Abstract
INTRODUCTION
Despite improvements in detection and surgical techniques perforation of the esophagus are lifethreatening. In this case report a rare presentation esophageal perforation due to Barrett's ulceration into an aortic vessel is described.
PRESENTATION OF CASE
We report a 42 year old man with known Barrett's esophagus presenting with abdominal pain. Further investigations showed an active intrathoracal hemorrhage due to esophageal perforation at exactly the same site of the known Barret's ulcer one year before. Thoracotomy with evacuation of blood was performed and an aortic branch as bleeding focus was found.
DISCUSSION
Hemothorax due to esophageal perforation of a benign Barrett's ulcer is rare. The diagnosis of aortoesophageal fistula's can be complicated and its presentation is frequently unspecific and is simply confused with other disorders. Acute thoracotomy is necessary and choice of closure depends on the cause and size of the perforation.
CONCLUSION
This case illustrates the need for maintaining a wide-ranging view of potential casus of hemothorax. The key to survival in patients with aorto-esophageal fistula is maintaining awareness of the condition to allow early diagnosis and operative management of this treatable lesion.
Keywords: Hemothorax, Esophageal perforation, Esophagus, Barrett's
1. Introduction
Esophageal perforation is a relatively rare but potentially lethal condition. Several factors, including the diversity of clinical symptoms and the proximity of vital structures, contribute to a high morbidity and a mortality rate of about 20%.1,2 Prompt radiological and endoscopic evaluation and surgical intervention are critical to minimize morbidity and mortality. Most cases of hemothorax are related to open or closed chest trauma or procedures such as central lines, thoracentesis, pleural biopsy, or catheterization and therefore anamnesis is generally suggestive for diagnosis. This case report presents an unusual presentation of esophageal perforation with hemothorax resulting from benign Barrett's ulcer perforating into an aortic vessel.
2. Case presentation
A 42-year-old man presented at the emergency room with a history of acute abdominal pain, pallor and sweating for the past 2 h. His history included infantile encephalopathy, a sliding hiatus hernia and Barrett's esophagus treated with omeprazole 40 mg daily. Due to poor swallowing function the patient received a PEG-tube 5 years previously for feeding. Endoscopy, performed one year before presentation because of melena, revealed esophageal ulceration 28 cm from the dental line, suspicious for malignancy. Biopsies showed a columnar lined (Barrret's) esophagus with ulceration but no malignant features. The patient received sucralfate in addition to omeprazole. Repeat endoscopy one month later showed complete ulcer healing. Due to buried bumper syndrome the patient received surgical insertion of a new PEG 23 days before presentation. He developed post-procedural vomiting which required placement of a jejunal extension through the PEG. Five days before presentation, the PEG-J was replaced by a PEJ because of gastric luxation of the PEG-J extension. On admission, his heart rate was 128 beats/min, blood pressure 115/72 mmHg, temperature 37.2 °C, and pulse oximetry 99% with 3 L oxygen. Chest examination showed reduced breath sounds on the right side. Abdominal examination revealed no distension but he was diffusely tender on palpation. Laboratory tests showed hemoglobin level of 7.7 mmol/L; hematocrit of 0.39 L/L; white blood cell count 16.7 nL−1; thrombocytes 647 nL−1, C-reactive protein (CRP) 18 mg/L, and amylase 86 IU/L. Liver and renal function were normal. Arterial blood gas analysis was normal although serum lactate was 3.6 mmol/L. Chest X-ray showed a hydrothorax on the right side (Fig. 1).
Fig. 1.
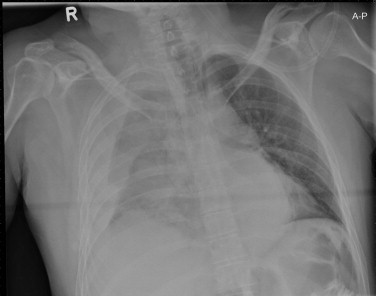
Right hydrothorax.
During admission the patient vomited once, with slight blood visible. Endoscopy demonstrated a small esophageal ulcer at 29 cm with a blood clot. The patient was admitted to intensive care as he developed signs of hemorrhagic shock with a drop in hemoglobin level to 4 mmol/L. Following stabilization in intensive care, a computed tomography (CT) scan of the thorax showed pleural fluid on the right side suggestive of blood. A blush from the thoracic aorta suggested active intrathoracic hemorrhage (Figs. 2 and 3). Immediately, a right lateral thoracotomy was performed which revealed 3 L of retained blood and clots. Inspection of the left chest revealed a 1-cm anterior esophageal perforation. Next to this perforation a direct branch of the aorta was identified as the bleeding focus. Hemostasis was achieved using Prolene sutures. After passing of a nasogastric tube, the esophageal perforation was closed primarily with polydiaxonane and Floseal was left. Active thoracic drainage with negative suction pressure and mediastinal passive drainage was performed. The patient received cefuroxime/metrodinazole for four weeks postoperatively. The patient went home after six weeks. Six weeks after admission an endoscopy revealed a small residual esophageal ulcer. Pathologic examination of biopsy specimens from the ulcer margin revealed again columnar lined (Barret's) esophagus with benign ulceration. Follow-up after 12 weeks showed healing of the ulcer with some columnar irregular scar tissue without signs of malignancy.
Fig. 2.

Anterior displacement of mediastinal structures due to a massive hematoma from the trachea bifurcation to diaphragm. The bleeding focus coming out of the aorta is clearly seen (arrow).
Fig. 3.

Arrow: blush coming out of the aortic vessel (arrow).
3. Discussion
Esophageal perforations are life-threatening. Leakage of esophageal and gastric contents into the mediastinum creates a necrotizing inflammatory process that can lead to sepsis, multiorgan failure, and death.1,2 A high index of clinical suspicion is a prerequisite for prompt diagnosis and early therapeutic intervention to reduce morbidity and mortality. Esophagus perforation often is iatrogenic due to endoscopic procedures followed by Boerhaave syndrome and traumatic perforation caused by accidentally swallowed foreign bodies.1,2 In our patient the gastro-endoscopic procedures could have been a predisposing factor in the development of this severe complication. However this seems a less likely explanation than spontaneous perforation because of presentation of the ulcer at the exact same site one year earlier.
About 30% of esophageal ruptures are spontaneous, which can be related to intense vomiting causing an increase in intra-abdominal pressure.1,2 This clinico-pathologic entity, described by Hermann Boerhaave in 1724, is called Boerhaave syndrome. Phelan et al. described a 78-year-old man with postemetic esophageal rupture presenting with a massive left hemothorax.3 In Boerhaave's syndrome the tear mostly occurs at the left posterolateral aspect of the distal esophagus just superior to the diaphragm and extends for several centimeters.3
Barrett's esophagus is the condition in which a metaplastic columnar epithelium that predisposes to cancer development replaces the stratified squamous epithelium that normally lines the distal esophagus. The metaplastic epithelium is acquired as a consequence of chronic gastroesophageal reflux disease (GERD). Frequently, bleeding events as complication of Barret's ulcer are seen, and range from massive hematemesis to occult bleeding with chronic anemia and iron deficiency. Perforation of Barrett's ulcer is rare. Guillem et al. reviewed 34 patients with a perforated benign Barrett's ulcer. They show penetration into mediastinal structures adjacent to the esophagus, such as the pleural cavity, left atrium, tracheobronchial tract, the aorta or its branches, pericardium, and pulmonary vein.4 In our patient the artery could be aberrant or may have been a segmental esophageal artery possibly hypertrophied from the surrounding inflammation. Aortoesophageal fistulas are mostly caused by thoracic aneurysms or malignancy.5 Few cases of aortoesophageal fistulas resulting from a perforation of an esophageal ulcer developed within Barrett's mucosa are described in the literature. The diagnosis can be complicated and its presentation is frequently unspecific and is simply confused with other disorders. These patients presented with massive upper gastro-intestinal hemorrhage in contrast to our patient were no active bleeding was seen during endoscopy. None of these patients were known to have a Barrett's ulcer.4,6–8 As in our patient, they describe a symptom free interval during which the patient is stable to undergo diagnostic and therapeutic procedures. This can be explained by spasm of the arterial wall, hypotension or occlusion of the fistula by clot which is later digested by infection or gastrointestinal contents.5,7
Management of aortoesophageal fistula includes surgical repair of both aorta and esophagus, most convenient to be reached with thoracic approach, and high dose broad spectrum antibiotic coverage.4–8 The basic approaches are primary repair, possibly supported by a local tissue flap, and esophageal exclusion with synchronous or delayed gastric or colon interposition. Compared to fistulas based on aortic aneurysm, generally there is no need for grafts to be inserted in an infected surgical field.4 In cases of perforated Barrett's ulcer, esophageal resection is advised as it removes the underlying esophageal disease. However, this procedure has a high morbidity rate.4,5 Our patient was treated with primary closure because of the small defect with no esophageal necrosis and relatively simply closure of the bleeding site from the artery. Even with appropriate management, the mortality of this rare condition remains high.5–8
Conflict of interest
None declared.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient and his legal guardian for publication of this Case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Author contributions
All contributed.
References
- 1.Bhatia P., Fortin D., Inculet R.I., Malthaner R.A. Current concepts in the management of esophageal perforations: a twenty-seven year Canadian experience. Annals of Thoracic Surgery. 2011;92(1):209–215. doi: 10.1016/j.athoracsur.2011.03.131. [DOI] [PubMed] [Google Scholar]
- 2.Vallböhmer D., Hölscher A.H., Hölscher M. Options in the management of esophageal perforation: analysis over a 12-year period. Diseases of the Esophagus. 2010;23(3):185. doi: 10.1111/j.1442-2050.2009.01017.x. [DOI] [PubMed] [Google Scholar]
- 3.Phelan H.A., Brakenridge S.C., Rutland T.J., Maltese C. Boerhaave syndrome presenting as massive hemothorax. Southern Medical Journal. 2009;102(2 (February)):202–203. doi: 10.1097/SMJ.0b013e318186be00. [DOI] [PubMed] [Google Scholar]
- 4.Guillem P.G., Porte H.L., Saudemont A., Quandalle P.A., Wurtz A.J. Perforation of Barrett's ulcer: a challenge in esophageal surgery. Annals of Thoracic Surgery. 2000;69:1707–1710. doi: 10.1016/s0003-4975(00)01310-2. [DOI] [PubMed] [Google Scholar]
- 5.Reardon M.J., Brewer R.J., LeMaire S.A., Baldwin J.C., Safi H.J. Surgical management of primary aortoesophageal fistula secondary to thoracic aneurysm. Annals of Thoracic Surgery. 2000;69:967–970. doi: 10.1016/s0003-4975(99)01087-5. [DOI] [PubMed] [Google Scholar]
- 6.Guillem P.G., Porte H.L., Techer E., Wurtz A. Aortoesophageal fistula of uncommon origin: perforation of a Barrett's ulcer. Diseases of the Esophagus. 2003;16(3):259–260. doi: 10.1046/j.1442-2050.2003.00339.x. [DOI] [PubMed] [Google Scholar]
- 7.Katyal D., Jewell L.D., Yakimets W.W. Aorto-esophageal fistula secondary to benign Barrett's ulcer: a rare cause of massive gastrointestinal hemorrhage. Canadian Journal of Surgery. 1993;36:480–482. [PubMed] [Google Scholar]
- 8.Borrie J., Goldwater L. Columnar cell-lined esophagus: assessment of etiology and treatment. A 22 year experience. Journal of Thoracic and Cardiovascular Surgery. 1976;71:825–834. [PubMed] [Google Scholar]


