Abstract
INTRODUCTION
Morgagni's hernia is a congenital herniation of abdominal viscera into the thoracic cavity through a retrosternal diaphragmatic defect.
PRESENTATION OF CASE
We present a case of incarcerated Morgagni hernia in a 69-year-old woman. Three years previously, she had undertaken a video-assisted thoracoscopic resection (VATS) of a mediastinal mass, which had been mistaken for a lipoma. Following the primary repair of the hernia at emergency laparotomy, the patient was discharged home uneventfully.
DISCUSSION
Irrespective of the radiologically characteristic findings of our case, the possibility of Morgagni hernia had not been entertained at the first operation. Thorough exploration around the diaphragm at the first VATS operation could have revealed the Morgagni hernia, ultimately avoiding the hernia-related complication such as an incarceration.
CONCLUSION
Morgagni hernia as a differential diagnosis in case of anterior mediastinal mass should not be missed.
Keywords: Morgagni, Hernia, Diaphragm, Incarceration, Mediastinal tumor
1. Introduction
Morgagni hernias are usually asymptomatic and often found incidentally on chest radiography. Symptoms of these hernias are attributable to the herniated viscera. We experienced an incarcerated Morgagni hernia, which had been overlooked and mistaken for a mediastinal lipoma previously.
2. Presentation of case
A 69-year-old obese female was transferred to our hospital with the tentative diagnosis of incarcerated diaphragmatic hernia from the referring hospital. The patient had undertaken video-assisted thoracoscopic resection of an anterior mediastinal mass 3 years before. She complained of disproportionately severe epigastric pain with sudden onset. On physical examination, her abdomen was slightly distended with remarkable tenderness. The chest X-ray revealed intestinal gas above the right diaphragm, which was also confirmed by the CT scan (Fig. 1). Having made the diagnosis of incarcerated diaphragmatic hernia, emergency laparotomy was performed through an upper midline incision. The jejunum was incarcerated into the right chest cavity through the retrosternal defect of about 30 mm in diameter, which was consistent with the foramen of Morgagni (Fig. 2). Fortunately, there was almost no ischemic change of the incarcerated intestine, which was replaced into the peritoneal cavity. The defect was repaired with 3-0 silk interrupted sutures. The postoperative course was uneventful.
Fig. 1.
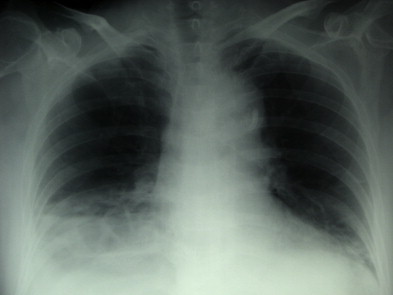
The intestinal gas observed above the right diaphragm.
Fig. 2.
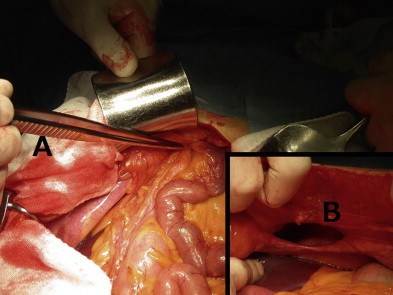
(A) The tip of the forceps pointing the incarceration of the jejunum through the hernia. (B) The defect of about 30 mm in diameter.
3. Discussion
Since 1769 when Morgagni first described the substernal herniation of the abdominal viscera into the chest cavity on autopsy examinations, Morgagni hernias have been rare entities in the general population.1 The incidence of congenital diaphragmatic hernias is estimated to be 1 in between 2000 and 5000 births. Morgagni hernia comprises 2% of diaphragmatic hernias.2 According to the report from the Massachusetts General Hospital in 2004, 50% of patients with Morgagni hernia were asymptomatic with a slight predominance of males. The average age at diagnosis was 42 years. 90% of the hernias were right-sided.1
The most common contents of the hernia were the omentum, followed by the colon, small intestine, and stomach.3
To make an accurate diagnosis, chest X-rays and CT scans are useful. Chest X-rays are the first choice for radiological evaluations of a diaphragmatic hernia. CT scans are more effective as a large paracardiac fat density with linear densities consistent with omental blood vessels and an abnormally high location of the transverse colon are radiological characteristics of Morgagni hernia.4 Differential diagnosis should be made between pleuropericardial cysts, lipomas, liposarcoma, mesothelioma, pericardial fat mass, diaphragmatic cysts, and thymoma.3,5,6
To avoid unnecessary patient morbidity, for example, incarceration with bowel obstruction, the prompt surgical repair of the foramen of Morgagni is of paramount importance. The longer the period between diagnosis and repair, the more the number of symptomatic patients have increased as in our case.1 Generally, repair of Morgagni hernias can be undertaken either trans-thoracically or trans-abdominally. Trans-abdominal repair of the hernia either via laparotomy or laparoscopy is safe and secure in complicated hernia (incarceration and strangulation) because entire abdominal exploration is necessary.7
In our case, at the first operation we never thought of Morgagni hernia as a differential. The chest images for the first operation showed right well-delineated pericardial mass with linear densities, which findings are characteristics of Morgagni hernia (Fig. 3). If we had explored around the diaphragm more thoroughly with the possibility of Morgagni hernia in mind at the first VATS operation, we would have detected the defect and performed primary repair of the hernia.
Fig. 3.
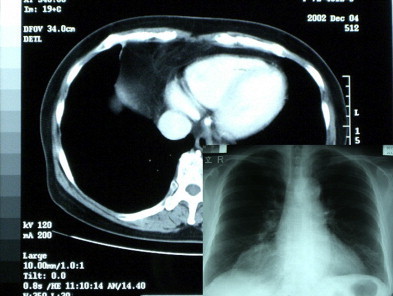
The chest X-ray and CT scan showing the cardiophrenic fat mass with linear densities consistent with omental blood vessels.
4. Conclusion
Morgagni hernia should be kept in mind as a differential diagnosis regarding anterior mediastinal mass, and it should be easy to diagnose preoperatively due to its characteristic radiological findings. Complicated Morgagni hernias should be repaired using the trans-abdominal approach.
Conflict of interest statement
None.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contributions
Dr. Teruya Komatsu is the corresponding author, and Dr. Yutaka Takahashi has cooperated in writing the manuscript and supervised the case analysis.
Disclosure statement
We, the authors, disclose that we have not received any payment or services from a third party for any aspect of the submitted work (including but not limited to grants, data monitoring board, study design, manuscript preparation, statistical analysis, etc.) and that we do not have any financial relationships (regardless of amount of compensation) with any entities.
References
- 1.Minneci P.C., Deans K.J., Kim P., Mathisen D.J. Foramen of Morgagni hernia: changes in diagnosis and treatment. Annals of Thoracic Surgery. 2004;77(6):1956–1959. doi: 10.1016/j.athoracsur.2003.12.028. [DOI] [PubMed] [Google Scholar]
- 2.Comer T.P., Clagett O.T. Surgical treatment of hernia of the foramen of Morgagni. Journal of Thoracic and Cardiovascular Surgery. 1966;52(4):461–468. [PubMed] [Google Scholar]
- 3.Yilmaz M., Isik B., Coban S., Sogutlu G., Ara C., Kirimlioglu V. Transabdominal approach in the surgical management of morgagni hernia. Surgery Today. 2007;37(1):9–13. doi: 10.1007/s00595-006-3336-0. [DOI] [PubMed] [Google Scholar]
- 4.Fagelman D., Caridi J.G. CT diagnosis of hernia of Morgagni. Gastrointestinal Radiology. 1984;9(2):153–155. doi: 10.1007/BF01887823. [DOI] [PubMed] [Google Scholar]
- 5.Gossios K.J., Tatsis C.K., Lykouri A., Constantopoulos S.H. Omental herniation through the foramen of Morgagni. Diagnosis with chest computed tomography. Chest. 1991;100(5):1469–1470. doi: 10.1378/chest.100.5.1469. [DOI] [PubMed] [Google Scholar]
- 6.Kamiya N., Yokoi K., Miyazawa N., Hishinuma S., Ogata Y., Katayama N. Morgagni hernia diagnosed by MRI. Surgery Today. 1996;26(6):446–448. doi: 10.1007/BF00311935. [DOI] [PubMed] [Google Scholar]
- 7.Kesieme E.B., Kesieme C.N. Congenital diaphragmatic hernia: review of current concept in surgical management. ISRN Surgery. 2011;2011:974041. doi: 10.5402/2011/974041. [DOI] [PMC free article] [PubMed] [Google Scholar]


