 2010;11:1485–1494. doi: 10.2174/1389450111009011485. [DOI] [PubMed] [Google Scholar]
- 62.Whiteman M, Le Trionnaire S, Chopra M, Fox B, Whatmore J. Emerging role of hydrogen sulfide in health and disease: critical appraisal of biomarkers and pharmacological tools. Clin Sci (Lond) 2011;121:459–488. doi: 10.1042/CS20110267. [DOI] [PubMed] [Google Scholar]
- 63.Yang G, Wu L, Jiang B, et al. H2S as a physiologic vasorelaxant: hypertension in mice with deletion of cystathionine gamma-lyase. Science. 2008;322:587–590. doi: 10.1126/science.1162667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kimura H. Hydrogen sulfide as a neuromodulator. Mol Neurobiol. 2002;26:13–19. doi: 10.1385/MN:26:1:013. [DOI] [PubMed] [Google Scholar]
- 65.Szabo C. Hydrogen sulphide and its therapeutic potential. Nat Rev Drug Discov. 2007;6:917–935. doi: 10.1038/nrd2425. [DOI] [PubMed] [Google Scholar]
- 66.Lowicka E, Beltowski J. Hydrogen sulfide (H2S): the third gas of interest for pharmacologists. Pharmacol Rep. 2007;59:4–24. [PubMed] [Google Scholar]
- 67.Faller S, Spassov SG, Zimmermann KK, et al. Hydrogen sulfide prevents hyperoxia-induced lung injury by downregulating reactive oxygen species formation and angiopoietin-2 release. Curr Pharm Des. 2012 Oct 18; doi: 10.2174/1381612811319150006. [Epub] [DOI] [PubMed] [Google Scholar]
- 68.Faller S, Ryter SW, Choi AM, Loop T, Schmidt R, Hoetzel A. Inhaled hydrogen sulfide protects against ventilator-induced lung injury. Anesthesiology. 2010;113:104–115. doi: 10.1097/ALN.0b013e3181de7107. [DOI] [PubMed] [Google Scholar]
- 69.Spiller F, Orrico MI, Nascimento DC, et al. Hydrogen sulfide improves neutrophil migration and survival in sepsis via K+ATP channel activation. Am J Respir Crit Care Med. 2010;182:360–368. doi: 10.1164/rccm.200907-1145OC. [DOI] [PubMed] [Google Scholar]
- 70.Von Burg R. Carbon monoxide. J Appl Toxicol. 1999;19:379–386. doi: 10.1002/(sici)1099-1263(199909/10)19:5<379::aid-jat563>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 71.Penney D, Benignus V, Kephalopoulos S, Kotzias D, Kleinman M, Verrier A World Health Organization, editors. WHO Guidelines for Indoor Air Quality: Selected Pollutants. Copenhagen: WHO; 2010. Carbon monoxide; p. 55. [PubMed] [Google Scholar]
- 72.Raub J. Environmental Health Criteria 213. Carbon Monoxide Second Edition. Geneva: WHO; 1999. p. 70. [Google Scholar]
- 73.Smith RP. Toxic responses of the blood. In: Casarett LJ, Doull J, Klaassen CD, Amdur MO, editors. Casarett and Doull's Toxicology: the Basic Science of Poisons. 3rd ed. New York: Macmillan; 1986. pp. 223–224. [Google Scholar]
- 74.Gorman D, Drewry A, Huang YL, Sames C. The clinical toxicology of carbon monoxide. Toxicology. 2003;187:25–38. doi: 10.1016/s0300-483x(03)00005-2. [DOI] [PubMed] [Google Scholar]
- 75.Piantadosi CA. Diagnosis and treatment of carbon monoxide poisoning. Respir Care Clin N Am. 1999;5:183–202. [PubMed] [Google Scholar]
- 76.Rudra CB, Williams MA, Sheppard L, et al. Relation of whole blood carboxyhemoglobin concentration to ambient carbon monoxide exposure estimated using regression. Am J Epidemiol. 2010;171:942–951. doi: 10.1093/aje/kwq022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Russell MA. Blood carboxyhaemoglobin changes during tobacco smoking. Postgrad Med J. 1973;49:684–687. doi: 10.1136/pgmj.49.576.684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Samoli E, Touloumi G, Schwartz J, et al. Short-term effects of carbon monoxide on mortality: an analysis within the APHEA project. Environ Health Perspect. 2007;115:1578–1583. doi: 10.1289/ehp.10375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Reboul C, Thireau J, Meyer G, et al. Carbon monoxide exposure in the urban environment: an insidious foe for the heart? Respir Physiol Neurobiol. 2012;184:204–212. doi: 10.1016/j.resp.2012.06.010. [DOI] [PubMed] [Google Scholar]
- 80.Kutty RK, Daniel RF, Ryan DE, Levin W, Maines MD. Rat liver cytochrome P-450b, P-420b, and P-420c are degraded to biliverdin by heme oxygenase. Arch Biochem Biophys. 1988;260:638–644. doi: 10.1016/0003-9861(88)90492-4. [DOI] [PubMed] [Google Scholar]
- 81.Tenhunen R, Ross ME, Marver HS, Schmid R. Reduced nicotinamide-adenine dinucleotide phosphate dependent biliverdin reductase: partial purification and characterization. Biochemistry. 1970;9:298–303. doi: 10.1021/bi00804a016. [DOI] [PubMed] [Google Scholar]
- 82.Vreman HJ, Wong RJ, Stevenson DK. Carbon monoxide in breath, blood, and other tissues. In: Penney DG, editor. Carbon Monoxide Toxicity. Boca Raton: CRC Press; 2000. pp. 19–60. [Google Scholar]
- 83.Cruse I, Maines MD. Evidence suggesting that the two forms of heme oxygenase are products of different genes. J Biol Chem. 1988;263:3348–3353. [PubMed] [Google Scholar]
- 84.Lee PJ, Jiang BH, Chin BY, et al. Hypoxia-inducible factor-1 mediates transcriptional activation of the heme oxygenase-1 gene in response to hypoxia. J Biol Chem. 1997;272:5375–5381. [PubMed] [Google Scholar]
- 85.Lee PJ, Alam J, Sylvester SL, Inamdar N, Otterbein L, Choi AM. Regulation of heme oxygenase-1 expression in vivo and in vitro in hyperoxic lung injury. Am J Respir Cell Mol Biol. 1996;14:556–568. doi: 10.1165/ajrcmb.14.6.8652184. [DOI] [PubMed] [Google Scholar]
- 86.Shibahara S, Muller RM, Taguchi H. Transcriptional control of rat heme oxygenase by heat shock. J Biol Chem. 1987;262:12889–12892. [PubMed] [Google Scholar]
- 87.Alam J, Shibahara S, Smith A. Transcriptional activation of the heme oxygenase gene by heme and cadmium in mouse hepatoma cells. J Biol Chem. 1989;264:6371–6375. [PubMed] [Google Scholar]
- 88.Keyse SM, Applegate LA, Tromvoukis Y, Tyrrell RM. Oxidant stress leads to transcriptional activation of the human heme oxygenase gene in cultured skin fibroblasts. Mol Cell Biol. 1990;10:4967–4969. doi: 10.1128/mcb.10.9.4967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Alam J, Cai J, Smith A. Isolation and characterization of the mouse heme oxygenase-1 gene: distal 5' sequences are required for induction by heme or heavy metals. J Biol Chem. 1994;269:1001–1009. [PubMed] [Google Scholar]
- 90.Alam J, Camhi S, Choi AM. Identification of a second region upstream of the mouse heme oxygenase-1 gene that functions as a basal level and inducer-dependent transcription enhancer. J Biol Chem. 1995;270:11977–11984. doi: 10.1074/jbc.270.20.11977. [DOI] [PubMed] [Google Scholar]
- 91.Alam J, Stewart D, Touchard C, Boinapally S, Choi AM, Cook JL. Nrf2, a Cap'n'Collar transcription factor, regulates induction of the heme oxygenase-1 gene. J Biol Chem. 1999;274:26071–26078. doi: 10.1074/jbc.274.37.26071. [DOI] [PubMed] [Google Scholar]
- 92.Alam J, Wicks C, Stewart D, et al. Mechanism of heme oxygenase-1 gene activation by cadmium in MCF-7 mammary epithelial cells: role of p38 kinase and Nrf2 transcription factor. J Biol Chem. 2000;275:27694–27702. doi: 10.1074/jbc.M004729200. [DOI] [PubMed] [Google Scholar]
- 93.Itoh K, Wakabayashi N, Katoh Y, et al. Keap1 represses nuclear activation of antioxidant responsive elements by Nrf2 through binding to the amino-terminal Neh2 domain. Genes Dev. 1999;13:76–86. doi: 10.1101/gad.13.1.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Kobayashi A, Kang MI, Okawa H, et al. Oxidative stress sensor Keap1 functions as an adaptor for Cul3-based E3 ligase to regulate proteasomal degradation of Nrf2. Mol Cell Biol. 2004;24:7130–7139. doi: 10.1128/MCB.24.16.7130-7139.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Ogawa K, Sun J, Taketani S, et al. Heme mediates derepression of Maf recognition element through direct binding to transcription repressor Bach1. EMBO J. 2001;20:2835–2843. doi: 10.1093/emboj/20.11.2835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Sun J, Hoshino H, Takaku K, et al. Hemoprotein Bach1 regulates enhancer availability of heme oxygenase-1 gene. EMBO J. 2002;21:5216–5224. doi: 10.1093/emboj/cdf516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Alam J, Igarashi K, Immenschuh S, Shibahara S, Tyrrell RM. Regulation of heme oxygenase-1 gene transcription: recent advances and highlights from the International Conference (Uppsala, 2003) on Heme Oxygenase. Antioxid Redox Signal. 2004;6:924–933. doi: 10.1089/ars.2004.6.924. [DOI] [PubMed] [Google Scholar]
- 98.Alam J, Cook JL. How many transcription factors does it take to turn on the heme oxygenase-1 gene? Am J Respir Cell Mol Biol. 2007;36:166–174. doi: 10.1165/rcmb.2006-0340TR. [DOI] [PubMed] [Google Scholar]
- 99.Stone JR, Marletta MA. Soluble guanylate cyclase from bovine lung: activation with nitric oxide and carbon monoxide and spectral characterization of the ferrous and ferric states. Biochemistry. 1994;33:5636–5640. doi: 10.1021/bi00184a036. [DOI] [PubMed] [Google Scholar]
- 100.Furchgott RF, Jothianandan D. Endothelium-dependent and -independent vasodilation involving cyclic GMP: relaxation induced by nitric oxide, carbon monoxide and light. Blood Vessels. 1991;28:52–61. doi: 10.1159/000158843. [DOI] [PubMed] [Google Scholar]
- 101.Suematsu M, Goda N, Sano T, et al. Carbon monoxide: an endogenous modulator of sinusoidal tone in the perfused rat liver. J Clin Invest. 1995;96:2431–2437. doi: 10.1172/JCI118300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Wang R. Resurgence of carbon monoxide: an endogenous gaseous vasorelaxing factor. Can J Physiol Pharmacol. 1998;76:1–15. doi: 10.1139/cjpp-76-1-1. [DOI] [PubMed] [Google Scholar]
- 103.Nakahira K, Kim HP, Geng XH, et al. Carbon monoxide differentially inhibits TLR signaling pathways by regulating ROS-induced trafficking of TLRs to lipid rafts. J Exp Med. 2006;203:2377–2389. doi: 10.1084/jem.20060845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Kim HP, Wang X, Zhang J, et al. Heat shock protein-70 mediates the cytoprotective effect of carbon monoxide: involvement of p38 beta MAPK and heat shock factor-1. J Immunol. 2005;175:2622–2629. doi: 10.4049/jimmunol.175.4.2622. [DOI] [PubMed] [Google Scholar]
- 105.Bilban M, Bach FH, Otterbein SL, et al. Carbon monoxide orchestrates a protective response through PPARgamma. Immunity. 2006;24:601–610. doi: 10.1016/j.immuni.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 106.Brouard S, Berberat PO, Tobiasch E, Seldon MP, Bach FH, Soares MP. Heme oxygenase-1-derived carbon monoxide requires the activation of transcription factor NF-kappa B to protect endothelial cells from tumor necrosis factor-alpha-mediated apoptosis. J Biol Chem. 2002;277:17950–17961. doi: 10.1074/jbc.M108317200. [DOI] [PubMed] [Google Scholar]
- 107.Zhang X, Shan P, Alam J, Fu XY, Lee PJ. Carbon monoxide differentially modulates STAT1 and STAT3 and inhibits apoptosis via a phosphatidylinositol 3-kinase/Akt and p38 kinase-dependent STAT3 pathway during anoxia-reoxygenation injury. J Biol Chem. 2005;280:8714–8721. doi: 10.1074/jbc.M408092200. [DOI] [PubMed] [Google Scholar]
- 108.Wang X, Wang Y, Kim HP, Nakahira K, Ryter SW, Choi AM. Carbon monoxide protects against hyperoxia-induced endothelial cell apoptosis by inhibiting reactive oxygen species formation. J Biol Chem. 2007;282:1718–1726. doi: 10.1074/jbc.M607610200. [DOI] [PubMed] [Google Scholar]
- 109.Wang X, Wang Y, Lee SJ, Kim HP, Choi AM, Ryter SW. Carbon monoxide inhibits Fas activating antibody-induced apoptosis in endothelial cells. Med Gas Res. 2011;1:8. doi: 10.1186/2045-9912-1-8. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 110.Morita T, Perrella MA, Lee ME, Kourembanas S. Smooth muscle cell-derived carbon monoxide is a regulator of vascular cGMP. Proc Natl Acad Sci U S A. 1995;92:1475–1479. doi: 10.1073/pnas.92.5.1475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Morita T, Kourembanas S. Endothelial cell expression of vasoconstrictors and growth factors is regulated by smooth muscle cell-derived carbon monoxide. J Clin Invest. 1995;96:2676–2682. doi: 10.1172/JCI118334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Kim HP, Wang X, Nakao A, et al. Caveolin-1 expression by means of p38beta mitogen-activated protein kinase mediates the antiproliferative effect of carbon monoxide. Proc Natl Acad Sci U S A. 2005;102:11319–11324. doi: 10.1073/pnas.0501345102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Taille C, El-Benna J, Lanone S, Boczkowski J, Motterlini R. Mitochondrial respiratory chain and NAD(P)H oxidase are targets for the antiproliferative effect of carbon monoxide in human airway smooth muscle. J Biol Chem. 2005;280:25350–25360. doi: 10.1074/jbc.M503512200. [DOI] [PubMed] [Google Scholar]
- 114.Rodriguez AI, Gangopadhyay A, Kelley EE, Pagano PJ, Zuckerbraun BS, Bauer PM. HO-1 and CO decrease platelet-derived growth factor-induced vascular smooth muscle cell migration via inhibition of Nox1. Arterioscler Thromb Vasc Biol. 2010;30:98–104. doi: 10.1161/ATVBAHA.109.197822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Morse D, Pischke SE, Zhou Z, et al. Suppression of inflammatory cytokine production by carbon monoxide involves the JNK pathway and AP-1. J Biol Chem. 2003;278:36993–36998. doi: 10.1074/jbc.M302942200. [DOI] [PubMed] [Google Scholar]
- 116.Mazzola S, Forni M, Albertini M, et al. Carbon monoxide pretreatment prevents respiratory derangement and ameliorates hyperacute endotoxic shock in pigs. FASEB J. 2005;19:2045–2047. doi: 10.1096/fj.05-3782fje. [DOI] [PubMed] [Google Scholar]
- 117.Mitchell LA, Channell MM, Royer CM, Ryter SW, Choi AM, McDonald JD. Evaluation of inhaled carbon monoxide as an anti-inflammatory therapy in a nonhuman primate model of lung inflammation. Am J Physiol Lung Cell Mol Physiol. 2010;299:L891–L897. doi: 10.1152/ajplung.00366.2009. [DOI] [PubMed] [Google Scholar]
- 118.Ghosh S, Wilson MR, Choudhury S, et al. Effects of inhaled carbon monoxide on acute lung injury in mice. Am J Physiol Lung Cell Mol Physiol. 2005;288:L1003–L1009. doi: 10.1152/ajplung.00451.2004. [DOI] [PubMed] [Google Scholar]
- 119.Clayton CE, Carraway MS, Suliman HB, et al. Inhaled carbon monoxide and hyperoxic lung injury in rats. Am J Physiol Lung Cell Mol Physiol. 2001;281:L949–L957. doi: 10.1152/ajplung.2001.281.4.L949. [DOI] [PubMed] [Google Scholar]
- 120.Fernandez-Gonzalez A, Alex Mitsialis S, Liu X, Kourembanas S. Vasculoprotective effects of heme oxygenase-1 in a murine model of hyperoxia-induced bronchopulmonary dysplasia. Am J Physiol Lung Cell Mol Physiol. 2012;302:L775–L784. doi: 10.1152/ajplung.00196.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Hoetzel A, Schmidt R, Vallbracht S, et al. Carbon monoxide prevents ventilator-induced lung injury via caveolin-1. Crit Care Med. 2009;37:1708–1715. doi: 10.1097/CCM.0b013e31819efa31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Hoetzel A, Dolinay T, Vallbracht S, et al. Carbon monoxide protects against ventilator-induced lung injury via PPAR-gamma and inhibition of Egr-1. Am J Respir Crit Care Med. 2008;177:1223–1232. doi: 10.1164/rccm.200708-1265OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Faller S, Foeckler M, Strosing KM, et al. Kinetic effects of carbon monoxide inhalation on tissue protection in ventilator-induced lung injury. Lab Invest. 2012;92:999–1012. doi: 10.1038/labinvest.2012.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Fujita T, Toda K, Karimova A, et al. Paradoxical rescue from ischemic lung injury by inhaled carbon monoxide driven by derepression of fibrinolysis. Nat Med. 2001;7:598–604. doi: 10.1038/87929. [DOI] [PubMed] [Google Scholar]
- 125.Mishra S, Fujita T, Lama VN, et al. Carbon monoxide rescues ischemic lungs by interrupting MAPK-driven expression of early growth response 1 gene and its downstream target genes. Proc Natl Acad Sci U S A. 2006;103:5191–5196. doi: 10.1073/pnas.0600241103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Schallner N, Fuchs M, Schwer CI, et al. Postconditioning with inhaled carbon monoxide counteracts apoptosis and neuroinflammation in the ischemic rat retina. PLoS One. 2012;7:e46479. doi: 10.1371/journal.pone.0046479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Nakao A, Kimizuka K, Stolz DB, et al. Protective effect of carbon monoxide inhalation for cold-preserved small intestinal grafts. Surgery. 2003;134:285–292. doi: 10.1067/msy.2003.238. [DOI] [PubMed] [Google Scholar]
- 128.Faleo G, Neto JS, Kohmoto J, et al. Carbon monoxide ameliorates renal cold ischemia-reperfusion injury with an upregulation of vascular endothelial growth factor by activation of hypoxia-inducible factor. Transplantation. 2008;85:1833–1840. doi: 10.1097/TP.0b013e31817c6f63. [DOI] [PubMed] [Google Scholar]
- 129.Kaizu T, Nakao A, Tsung A, et al. Carbon monoxide inhalation ameliorates cold ischemia/reperfusion injury after rat liver transplantation. Surgery. 2005;138:229–235. doi: 10.1016/j.surg.2005.06.015. [DOI] [PubMed] [Google Scholar]
- 130.Kohmoto J, Nakao A, Kaizu T, et al. Low-dose carbon monoxide inhalation prevents ischemia/reperfusion injury of transplanted rat lung grafts. Surgery. 2006;140:179–185. doi: 10.1016/j.surg.2006.03.004. [DOI] [PubMed] [Google Scholar]
- 131.Kohmoto J, Nakao A, Sugimoto R, et al. Carbon monoxide-saturated preservation solution protects lung grafts from ischemia-reperfusion injury. J Thorac Cardiovasc Surg. 2008;136:1067–1075. doi: 10.1016/j.jtcvs.2008.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Nakao A, Toyokawa H, Tsung A, et al. Ex vivo application of carbon monoxide in University of Wisconsin solution to prevent intestinal cold ischemia/reperfusion injury. Am J Transplant. 2006;6:2243–2255. doi: 10.1111/j.1600-6143.2006.01465.x. [DOI] [PubMed] [Google Scholar]
- 133.Pannen BH, Kohler N, Hole B, Bauer M, Clemens MG, Geiger KK. Protective role of endogenous carbon monoxide in hepatic microcirculatory dysfunction after hemorrhagic shock in rats. J Clin Invest. 1998;102:1220–1228. doi: 10.1172/JCI3428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Amersi F, Shen XD, Anselmo D, et al. Ex vivo exposure to carbon monoxide prevents hepatic ischemia/reperfusion injury through p38 MAP kinase pathway. Hepatology. 2002;35:815–823. doi: 10.1053/jhep.2002.32467. [DOI] [PubMed] [Google Scholar]
- 135.Christou H, Morita T, Hsieh CM, et al. Prevention of hypoxia-induced pulmonary hypertension by enhancement of endogenous heme oxygenase-1 in the rat. Circ Res. 2000;86:1224–1229. doi: 10.1161/01.res.86.12.1224. [DOI] [PubMed] [Google Scholar]
- 136.Minamino T, Christou H, Hsieh CM, et al. Targeted expression of heme oxygenase-1 prevents the pulmonary inflammatory and vascular responses to hypoxia. Proc Natl Acad Sci U S A. 2001;98:8798–8803. doi: 10.1073/pnas.161272598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Yet SF, Perrella MA, Layne MD, et al. Hypoxia induces severe right ventricular dilatation and infarction in heme oxygenase-1 null mice. J Clin Invest. 1999;103:R23–R29. doi: 10.1172/JCI6163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Zuckerbraun BS, Chin BY, Wegiel B, et al. Carbon monoxide reverses established pulmonary hypertension. J Exp Med. 2006;203:2109–2119. doi: 10.1084/jem.20052267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Dubuis E, Potier M, Wang R, Vandier C. Continuous inhalation of carbon monoxide attenuates hypoxic pulmonary hypertension development presumably through activation of BKCa channels. Cardiovasc Res. 2005;65:751–761. doi: 10.1016/j.cardiores.2004.11.007. [DOI] [PubMed] [Google Scholar]
- 140.Selman M, King TE, Pardo A American Thoracic Society; European Respiratory Society; American College of Chest Physicians. Idiopathic pulmonary fibrosis: prevailing and evolving hypotheses about its pathogenesis and implications for therapy. Ann Intern Med. 2001;134:136–151. doi: 10.7326/0003-4819-134-2-200101160-00015. [DOI] [PubMed] [Google Scholar]
- 141.Zhou Z, Song R, Fattman CL, et al. Carbon monoxide suppresses bleomycin-induced lung fibrosis. Am J Pathol. 2005;166:27–37. doi: 10.1016/S0002-9440(10)62229-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Choi KM, Gibbons SJ, Nguyen TV, et al. Heme oxygenase-1 protects interstitial cells of Cajal from oxidative stress and reverses diabetic gastroparesis. Gastroenterology. 2008;135:2055–2064. doi: 10.1053/j.gastro.2008.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Kashyap PC, Choi KM, Dutta N, et al. Carbon monoxide reverses diabetic gastroparesis in NOD mice. Am J Physiol Gastrointest Liver Physiol. 2010;298:G1013–G1019. doi: 10.1152/ajpgi.00069.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Rodella L, Lamon BD, Rezzani R, et al. Carbon monoxide and biliverdin prevent endothelial cell sloughing in rats with type I diabetes. Free Radic Biol Med. 2006;40:2198–2205. doi: 10.1016/j.freeradbiomed.2006.02.018. [DOI] [PubMed] [Google Scholar]
- 145.Simon T, Pogu S, Tardif V, et al. Carbon monoxide-treated dendritic cells decrease beta1-integrin induction on CD8(+) T cells and protect from type 1 diabetes. Eur J Immunol. 2013;43:209–218. doi: 10.1002/eji.201242684. [DOI] [PubMed] [Google Scholar]
- 146.Gunther L, Berberat PO, Haga M, et al. Carbon monoxide protects pancreatic beta-cells from apoptosis and improves islet function/survival after transplantation. Diabetes. 2002;51:994–999. doi: 10.2337/diabetes.51.4.994. [DOI] [PubMed] [Google Scholar]
- 147.Wang H, Lee SS, Gao W, et al. Donor treatment with carbon monoxide can yield islet allograft survival and tolerance. Diabetes. 2005;54:1400–1406. doi: 10.2337/diabetes.54.5.1400. [DOI] [PubMed] [Google Scholar]
- 148.Joe Y, Zheng M, Kim SK, et al. The role of carbon monoxide in metabolic disease. Ann N Y Acad Sci. 2011;1229:156–161. doi: 10.1111/j.1749-6632.2011.06121.x. [DOI] [PubMed] [Google Scholar]
- 149.Lancel S, Montaigne D, Marechal X, et al. Carbon monoxide improves cardiac function and mitochondrial population quality in a mouse model of metabolic syndrome. PLoS One. 2012;7:e41836. doi: 10.1371/journal.pone.0041836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Bainbridge SA, Sidle EH, Smith GN. Direct placental effects of cigarette smoke protect women from pre-eclampsia: the specific roles of carbon monoxide and antioxidant systems in the placenta. Med Hypotheses. 2005;64:17–27. doi: 10.1016/j.mehy.2004.06.019. [DOI] [PubMed] [Google Scholar]
- 151.Ahmed A, Rahman M, Zhang X, et al. Induction of placental heme oxygenase-1 is protective against TNFalpha-induced cytotoxicity and promotes vessel relaxation. Mol Med. 2000;6:391–409. [PMC free article] [PubMed] [Google Scholar]
- 152.Yusuf K, Kamaluddeen M, Wilson RD, Akierman A. Carboxyhemoglobin levels in umbilical cord blood of women with pre-eclampsia and intrauterine growth restriction. J Perinat Med. 2012 Jun 24; doi: 10.1515/jpm-2011-0312. [Epub]. http://dx.doi.org/10.1515/jpm-2011-0312. [DOI] [PubMed] [Google Scholar]
- 153.Bainbridge SA, Belkacemi L, Dickinson M, Graham CH, Smith GN. Carbon monoxide inhibits hypoxia/reoxygenation-induced apoptosis and secondary necrosis in syncytiotrophoblast. Am J Pathol. 2006;169:774–783. doi: 10.2353/ajpath.2006.060184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Zhai D, Guo Y, Smith G, Krewski D, Walker M, Wen SW. Maternal exposure to moderate ambient carbon monoxide is associated with decreased risk of preeclampsia. Am J Obstet Gynecol. 2012;207:57. doi: 10.1016/j.ajog.2012.03.022. [DOI] [PubMed] [Google Scholar]
- 155.Motterlini R, Mann BE, Foresti R. Therapeutic applications of carbon monoxide-releasing molecules. Expert Opin Investig Drugs. 2005;14:1305–1318. doi: 10.1517/13543784.14.11.1305. [DOI] [PubMed] [Google Scholar]
- 156.Foresti R, Bani-Hani MG, Motterlini R. Use of carbon monoxide as a therapeutic agent: promises and challenges. Intensive Care Med. 2008;34:649–658. doi: 10.1007/s00134-008-1011-1. [DOI] [PubMed] [Google Scholar]
- 157.Motterlini R, Sawle P, Hammad J, et al. CORM-A1: a new pharmacologically active carbon monoxide-releasing molecule. FASEB J. 2005;19:284–286. doi: 10.1096/fj.04-2169fje. [DOI] [PubMed] [Google Scholar]
- 158.Kretschmer R, Gessner G, Gorls H, Heinemann SH, Westerhausen M. Dicarbonyl-bis(cysteamine)iron(II): a light induced carbon monoxide releasing molecule based on iron (CORM-S1) J Inorg Biochem. 2011;105:6–9. doi: 10.1016/j.jinorgbio.2010.10.006. [DOI] [PubMed] [Google Scholar]
- 159.Hasegawa U, van der, Simeoni E, Wandrey C, Hubbell JA. Carbon monoxide-releasing micelles for immunotherapy. J Am Chem Soc. 2010;132:18273–18280. doi: 10.1021/ja1075025. [DOI] [PubMed] [Google Scholar]
- 160.Motterlini R, Sawle P, Hammad J, et al. Vasorelaxing effects and inhibition of nitric oxide in macrophages by new iron-containing carbon monoxide-releasing molecules (CO-RMs) Pharmacol Res. 2013;68:108–117. doi: 10.1016/j.phrs.2012.12.001. [DOI] [PubMed] [Google Scholar]
- 161.Foresti R, Hammad J, Clark JE, et al. Vasoactive properties of CORM-3, a novel water-soluble carbon monoxide-releasing molecule. Br J Pharmacol. 2004;142:453–460. doi: 10.1038/sj.bjp.0705825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Sawle P, Foresti R, Mann BE, Johnson TR, Green CJ, Motterlini R. Carbon monoxide-releasing molecules (CO-RMs) attenuate the inflammatory response elicited by lipopolysaccharide in RAW264.7 murine macrophages. Br J Pharmacol. 2005;145:800–810. doi: 10.1038/sj.bjp.0706241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Sun B, Zou X, Chen Y, Zhang P, Shi G. Preconditioning of carbon monoxide releasing molecule-derived CO attenuates LPS-induced activation of HUVEC. Int J Biol Sci. 2008;4:270–278. doi: 10.7150/ijbs.4.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Sun B, Sun H, Liu C, Shen J, Chen Z, Chen X. Role of CO-releasing molecules liberated CO in attenuating leukocytes sequestration and inflammatory responses in the lung of thermally injured mice. J Surg Res. 2007;139:128–135. doi: 10.1016/j.jss.2006.08.032. [DOI] [PubMed] [Google Scholar]
- 165.Cepinskas G, Katada K, Bihari A, Potter RF. Carbon monoxide liberated from carbon monoxide-releasing molecule CORM-2 attenuates inflammation in the liver of septic mice. Am J Physiol Gastrointest Liver Physiol. 2008;294:G184–G191. doi: 10.1152/ajpgi.00348.2007. [DOI] [PubMed] [Google Scholar]
- 166.Mizuguchi S, Stephen J, Bihari R, et al. CORM-3-derived CO modulates polymorphonuclear leukocyte migration across the vascular endothelium by reducing levels of cell surface-bound elastase. Am J Physiol Heart Circ Physiol. 2009;297:H920–H929. doi: 10.1152/ajpheart.00305.2009. [DOI] [PubMed] [Google Scholar]
- 167.Lancel S, Hassoun SM, Favory R, Decoster B, Motterlini R, Neviere R. Carbon monoxide rescues mice from lethal sepsis by supporting mitochondrial energetic metabolism and activating mitochondrial biogenesis. J Pharmacol Exp Ther. 2009;329:641–648. doi: 10.1124/jpet.108.148049. [DOI] [PubMed] [Google Scholar]
- 168.Musameh MD, Green CJ, Mann BE, Fuller BJ, Motterlini R. Improved myocardial function after cold storage with preservation solution supplemented with a carbon monoxide-releasing molecule (CORM-3) J Heart Lung Transplant. 2007;26:1192–1198. doi: 10.1016/j.healun.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 169.Mayr FB, Spiel A, Leitner J, et al. Effects of carbon monoxide inhalation during experimental endotoxemia in humans. Am J Respir Crit Care Med. 2005;171:354–360. doi: 10.1164/rccm.200404-446OC. [DOI] [PubMed] [Google Scholar]
- 170.Bathoorn E, Slebos DJ, Postma DS, et al. Anti-inflammatory effects of inhaled carbon monoxide in patients with COPD: a pilot study. Eur Respir J. 2007;30:1131–1137. doi: 10.1183/09031936.00163206. [DOI] [PubMed] [Google Scholar]