Abstract
INTRODUCTION
Tailgut cysts or retrorectal cystic hamartomas are rare developmental anomalies that are believed to arise from the embryonic hindgut.
PRESENTATION OF CASE
9 months old male infant was presented with swelling in the right gluteal region. MRI lumbo-sacral spine showed well defined round to oval lesion which is brightly hypertense on T2W1 and hypotense on T1W1 posterior to sacrum and coccyx with no evidence of connection to the thecal sac indicating cyst. Complete excision of the cyst was done. Histopathology report shows cyst wall partially lined with stratified squamous epithelium and cyst wall shows spaces lined by cuboidal epithelium and nerve bundles with no evidence of malignancy suggestive of tailgut cyst.
DISCUSSION
Tailgut cysts are rare congenital anomalies. Most commonly located in the retrorectal space. They are thought to be derived from the remnants of the embryonic hindgut. Age ranges from 4 to 73 years but an average presentation is at 35 years. Female to male ratio is 3:1. MRI is a good diagnostic tool for diagnosis of tailgut cyst. Complete surgical excision is the treatment of choice as this provides a definite diagnosis and prevents possible complications such as infection, fistula formation and malignant degeneration.
CONCLUSION
The aim of presenting this case is its rarity. Complete surgical excision is the treatment of choice. Preoperative imaging with MRI is essential to plan the most appropriate surgical approach.
Keywords: Tailgut cyst, Retrorectal cystic hamartomas, Rarity
1. Introduction
Tailgut cysts are rare congenital anomalies. Most commonly located in the retrorectal space. They are thought to be derived from the remnants of the embryonic hindgut (postanal gut). Age ranges from 4 to 73 years but an average presentation is at 35 years with 3:1 female to male ratio. MRI is a good diagnostic tool for diagnosis of tailgut cyst. Complete surgical excision is the treatment of choice for tailgut cyst as this provides a definite diagnosis to rule out malignancy and prevents possible complications such as infection, fistula formation and malignant degeneration.
2. Case report
9 months old male infant was presented with swelling in the right gluteal region since 6 months. It was a full term normal baby with birth weight of 2.5 kg. Clinical examination showed well nourished baby, vitally stable. Local examination showed a swelling in the right gluteal region 5 cm × 3 cm. On digital rectal examination no mass was palpable. Other systems were essentially normal. Laboratory investigations were within normal limits. X-ray lumbosacral spine did not show any abnormality. Ultrasonography showed 4.5 cm × 2.5 cm × 0.5 cm unilocular hypoechoic lesion posterior to sacrum and coccyx. MRI lumbo-sacral spine showed well defined round to oval lesion which is brightly hypertense on T2W1 and hypotense on T1W1 posterior to sacrum and coccyx with no evidence of connection to the thecal sac indicating cyst. Complete excision was done through posterior approach up to coccyx. Histopathology report shows cyst wall partially lined with stratified squamous epithelium and wall shows spaces lined by cuboidal epithelium and nerve bundles with no evidence of malignancy suggestive of tailgut cyst. Broad spectrum antibiotics were given and careful monitoring of vital organs was done. His post operative period was uneventful. He was discharged after 15 days. Patient was followed on Out Patient Department basis without any complications post operatively.
3. Discussion
Tailgut cysts are rare congenital lesions that almost invariably occur in retrorectal space but can also occur in prerectal1 and perirenal locations.2 The differential diagnosis can be classified as congenital, neurogenic, osseous, miscellaneous and inflammatory. Excluding the inflammatory processes, congenital lesions account for approximately two-thirds of retrorectal lesions.3 These include developmental cysts, chordomas, and anterior sacral meningoceles. Developmental cysts can further be divided according to their origin and histopathological features into tailgut cysts, enteric duplication cysts, dermoid cysts, epidermoid cysts, and teratomas.
Embryologically, tailgut cysts are believed to arise from vestigial remnants of the embryonic hindgut. The embryo possesses a true tail during early human development which is maximal at the 8 mm stage (35 days gestational age). It is hypothesized that remnants of the tailgut that fail to regress may lead to the subsequent formation of tailgut cysts.4,5 Female to male ratio is 3:1. The ages ranged from 4 days to 73 years with an average age at 35 years. Patients may present with low back pain or rectal pain, pain during defecation, rectal fullness, painless rectal bleeding, change in caliber of stool, urinary frequency, etc. In asymptomatic patients most lesions are detected incidentally. Almost all are palpable on rectal examination as extrinsic, contained fluctuant masses.3,4 The diagnosis is often delayed due to the unfamiliarity with this entity and because the symptoms associated with it mimic other more commonly occurring pathologies at this site.6
Plain films, colonoscopy, barium enema, transrectal ultrasound, CT imaging may be useful. MRI has become the modality of choice. MR imaging typically demonstrates a retrorectal lesion with low signal intensity on T1-weighted images and high signal intensity on T2-weighted images although it may vary according to the content. Malignancy is suspected if there is focal irregular wall thickening and intermediate signal intensity before contrast on both T1 and T2 weighted images with enhancement after contrast.5,7 Preoperative biopsy is indicated if there is a suspicion of malignancy and avoided if benign or cystic (Figs. 1–4).
Fig. 1.

MRI lumbo-sacral spine showing well defined hypotense on T1W1, round to oval lesion posterior to sacrum and coccyx.
Fig. 2.

MRI lumbo-sacral spine showed well defined round to oval lesion, brightly hypertense on T2W1.
Fig. 3.
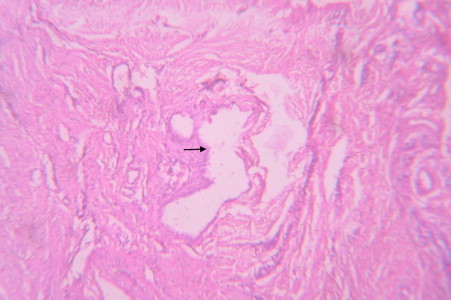
Cyst wall partially lined with cuboidal epithelium.
Fig. 4.

Showing nerve bundles and muscle fascicles.
Complete surgical excision is recommended to avoid recurrence, alleviate symptoms, prevent infection and potential local dissemination of malignant cells. Different surgical approaches are there like posterior approach, abdominal approach, or a combination of two. Posterior approach is recommended for small benign lesions below level of S3. If the superior border can be palpated on digital rectal examination then posterior approach is taken. Every attempt should be made to preserve the sacral nerve roots but if it is necessary to resect them then unilateral preservation of S2–4 should maintain normal bladder and bowel function.8 Cysts that have their lowest extent above the level of the S4 vertebrae should be approached transabdominally.9 Recent case reports have demonstrated laparoscopic excision of these lesions to be safe and effective approach. Tailgut cysts greater than 4–5 cm are best approached through a combined or abdominosacral approach. This is also true for lesions that extend above and below the level of the S3. There is no standard recommendation for the follow-up of the tailgut cysts. It should be clinical and case specific. If in doubt cross-sectional imaging should be done.
4. Conclusion
The aim of presenting this case is its rarity. Complete surgical excision is the treatment of choice for tailgut cyst as this provides a definite diagnosis and prevents possible complications such as infection, fistula formation and malignant degeneration. Preoperative imaging with MRI is essential to plan the most appropriate surgical approach.
Conflict of interest
None.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contributions
Abstract was written by Vinayak Raje. Data were analysed by Vaishali Raje. Presentation of the case was done by Rahul K. Patil.
Tejas D. Chotai was responsible for the Introduction part. Aditya R. Punamiya was responsible for Discussion and References. Manuscript was written by Dilrag S. Dhindsa. J.V. Wadar was responsible for the figures.
Acknowledgement
We are thankful to Dr. A.Y. Kshirsagar, Medical Director for his help and support.
References
- 1.Jang S.H., Jang K.S., Song Y.S., Min K.W., Han H.X., Lee K.G. Unusual prerectal location of a tailgut cyst: a case report. World Journal of Gastroenterology. 2006;12(31):5081–5083. doi: 10.3748/wjg.v12.i31.5081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sung M.T., Ko S.F., Niu C.K., Hsieh C.S., Huang H.Y. Perirenal tailgut cyst (cystic hamartoma) Journal of Pediatric Surgery. 2003;38(9):1404–1406. doi: 10.1016/s0022-3468(03)00408-1. [DOI] [PubMed] [Google Scholar]
- 3.Jao S.W., Beart R.W., Spencer R.J. Retrorectal tumors: Mayo Clinic experience, 1960–1979. Diseases of the Colon and Rectum. 1985;28(9):644–652. doi: 10.1007/BF02553440. [DOI] [PubMed] [Google Scholar]
- 4.Hjermstad B.M., Helwig E.B. Tailgut cysts. Report of 53 cases. American Journal of Clinical Pathology. 1988;89(2):139–147. doi: 10.1093/ajcp/89.2.139. [DOI] [PubMed] [Google Scholar]
- 5.Au E., Anderson O., Morgan B., Alarcon L., George M.L. Tailgut cysts: report of two cases. International Journal of Colorectal Disease. 2009;24(3):345–350. doi: 10.1007/s00384-008-0598-6. [DOI] [PubMed] [Google Scholar]
- 6.Prasad A.R., Amin M.B., Randolph T.L., Lee C.S., Ma C.K. Retrorectal cystic hamartoma: report of 5 cases with malignancy arising in 2. Archives of Pathology and Laboratory Medicine. 2000;124(5):725–729. doi: 10.5858/2000-124-0725-RCH. [DOI] [PubMed] [Google Scholar]
- 7.Aflalo-Hazan V., Rousset P., Mourra N., Lewin M., Azizi L., Hoeffel C. Tailgut cysts: MRI findings. European Radiology. 2008;18(11):2586–2593. doi: 10.1007/s00330-008-1028-4. [DOI] [PubMed] [Google Scholar]
- 8.Bohm B., Milsom J.W., Fazio V.W., Lavery I.C., Church J.M., Oakley J.R. Our approach to the management of congenital presacral tumors in adults. International Journal of Colorectal Disease. 1993;8(3):134–138. doi: 10.1007/BF00341185. [DOI] [PubMed] [Google Scholar]
- 9.Hassan I., Wietfeldt E.D. Presacral tumors: diagnosis and management. Clinics in Colon and Rectal Surgery. 2009;22(2):84–93. doi: 10.1055/s-0029-1223839. [DOI] [PMC free article] [PubMed] [Google Scholar]


