Abstract
Background/Aims
Hepatic or splenic lesions in hematologic patients are not defined well because they are not easy to evaluate due to limitations of invasive procedures. Management typically depends on the clinical diagnosis with few microbiological data.
Methods
We reviewed the medical records of consecutive hematologic patients with hepatic or splenic lesions in the infectious diseases unit from April 2009 to December 2010 at the Catholic Hematopoietic Stem Cell Transplantation Center in Korea.
Results
Twenty-six patients were identified. Their mean age was 46.0 ± 14.7 years, and 16 (61.5%) were male. Underlying diseases were acute myelogenous leukemia (n = 15, 57.7%) and myelodysplastic syndrome (n = 6, 23.1%). Among the nine nontuberculous infectious lesions, two bacterial, six fungal, and one combined infection were identified. The numbers of confirmed, probable, and possible tuberculosis (TB) cases were one, three, and four, respectively. Two patients had concurrent pulmonary TB. QuantiFERON-TB Gold In-Tube (QFT-GIT, Cellestis Ltd.) was positive in seven cases, among which six were diagnosed with TB. The sensitivity and specificity of QFT-GIT were 75% and 81.3%. Nine (34.6%) were defined as noninfectious causes.
Conclusions
Causes of hepatic or splenic lesion in hematologic patients were diverse including TB, non-TB organisms, and noninfectious origins. TB should be considered for patients not responding to antibacterial or antifungal drugs, even in the absence of direct microbiological evidence. QFT-GIT may be useful for a differential diagnosis of hepatosplenic lesions in hematologic patients.
Keywords: Hematology, Liver abscess, Tuberculosis, Diagnosis
INTRODUCTION
Patients with fever and hepatic or splenic lesions should have an abscess ruled out. Traditionally, amebic and pyogenic infections are the two most common causes of liver abscess and the former has decreased with improved public and individual hygiene [1,2]. Hepatosplenic fungal infection is another possible diagnosis, particularly in patients with hematologic malignancies such as acute leukemia [3,4] or tuberculosis (TB) in Korea where pulmonary and extrapulmonary TB are still common [5].
A diagnosis of hepatosplenic lesions usually depends on invasive procedures such as sonography-guided biopsy or aspiration with subsequent microbiological confirmation. However, invasive diagnostic procedures are not easy to perform in hematologic patients because of the increased bleeding risk and marked neutropenia following intensive chemotherapy. Therefore, management is largely dependent on clinical diagnosis when few microbiological data are available.
QuantiFERON-TB Gold In-Tube (QFT-GIT, Cellestis Ltd., Victoria, Australia) is one of two interferon-γ release assays (IGRAs) that have been approved by the U.S. Food and Drug Administration and recommended by the U.S. Centers for Disease Control and Prevention as an aid to detection of latent TB infection among patients at risk [6]. Several studies have investigated the diagnostic performance of IGRAs for extrapulmonary TB (E-TB) with some promising results [7-9].
In this retrospective study, we investigated the clinical characteristics, causes, and outcomes of hepatic or splenic lesions and evaluated the usefulness of the QFT-GIT for the diagnosis of TB in febrile patients with hematologic diseases.
METHODS
Study patients and data collection
We identified all consecutive cases of hepatic or splenic lesions in patients with hematologic diseases who were admitted to the infectious diseases (IDs) unit or who consulted with the hematologic unit from April 2009 to December 2010 at the Catholic Hematopoietic Stem Cell Transplantation (HSCT) Center in Korea. The following data were collected from all cases; demographic information (e.g., age and sex), underlying diseases, medical history, microbiological data, radiological findings, site of infection, medical and surgical treatment, laboratory findings including QFT-GIT results, and other important clinical parameters at the time of infection and follow-up. The QFT-GIT test and interpretation were performed according to the manufacturer's instructions (Cellestis Ltd.). Serum detection of galactomannan (GM) by Platelia Aspergillus assay (Bio-Rad Laboratories, Marenes-La-Couquette, France) and blood chemistry were performed at least twice weekly at our institution, and other examinations were conducted as clinically indicated. The endpoint of the study was April 2011 or time of death or follow-up loss. This study was approved by the Institutional Review Board at Seoul St. Mary's Hospital with a waiver of informed consent (Project No. KC11RISI0366).
Evaluation of hepatosplenic lesions
All patient medical records and images were reviewed by two IDs specialists, the attending hematologist, and one radiologist. Infectious lesions were classified as TB or non-TB infections. When infections were suspected without identifying a causative organism, the decision was based on the response to empirical antibacterial or antifungal drugs. Invasive fungal disease (IFD) was defined according to the European Organization for Research and Treatment of Cancer/Mycosis Study Group (EORTC/MSG) definition criteria [10]. We made a final clinical diagnosis for noninfectious lesions based on a combination of the response to anti-cancer chemotherapy, underlying disease status, serial radiological findings, and laboratory results.
The categories of diagnostic certainty for TB were classified as "confirmed," "probable," and "possible." They were defined as described in previous studies [7,11]. A confirmed case was defined as positive for Mycobacterium tuberculosis in culture or by the M. tuberculosis polymerase chain reaction in any clinical specimen. A probable case was defined as clinical suspicion of TB and one of the following: histological finding of biopsy tissue showing granulomatous inflammation with caseating necrosis or positive acid fast bacilli stain results in a clinical specimen. A possible case was defined as successful clinical and radiological response to empirical anti-TB therapy when antibacterial and antifungal drugs were ineffective. The QFT-GIT results did not influence the certainty of diagnosis.
Assessment of response to therapy and outcome
We assessed the clinical response to therapy for the infectious lesions as described in a previous study with modifications [12]. Follow-up computed tomography (CT) was required for at least 4 weeks after treatment in cases of medical treatment alone. Cure was defined as complete resolution of radiological findings without relapse and disappearance of all attributable signs and symptoms. Improvement was defined as a decrease in the number and size or more than a one-third decrease in the greatest diameter with clinical improvement. Responses that did not fulfill the above criteria were defined as failure. When a patient died without follow-up radiology, the case was considered a failure. Outcome for all cases was assessed as either survival or death on the last follow-up day. Radiological images were analyzed by a radiologist and reviewed for a response.
Statistics
Statistical significance was assessed via the chi-squared test or the Fisher's exact test for categorical variables and the independent t test or the Mann-Whitney U test for continuous variables. The p values < 0.05 were considered to indicate statistical significance.
RESULTS
Patients' characteristics
Twenty-seven cases were identified during the study period. One case was excluded because the patient refused further evaluation after the initial CT scan. The baseline demographic and clinical characteristics of the 26 patients are shown in Table 1. The mean age of the patients was 46.0 ± 14.7 years, and 16 were male (61.5%). Underlying diseases were acute myelogenous leukemia (n = 15, 57.7%), myelodysplastic syndrome (n = 6, 23.1%), acute lymphoblastic leukemia (n = 2, 7.7%), lymphoma (n = 2, 7.7%), and severe aplastic anemia (n = 1, 3.7%). None of the patients had a history of TB or diabetes. Laboratory findings were not different between the infectious and noninfectious groups except hypoalbuminemia, which was more common in the infectious group (p = 0.038). Among 17 infectious cases, eight (47.1%) were demonstrated to be TB. Invasive procedures were performed in 34.6% (9/26) of the patients, which included biopsy (n = 5), drainage (n = 1), left lateral sectionectomy of the liver, followed by drainage (n = 1) and splenectomy (n = 2). The mean follow-up period was 241 ± 172 days. Most patients had liver involvement, and only two patients in the infectious group had spleen involvement without liver invasion (Table 2).
Table 1.
Patient baseline demographic and clinical characteristics
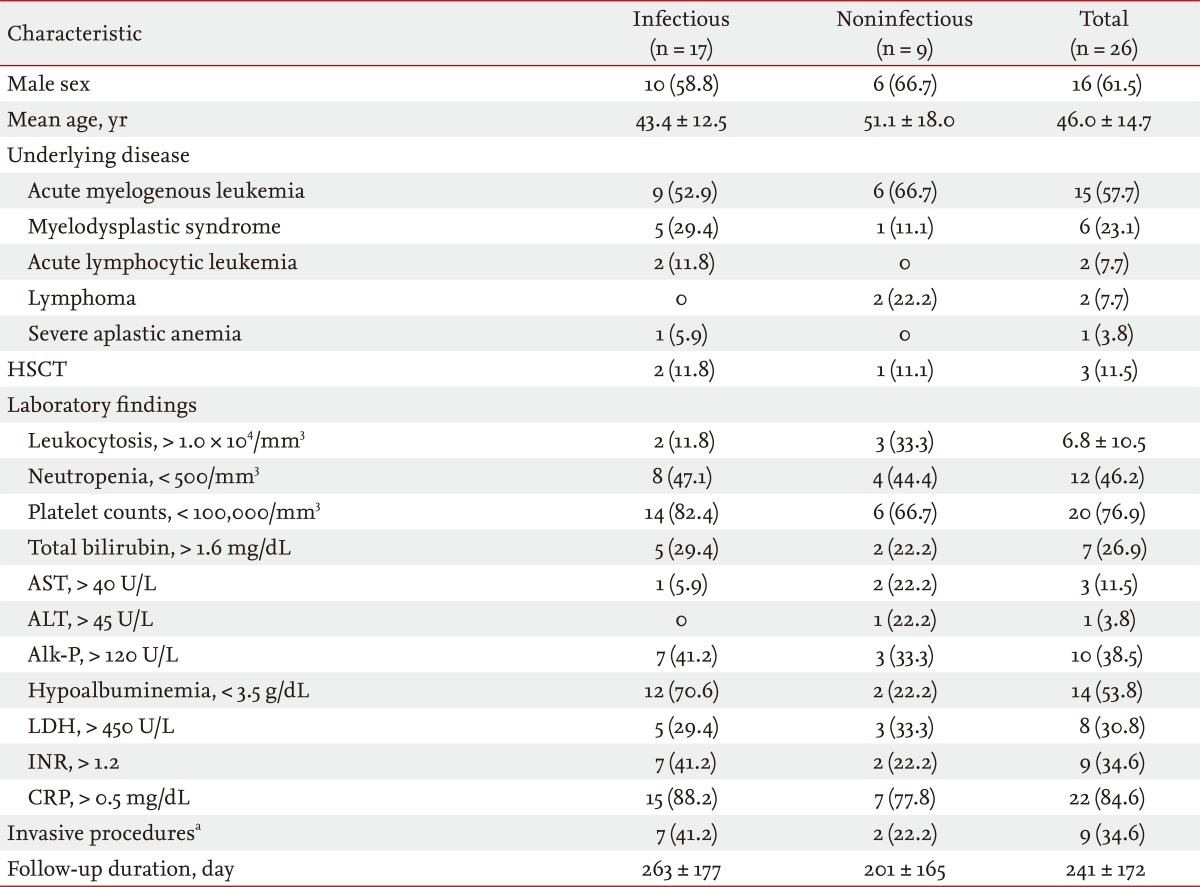
Values are presented as number (%) or mean ± SD.
HSCT, hematopoietic stem cell transplantation; AST, aspartate transaminase; ALT, alanine transaminase; Alk-P, alkaline phosphatase; LDH, lactate dehydrogenase; INR, international normalized ratio; CRP, C-reactive protein.
aIncludes percutaneous aspiration or biopsy, drainage, and surgical resection.
Table 2.
Locations, numbers, and sizes of lesions according to etiology
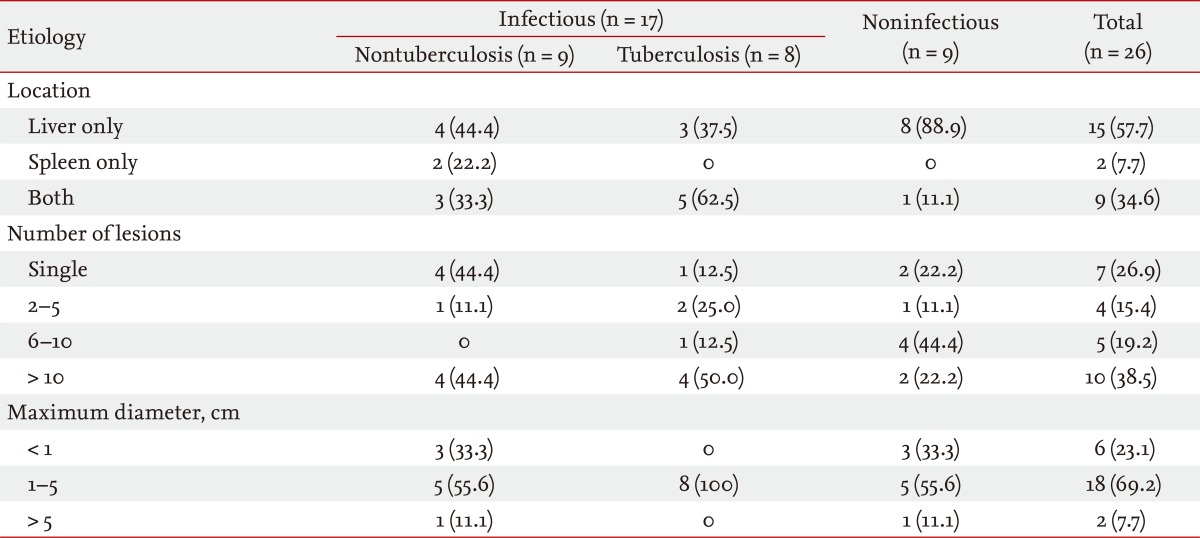
Values are presented as number (%).
Characteristics according to the origin of the hepatic or splenic lesions
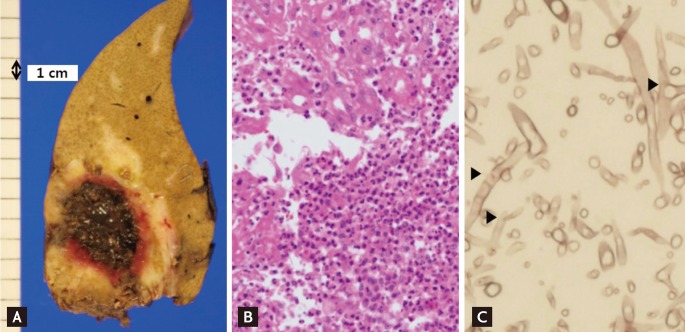
The characteristics of the nine patients with non-TB bacterial or fungal infections are presented in Table 3. Six fungal, two bacterial, and one combined infection were identified. Disseminated candidiasis was assumed in three patients, among which two (cases 7 and 9) were positive for Candida tropicalis in a blood culture. They were considered "probable" disseminated candidiasis by the 2008 EORTC/MSG criteria for IFD. The other patient (case 3) was considered "possible" disseminated candidiasis and developed multiple target-like lesions in the liver and spleen with a negative blood culture. Case 6 had splenic abscess with septic pneumonia caused by Escherichia coli. Case 8 showed ~7-cm single liver abscess at presentation, a pig-tail drainage catheter was inserted, and Enterococcus faecium was identified from the abscess culture. Teicoplanin (400 mg every 12 hours for three doses, then 400 mg once/day intravenously) was administered for 3 weeks but the follow-up CT scan revealed little interval change. She underwent a left lateral sectionectomy of the liver and the pathology showed septated branched hyphae with tissue invasion consistent with an invasive mold infection (Fig. 1) but tissue culture for fungus was negative. Allogeneic HSCT was performed successfully after 4 months.
Table 3.
Characteristics of nine patients with nontuberculosis bacterial or fungal infections
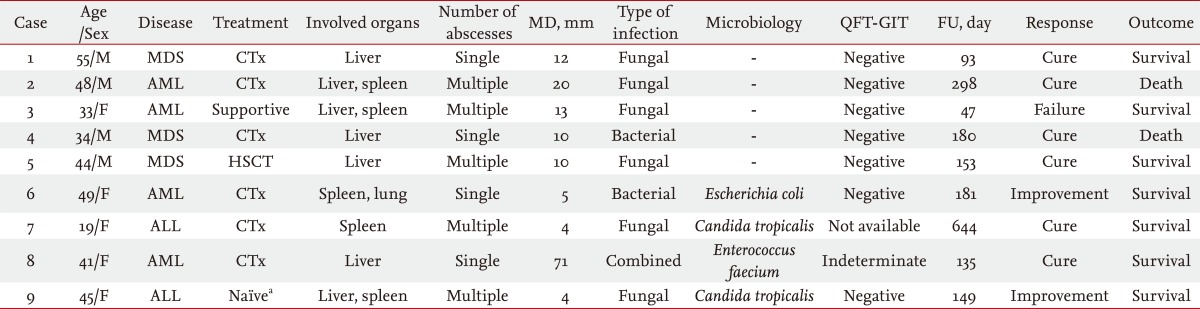
MD, maximum diameter; QFT-GIT, QuantiFERON-TB Gold In-Tube; FU, follow-up; MDS, myelodysplastic syndrome; CTx, chemotherapy; AML, acute myelogenous leukemia; HSCT, hematopoietic stem cell transplantation; ALL, acute lymphoblastic leukemia.
aNaïve, newly diagnosed without previous anticancer chemotherapy.
Figure 1.
Gross and microscopic findings of case 8. (A) A ~6 × 3-cm necrotic mass surrounded by hemorrhage is noted. (B) Abscess formation with fibrosis and necrosis is observed (H&E, × 200). (C) Fungi with Y-shaped branching septated hyphae (arrows) suspicious of Aspergillus species are scattered (Grocott-Gomori methenamine silver stain, × 400). Adapted from Hong et al. Infect Chemother 2011;43:377-381, with permission from The Korean Society of Infectious Diseases and Korean Society for Chemotherapy [17].
The characteristics of the eight TB patients are presented in Table 4. One patient (case 10) successfully underwent unrelated HSCT while taking anti-TB medications. The numbers of confirmed, probable, and possible TB cases were one, three, and four, respectively. One patient (case 16) was confirmed by tissue PCR for M. tuberculosis after splenectomy. Two probable cases (cases 12 and 15) had concurrent confirmed pulmonary TB. The organisms cultured from these two pulmonary TB cases were susceptible to all commonly used first and second line anti-TB drugs, but one patient died before the end of anti-TB treatment due to progressive acute myeloid leukemia. Three patients were taking voriconazole (VCZ) to treat invasive pulmonary aspergillosis and they took levofloxacin instead of rifampin, which has significant drug interactions with VCZ. One patient with probable TB (case 15) who had disseminated disease changed to a second-line anti-TB drug after 8 months. Two patients (cases 15 and 16) are still taking anti-TB drugs.
Table 4.
Characteristics of eight patients with tuberculosis
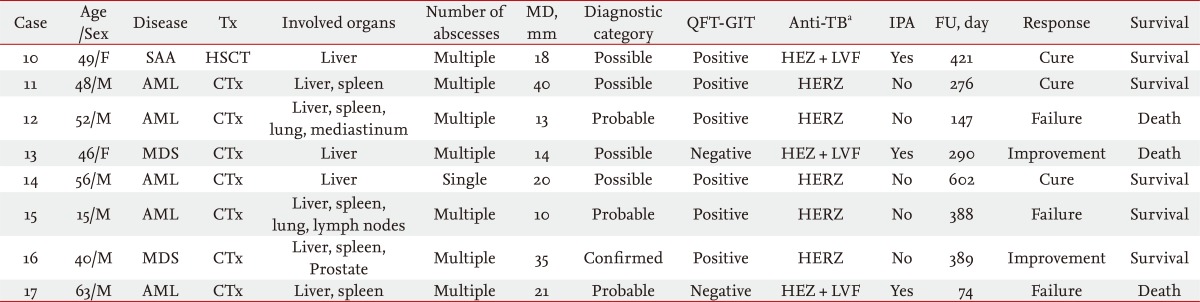
Tx, treatment; MD, maximum diameter; QFT-GIT, QuantiFERON-TB Gold In-Tube; TB, tuberculosis; IPA, invasive pulmonary aspergillosis; FU, follow-up; SAA, severe aplastic anemia; HSCT, hematopoietic stem cell transplantation; HEZ, isoniazid, ethambutol, pyrazinamide; LVF, levofloxacin; AML, acute myelogenous leukemia; CTx, chemotherapy; HERZ, isoniazid, ethambutol, rifampin, pyrazinamide; MDS, myelodysplastic syndrome.
aPyrazinamide was administered for the first 2 months.
The characteristics of the nine patients with a noninfectious origin are presented in Table 5. Three patients were newly diagnosed patients who had not undergone previous anticancer chemotherapy and one patient had relapsed with underlying non-Hodgkin's lymphoma after autologous HSCT. Pathology was available in two patients, and the final clinical diagnoses were infiltration of underlying hematologic malignancies (n = 4), hemangioma (n = 2), eosinophilic infiltration (n = 2), and simple cyst (n = 1).
Table 5.
Characteristics of the nine patients with a noninfectious origin
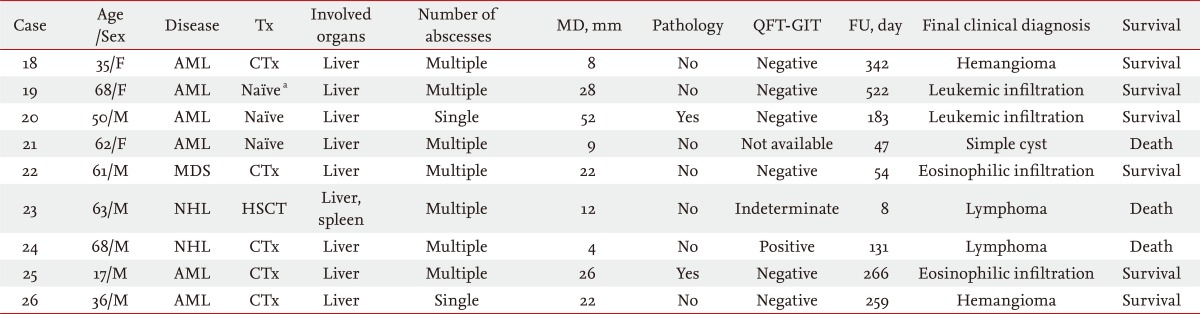
Tx, treatment; MD, maximum diameter; QFT-GIT, QuantiFERON-TB Gold In-Tube; FU, follow-up; AML, acute myelogenous leukemia; CTx, chemotherapy; MDS, myelodysplastic syndrome; HSCT, hematopoietic stem cell transplantation; NHL, non-Hodgkin's lymphoma.
aNaïve, newly diagnosed without previous anticancer chemotherapy.
QFT-GIT for the TB diagnosis
Of the 26 patients, QFT-GIT was not performed in two cases, and results were indeterminate in two cases. The QFT-GI result was positive in six of eight cases among TB patients and negative in 13 of 16 cases among patients with non-TB lesions. The sensitivity and specificity of QFT-GIT for the diagnosis of hepatosplenic TB were 75% (6/8) and 81.3% (13/16), respectively.
Outcome and cause of death
Eight patients died at the end of follow-up. The mortalities were attributable to progression of underlying hematologic malignancies (n = 5), brain hemorrhage (n = 1), heart failure with infective endocarditis by methicillin-resistant Staphylococcus aureus (n = 1), and septic shock by E. faecium bacteremia (n = 1). The overall survival rates at 8 weeks and at the last follow-up were 92.3% and 69.2%, respectively.
DISCUSSION
We add an empirical antifungal agent when a hematologic patient develops a neutropenic fever that does not respond to empirical broad spectrum antibacterial therapy for more than 4 to 7 days. The next step is to take a CT scan of the chest or, less commonly, of the abdomen. During the study period, the investigators noticed unexpected hepatic or splenic lesions in some patients on CT scans; thus we evaluated the characteristics of these lesions.
Hepatic and splenic lesions in hematologic patients of infectious and noninfectious origins were difficult to distinguish. Although hypoalbuminemia was more common in the infectious group, laboratory findings were not useful for distinguishing between infectious and noninfectious origins (Table 1). Concerns regarding postprocedural infection and bleeding limit invasive procedures. Only seven cases of infectious and two cases in the noninfectious group underwent percutaneous biopsy, drainage, or surgery. Hence, many patients received empirical antibiotic treatment and final diagnoses were usually based on other clinical information rather than definitive microbiology.
Among the 26 cases, 17 comprised the infectious group and five (29.4%) had direct microbiological evidence (Tables 3 and 4) of infection. Most patients (n = 15, 88.2%) had hepatic involvement. Patients with a pyogenic liver abscess have been reported to present with leukocytosis, elevated alkaline phosphatase, hypoalbuminemia, and elevated C-reactive protein [2,13,14]. However, only two (11.8%) had leukocytosis, eight (47.1%) had neutropenia, and seven (41.2%) had elevated alkaline phosphatase level in the present study.
Fungal liver abscesses have been reported mostly in patients with malignancies [3,15]. Marcus et al. [15] reported 17 bacterial and 20 fungal hepatic abscesses in patients with cancer. Among those with fungal abscesses, 15 (75%) had hematological malignancies and 19 (95%) had undergone prior anticancer chemotherapy. Disseminated candidiasis is a well-established etiology of fungal hepatosplenic lesions in hematologic patients. Sallah et al. [16] reviewed 23 hepatosplenic candidiasis patients with acute leukemia. Microorganisms were identified in 10 cases (43.8%), which were Candida albicans (n = 6), C. tropicalis (n = 3), and C. glabrata (n = 1). We found two probable and one possible disseminated candidiasis case, and two were positive for C. tropicalis in blood culture.
Case 8 had a large hepatic lesion consisting of a combined E. faecium abscess with fungal hyphae. Aspergillus species was considered initially because the branching hyphae had septations with acute angles, and the GM assay was positive. However, the tissue culture was negative for fungus [17]. Huang et al. [18] reported that 35 of 153 (22%) patients with a pyogenic hepatic abscesses had a concurrent fungal infection from 1973 to 1993. Hepatobiliary or pancreatic cancers were the most common associated diseases, and hematologic malignancies were not included in their study. Considering that fungal infection is not uncommon in hematologic patients, more aggressive and invasive procedures could identify combined etiologies more frequently.
Llenas-García et al. [19] investigated 22 cases of splenic abscess and reported that M. tuberculosis was the most frequent causative microorganism, accounting for eight patients (36.4%), all of whom had acquired immunodeficiency syndrome as a predisposing factor. In the present study, in which hematologic malignancy was a predisposing factor, five of 10 patients with splenic abscesses had TB followed by fungal (n = 4), and bacterial (n = 1) infections.
Primary hepatic TB is very rare and difficult to diagnose [20-22]. Chong [21] reported 14 patients (0.74%) with hepatic TB of 1,888 patients with TB over a 10-year period. Only three patients (0.16%) had isolated hepatic involvement. The overall annual incidence ranged from 0.0% to 1.05% of all TB infections. Some investigators have reported that IGRAs are useful for diagnosing E-TB, which includes TB lymphadenitis most commonly, and pleural, skeletal, central nervous system, and abdominal TB less commonly [7-9,23]. The reported sensitivities and specificities of IGRAs for the diagnosis of E-TB are 69% to 94% and 82% to 88%, collectively, and vary among disease sites [7-9]. In patients with suspected TB lymphadenitis, blood IGRA may be useful adjunct assay to diagnose or exclude E-TB [8,23], but blood IGRA alone is not useful for diagnosis of TB of the spine or central nervous system [8,24]. Previous studies included no or few, if any, hepatic or splenic TB patients and no other studies have evaluated the usefulness of the QFT-GIT for diagnosing hepatic or splenic TB in hematologic patients. In the present study, none of the patients had a history of TB, and QFT-GIT was positive in six of eight TB cases. The sensitivity and specificity of the QFT-GIT were 75% (6/8) and 81.3% (13/16). Excluding concurrent pulmonary TB, four of six cases were positive for QFT-GIT. TB should be considered for those not responding to antibacterial or antifungal drugs and the QFT-GIT may be useful in the differential diagnosis of hepatosplenic lesions in hematologic patients.
A noninfectious origin accounted for 34.6% of patients. The final diagnosis was based on a response to chemotherapy, underlying disease status, serial radiological findings, and laboratory results except for two pathologically confirmed cases. In contrast, most of the infectious group (n = 8, 88.9%) had isolated hepatic involvement.
Of the 17 infectious cases, the number of cures, improvements, and failures was nine, four, and four, respectively. Although five patients in the infectious group died during the follow-up period, hepatosplenic infections were not fatal and did not directly influence mortality. Those patients died of underlying disease progression (n = 2), another infection (n = 2), or brain hemorrhage (n = 1).
Considering the rarity of hepatosplenic TB, this study included a very small number of patients and was retrospective in nature. Thus, a larger prospective study is required to explore the usefulness of QFT-GIT in hepatosplenic TB.
In summary, causes of hepatic or splenic lesions in Korean hematologic patients are diverse and include bacterial, fungal, TB, and noninfectious origins. Meticulous diagnostic and therapeutic attempts should be made to identify the causative agent. QFT-GIT may be useful for the differential diagnosis of hepatosplenic lesions in hematologic patients, but more research is needed.
KEY MESSAGE
1. Causes of hepatosplenic lesions in hematologic patients were diverse including tuberculosis (TB), non-TB organisms, and noninfectious origins.
2. QuantiFERON-TB Gold In-Tube may be useful for differential diagnosis of hepatosplenic lesions in hematologic patients.
Footnotes
D.G. Lee received research grants from Yuhan/Gilead, is a consultant to Astellas, Janssen, MSD, and Pfizer, and has received honoraria from these companies.
References
- 1.Sherman JD, Robbins SL. Changing trends in the casuistics of hepatic abscess. Am J Med. 1960;28:943–950. doi: 10.1016/0002-9343(60)90203-5. [DOI] [PubMed] [Google Scholar]
- 2.Yoo HM, Kim WH, Shin SK, Chun WH, Kang JK, Park IS. The changing patterns of liver abscess during the past 20 years: a study of 482 cases. Yonsei Med J. 1993;34:340–351. doi: 10.3349/ymj.1993.34.4.340. [DOI] [PubMed] [Google Scholar]
- 3.Lipsett PA, Huang CJ, Lillemoe KD, Cameron JL, Pitt HA. Fungal hepatic abscesses: characterization and management. J Gastrointest Surg. 1997;1:78–84. doi: 10.1007/s11605-006-0013-y. [DOI] [PubMed] [Google Scholar]
- 4.Chen CY, Chen YC, Tang JL, et al. Hepatosplenic fungal infection in patients with acute leukemia in Taiwan: incidence, treatment, and prognosis. Ann Hematol. 2003;82:93–97. doi: 10.1007/s00277-002-0588-7. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization. Global tuberculosis control 2010 [Internet] Geneva (CH): World Health Organization; c2010. [cited 2011 Aug 22]. Available from: http://www.who.int/tb/publications/global_report/2010/en/index.html. [Google Scholar]
- 6.Mazurek GH, Jereb J, Vernon A, et al. Updated guidelines for using interferon gamma release assays to detect Mycobacterium tuberculosis infection: United States, 2010. MMWR Recomm Rep. 2010;59(RR-5):1–25. [PubMed] [Google Scholar]
- 7.Kim SH, Choi SJ, Kim HB, Kim NJ, Oh MD, Choe KW. Diagnostic usefulness of a T-cell based assay for extrapulmonary tuberculosis. Arch Intern Med. 2007;167:2255–2259. doi: 10.1001/archinte.167.20.2255. [DOI] [PubMed] [Google Scholar]
- 8.Song KH, Jeon JH, Park WB, et al. Usefulness of the whole-blood interferon-gamma release assay for diagnosis of extrapulmonary tuberculosis. Diagn Microbiol Infect Dis. 2009;63:182–187. doi: 10.1016/j.diagmicrobio.2008.10.013. [DOI] [PubMed] [Google Scholar]
- 9.Ak O, Dabak G, Ozer S, Saygi A, Dabak R. The evaluation of the Quantiferon-TB gold test in pulmonary and extrapulmonary tuberculosis. Jpn J Infect Dis. 2009;62:149–151. [PubMed] [Google Scholar]
- 10.De Pauw B, Walsh TJ, Donnelly JP, et al. Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis. 2008;46:1813–1821. doi: 10.1086/588660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liebeschuetz S, Bamber S, Ewer K, Deeks J, Pathan AA, Lalvani A. Diagnosis of tuberculosis in South African children with a T-cell-based assay: a prospective cohort study. Lancet. 2004;364:2196–2203. doi: 10.1016/S0140-6736(04)17592-2. [DOI] [PubMed] [Google Scholar]
- 12.Segal BH, Herbrecht R, Stevens DA, et al. Defining responses to therapy and study outcomes in clinical trials of invasive fungal diseases: Mycoses Study Group and European Organization for Research and Treatment of Cancer consensus criteria. Clin Infect Dis. 2008;47:674–683. doi: 10.1086/590566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pang TC, Fung T, Samra J, Hugh TJ, Smith RC. Pyogenic liver abscess: an audit of 10 years' experience. World J Gastroenterol. 2011;17:1622–1630. doi: 10.3748/wjg.v17.i12.1622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wie SH, Chang UI, Kim JD, et al. Clinical features of 141 cases of pyogenic liver abscess over a 10-year period and antibiotic sensitivity to the causative organisms. Infect Chemother. 2008;40:199–206. [Google Scholar]
- 15.Marcus SG, Walsh TJ, Pizzo PA, Danforth DN., Jr Hepatic abscess in cancer patients: characterization and management. Arch Surg. 1993;128:1358–1364. doi: 10.1001/archsurg.1993.01420240066012. [DOI] [PubMed] [Google Scholar]
- 16.Sallah S, Semelka RC, Wehbie R, Sallah W, Nguyen NP, Vos P. Hepatosplenic candidiasis in patients with acute leukaemia. Br J Haematol. 1999;106:697–701. doi: 10.1046/j.1365-2141.1999.01592.x. [DOI] [PubMed] [Google Scholar]
- 17.Hong KW, Kwon JC, Chun HJ, Lee DG, Kim HJ, Min WS. Liver abscess by Aspergillus and Enterococcus faecium in a patient with acute myeloid leukemia: a case report and literature review. Infect Chemother. 2011;43:377–381. [Google Scholar]
- 18.Huang CJ, Pitt HA, Lipsett PA, et al. Pyogenic hepatic abscess: changing trends over 42 years. Ann Surg. 1996;223:600–607. doi: 10.1097/00000658-199605000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Llenas-Garcia J, Fernandez-Ruiz M, Caurcel L, Enguita-Valls A, Vila-Santos J, Guerra-Vales JM. Splenic abscess: a review of 22 cases in a single institution. Eur J Intern Med. 2009;20:537–539. doi: 10.1016/j.ejim.2009.04.009. [DOI] [PubMed] [Google Scholar]
- 20.Chen HC, Chao YC, Shyu RY, Hsieh TY. Isolated tuberculous liver abscesses with multiple hyperechoic masses on ultrasound: a case report and review of the literature. Liver Int. 2003;23:346–350. doi: 10.1034/j.1478-3231.2003.00861.x. [DOI] [PubMed] [Google Scholar]
- 21.Chong VH. Hepatobiliary tuberculosis: a review of presentations and outcomes. South Med J. 2008;101:356–361. doi: 10.1097/SMJ.0b013e318164ddbb. [DOI] [PubMed] [Google Scholar]
- 22.Zayer S, Koberstein B, Pohle T. Hepatic lesions in an elderly woman: cancer isn't always the answer. Z Gastroenterol. 2011;49:39–41. doi: 10.1055/s-0029-1245695. [DOI] [PubMed] [Google Scholar]
- 23.Kim YK, Uh Y, Lee NS, Cho MY, Eom M, Kim HY. Whole-blood interferon-gamma release assay for diagnosis of tuberculous lymphadenitis. Tohoku J Exp Med. 2011;224:189–193. doi: 10.1620/tjem.224.189. [DOI] [PubMed] [Google Scholar]
- 24.Kim SH, Cho OH, Park SJ, et al. Rapid diagnosis of tuberculous meningitis by T cell-based assays on peripheral blood and cerebrospinal fluid mononuclear cells. Clin Infect Dis. 2010;50:1349–1358. doi: 10.1086/652142. [DOI] [PubMed] [Google Scholar]