Abstract
INTRODUCTION
Tube decompression of the duodenum is an old but underutilized technique known to decrease morbidity and mortality in patients with difficult to manage duodenal injuries. Broad arrays of techniques have been described in the literature and are reviewed, but most are complex procedures not appropriate for the management of an unstable patient.
PRESENTATION OF CASE
In this paper we describe the technique of tube duodenostomy and the successful application in three cases of large defects (>3 cm) which two of these cases had failed previous repair attempts. The defects were caused by very different etiologies, including blunt trauma, peptic ulcer disease and erosion from cancer. All were finally managed by application of tube duodenostomy with success.
DISCUSSION
Patients with “difficult to manage duodenum” usually present with hemodynamic instability with hostile abdomen. Complex procedures in an unstable patient are associated with adverse outcomes. In patients with significant comorbidities and instability the damage control principle of trauma surgery is gaining popularity. Tube duodenostomy technique described in this paper fits in well with that principle.
CONCLUSION
Application of tube duodenostomy instead of a complex procedure in an unstable patient provides an opportunity to stabilize the patient, converting an impending catastrophe to a future scheduled surgery.
Keywords: Duodenal injury, Tube duodenostomy
1. Introduction
Complex duodenal injuries pose a significant challenge to the general surgeon. On one hand, they are relatively rare injuries, thus rendering it unlikely that most practicing surgeons would have extensive experience managing these cases. On the other hand, the consequences of inadequate repair can be devastating, leading to delayed leaks, widespread abdominal contamination, sepsis and death.1–3
Simple duodenal perforations usually result from peptic ulcer disease or endoscopic intervention, and can be treated with primary repair or with an omental patch.4 In contrast, multiple procedures have been described for large duodenal perforations, ranging from drainage and pyloric exclusion to pancreaticoduodenectomy.5–8 While effective, many of these operations are technically demanding and require long operative times, neither of which are ideal for patients presenting with sepsis who are often hemodynamically unstable and manifesting shock physiology by the time the diagnosis has been made.9,10 Thus the ideal repair would be simple, easily learned and able to be performed quickly in a damage-control fashion.
Tube decompression of the duodenum was initially utilized in management of the duodenal stump after gastrectomy, in order to prevent blow-out of the duodenal stump at the suture line.11 Through the years tube duodenostomy has proven to be an effective and safe technique in the management of the difficult duodenal injury.12 Despite good outcomes it has not gained universal acceptance and has been underutilized. Recently a limited number of case series have been published on the application of tube duodenostomy in the management of giant duodenal ulcers and traumatic injuries.12–15
In this paper we present the basic technique of tube duodenostomy, and three cases of large (>3 cm) defects from very different etiologies, including blunt trauma, peptic ulcer disease and erosion from cancer, in which this method was used. Two of these cases had previous failed attempts at repair. All cases were successfully managed by tube duodenostomy, with or without concomitant pyloric exclusion, thus highlighting the broad applicability of this simple technique in managing a very vexing surgical problem.
2. Operative technique
Tube duodenostomy is a simple technique, does not involve an anastomosis and is easy to perform. After mobilization of the right colon and exposure of the lateral and anterior walls of the duodenum (Kocherization) to provide good visualization, the extent of the defect is ascertained. A 20F Malencot's catheter is inserted into the duodenum to decompress the lumen. If a tension free primary approximation of the edges is feasible but there is a high risk of leakage due to the injury mechanism or size, the catheter is placed in the middle of the repair and the edges are approximated carefully on either side. If the edges of the defect are unable to be closed without a tension free repair or if there is gross inflammation in the area with friable tissue, the Malecot's catheter may be inserted through the defect and secured with a purse string suture. We recommend use of a monofilament suture; a 3-0 polydioxenone suture (PDS) was used in the cases presented. A piece of omentum may be wrapped and secured around the base of the tube to help seal the defect if desired. In both scenarios the area should be drained with an additional flat drain placed along side of the repair (Figs. 1 and 2). To prevent gastric emptying to the duodenum a pyloric exclusion procedure may be added or a draining gastrostomy tube may be placed. Finally a feeding jejunostomy is placed for enteral nutritional support. The duodenal drain should be left in place for a minimum of 6 weeks in order for a defined track to develop, similar to the use of T tubes in bile duct injuries. Once the patient has recovered from their initial hospital course and the appropriate time has lapsed, the tube is clamped for 2–3 days to ensure that there are no adverse sequelae; the tube is then pulled and a dry dressing applied over the skin site which heals within a few days. In our experience we have not found it necessary to perform imaging studies through the duodenostomy tube prior to removal.
Fig. 1.
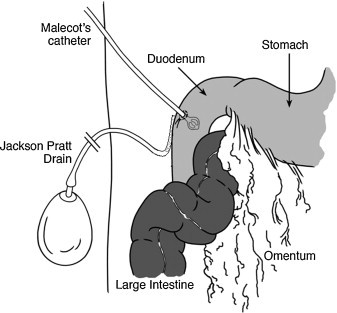
Tube duodenostomy in place within the duodenum with adjacent suction drainage catheter.
Fig. 2.
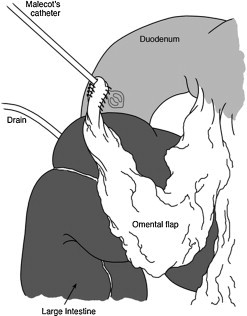
Omental flap placed around exit site of the tube in the duodenum to prevent leakage around the site and further secure the drain in place.
2.1. Case #1: delayed diagnosis of duodenal injury following blunt trauma
A 62 year male was involved in a motor cycle accident that resulted in a high cervical cord injury with quadriplegia. He was treated with high dose steroids in the first 24 h for spinal cord protection. The patient did not have abdominal pain or tenderness on presentation, and the initial computed tomography (CT) scan was negative for intra-abdominal injury.
On day 4 he developed leukocytosis, abdominal distention and fever. Repeat CT of the abdomen and pelvis with oral contrast revealed extravasation of contrast near the first part of the duodenum (see Fig. 1). At operation a 3.5 cm laceration of the first part of the duodenum on the mesenteric side was found. The laceration was fixed primarily with interrupted 3-0 silk suture and a gastrostomy tube and feeding jejunostomy tube were placed. Two large drains were placed anterior and posterior to the duodenal repair prior to abdominal closure. Although his immediate post-operative recovery was uneventful, on post-operative day 5 (post-injury day 10) the patient suddenly became hemodynamically unstable with respiratory failure requiring reintubation and mechanical ventilation. An esophagogastroduodenoscopy was performed which revealed bleeding at the site of duodenal repair. This finding was confirmed at operation, in addition to discovery of a leak and failure of the initial repair. A pyloric exclusion was performed as described by Vaughan et al.8 with tube duodenostomy placed for proximal decompression of the duodenum. The previous surgery had already established feeding access and drainage of the stomach. He suffered no further sequelae from the surgery and was transferred to a long term care facility.
2.2. Case #2: psuedomyxoma peritonei of the duodenum
A 53 year old man with a history of perforated appendiceal carcinoma treated with right hemicolectomy and adjuvant chemotherapy one year previously presented with recurrent abdominal fullness, distention and early satiety. CT scan demonstrated a large fluid collection in the right abdomen near the site of previous surgery (Figure X) which biopsy confirmed was a recurrent mucinous adenocarcinoma, suggestive of pseudomyxoma peritoneii. The patient opted for an attempt at debulking surgery, which revealed recurrence of cancer at the previous ileocolonic anastomosis, extending into the retroperitoneum and the second part of the duodenum. The anastomosis was resected and a new anastomosis was made with cancer free margins. Upon debulking of the tumor at the second part of the duodenum it was realized that the tumor had eroded the anterior wall of the duodenum, leaving a 3 cm defect after debulking. A tube duodenostomy was placed in the defect and secured with 3-0 PDS purse string suture. A gastrojejunostomy was created for proximal diversion of gastrointestinal content away from the duodenum, as well as to allow oral feeding for palliation, and his abdomen was closed. He was discharged home on post-operative day seven with duodenostomy tube in place, on a regular diet and with good return of bowel function. The duodenostomy tube was able to be removed in clinic after 6 weeks, and the patient tolerated a regular diet until his death from metastatic cancer 6 months after the operation.
2.3. Case #3: duodenal perforation from high dose steroids for encephalitis
A 39 year old man presented to the hospital with altered mental state and decreased consciousness. He was diagnosed with Hashimoto's encephalitis and treated with high dose intravenous steroids. Eight days after admission he developed bloody nasogastric output and increased abdominal distention. A radiograph revealed free air under the diaphragm, resulting in operative exploration where a small duodenal bulb perforation was discovered. This was repaired with a Graham Patch and a gastrostomy–jejunostomy tube was placed for simultaneous decompression and feeding. His post-operative course was further complicated by renal failure. Routine contrast study on post-operative day five revealed extravasation of contrast at the previous repair site (Figure Y). At re-operation the patient was found to have four new perforations at the duodenal bulb near the previous Graham patch site. A pyloric exclusion was performed with 90 mm TL stapler, 28 French Pezzer tube duodenostomy placed, and exchange of a Moss tube for a simple gastrostomy tube. The patient's abdomen was left open for 24 h due to large amount of enteric content in the peritoneal cavity and taken back to the OR for abdominal washout, placement of feeding jejunostomy tube, placement of right upper quadrant drains, and closure of fascia. He was transferred to a long term care facility tolerating jejunal tube feeds with no further complications.
3. Discussion
The value of tube decompression of the duodenum was initially shown in 1954 for the management of the duodenal stump after gastrectomy.16 Duodenal stump leak is the most dreaded complication of gastrectomy operations, and in early reviews presented with a mortality rate as high as 50%.17 For many decades tube duodenostomy was demonstrated as a successful method managing the difficult duodenum; however it has not gained wide popularity.18 Complex duodenal injuries are more prone to leaks after repair than duodenal stumps after gastrectomy. Although the majority of duodenal perforations can effectively be managed by simple repair, complicated procedures are needed for complex injuries.19 This is also true for perforations of the duodenum due to peptic ulcer disease.20
There is no clear cut definition to what should be classified as a complex duodenal perforation and if and when to use extensive surgery for repair. For traumatic injuries, there is a de facto approach as to classify AAST-OIS grade III or greater injuries as complex duodenal injuries. Blunt trauma, bullet wounds, delayed diagnosis exceeding 24 h, and injuries to the second portion of the duodenum frequently cause surgeons to consider complex repairs.21–23 In the case of peptic ulcer disease perforations larger than 2 cm have been shown to have higher leak rates (up to 15%) with primary repair, with an associated mortality of 10–35% increasing with delay in re-exploration.4,20,24,25
Many surgical options have been described for the treatment of the “difficult to manage” duodenum. Small bowel serosal patching,6 Roux en Y duodeno jejunostomy,7 pylorus exclusion and gastrojejunostomy,8 pancreas preserving duodenectomy5 and ultimately the Whipple operation26 have all been successfully used in this situation; however each of these techniques also has drawbacks when applied to this patient population. Among these operations jejunal serosal patching is relative simple, and is performed by suturing a loop of jejunum to cover the duodenal defect. Although this procedure has shown promising results in animal models, several series have failed to show difference in morbidity and mortality compared to primary repair.6,27 Pyloric exclusion with primary repair has been extensively employed in the management of duodenal defects, and recent studies have found no difference in mortality compared to primary repair30; however it has also been shown to increase hospital stay without any contribution to the reduction of abdominal septic complications.31 Pancreas preserving duodenectomy have been advocated as an alternative to the standard Whipple operation in cases of complex duodenal injuries. Preservation of the pancreas, reduction in the number of anastomoses and avoidance of manipulation of the biliary tree are postulated as advantages over standard pancreaticoduodenectomy.5 Unfortunately published studies comparing this procedure to the Whipple operation in duodenal pathology have shown no benefit in reduction of morbidity and mortality.32,33 Despite relative simplicity compared to standard pancreaticoduodenectomy, pancreas preserving duodenectomy is a complicated procedure which requires extensive knowledge of the anatomy and familiarity with operations in this region.34 The Whipple procedure is a complex operation requiring significant experience and is prone to complications even in elective surgery. Case series published on the applicability of the Whipple procedure to duodenal trauma have shown mortality rates ranging from 31 to 54%.21,35 Both pancreas preserving duodenectomy and the Whipple procedure are not feasible options in the case of the hemodymically unstable patient. Roux en Y duodeneojejunostomy, initially defined in 1975,7 has been regarded as a safe alternative to the above techniques.2 Although this technique is well established in case of penetrating duodenal injuries where time to diagnosis is short, we failed to find any data regarding its use in unfavorable conditions such as delayed diagnosis, giant ulcers and especially re-leak where significant inflammation is present36 and disseminated tumor cases where the tissue healing is grossly impaired.37 This technique also adds one more anastomosis with a risk of leak in the patient already suffering a hostile abdomen. Where the size of the duodenal wall defect is so large as to prevent the application of tube duodenostomy, the successful use of duodenojejunostomy has been reported for the management of such defects in both trauma and tumor invasion with success.28,29 Therefore the surgeon should be prepared to perform this procedure in cases where there is a potential for very large defects not amenable to tube duodenostomy.
Tube duodenostomy on the other hand is a simple technique, does not involve an anastomosis and is easy to learn, teach, and perform. In the early literature several papers were published which showed no change in outcomes and high leak rates, which likely contributed to the lack of popularity for this method.38,39 Despite the data presented in these early papers, more recent literature indicates excellent outcomes with no leaks, decreased morbidity and shorter hospital stays.40,41 In a recent study of 40 patients with giant duodenal ulcer perforations, the group who underwent tube duodenostomy had one post-operative leak compared to 14 in the conventional repair group (Cellan Jones or Graham patch) and only one mortality.13 Similar results with very favorable outcomes have been reported around the world for patients suffering trauma or a “difficult to manage duodenal stump” following surgery.12,14,42
The common denominator of the patient presenting with “difficult to manage duodenum”, either from trauma or giant ulcers or delayed diagnosis of perforations is hemodynamic instability with hostile abdomen. Complex procedures under these circumstances as previously described are associated with adverse outcomes. In patients with significant comorbidities and/or hemodynamic instability, the damage control principle of trauma surgery is gaining popularity9,43–45 and the tube duodenostomy technique described in this paper fits in well with that principle.
Given the complexity of duodenal injuries and the rarity with which most general surgeons will have to face this problem, the authors feel that the definitive management of complex duodenal injuries injury is best managed at a specialized hepatopancreatobiliary center where possible. Tube duodeneostomy provides an opportunity to stabilize the patient, converting an impending catastrophe to a future scheduled surgery where the possibility for transfer exists, and provides a safe alternative to complex surgery in cases where sub-specialty expertise may not be available.
Conflict of interest statement
None.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author's contributions
Onur Kutlu helped in writing, analysis, and design. Steven Garcia helped in data collection. Sharmila Dissanaike helped in writing, editing, and design.
References
- 1.Jansen M., Du Toit D.F., Warren B.L. Duodenal injuries: surgical management adapted to circumstances. Injury. 2002;33(7):611–615. doi: 10.1016/s0020-1383(02)00108-0. [DOI] [PubMed] [Google Scholar]
- 2.Weigelt J.A. Duodenal injuries. Surgical Clinics of North America. 1990;70(3):529–539. doi: 10.1016/s0039-6109(16)45128-5. [DOI] [PubMed] [Google Scholar]
- 3.Bozkurt B., Ozdemir B.A., Kocer B., Unal B., Dolapci M., Cengiz O. Operative approach in traumatic injuries of the duodenum. Acta Chirurgica Belgica. 2006;106(4):405–408. doi: 10.1080/00015458.2006.11679916. [DOI] [PubMed] [Google Scholar]
- 4.Jani K., Saxena A.K., Vaghasia R. Omental plugging for large-sized duodenal peptic perforations: a prospective randomized study of 100 patients. Southern Medical Journal. 2006;99(5):467–471. doi: 10.1097/01.smj.0000203814.87306.cd. [DOI] [PubMed] [Google Scholar]
- 5.Wig J.D., Kudari A., Yadav T.D., Doley R.P., Bharathy K.G., Kalra N. Pancreas preserving total duodenectomy for complex duodenal injury. Journal of the Pancreas. 2009;10(4):425–428. [PubMed] [Google Scholar]
- 6.McInnis W.D., Aust J.B., Cruz A.B., Root H.D. Traumatic injuries of the duodenum: a comparison of 1 degrees closure and the jejunal patch. Journal of Trauma. 1975;15(10):847–853. [PubMed] [Google Scholar]
- 7.Cukingnan R.A., Jr., Culliford A.T., Worth M.H., Jr. Surgical correction of a lateral duodenal fistula with the Roux-Y technique: report of a case. Journal of Trauma. 1975;15(6):519–523. doi: 10.1097/00005373-197506000-00012. [DOI] [PubMed] [Google Scholar]
- 8.Vaughan G.D., 3rd, Frazier O.H., Graham D.Y., Mattox K.L., Petmecky F.F., Jordan G.L., Jr. The use of pyloric exclusion in the management of severe duodenal injuries. American Journal of Surgery. 1977;134(6):785–790. doi: 10.1016/0002-9610(77)90325-7. [DOI] [PubMed] [Google Scholar]
- 9.Rickard M.J., Brohi K., Bautz P.C. Pancreatic and duodenal injuries: keep it simple. ANZ Journal of Surgery. 2005;75(7):581–586. doi: 10.1111/j.1445-2197.2005.03351.x. [DOI] [PubMed] [Google Scholar]
- 10.Ivatury R.R., Nassoura Z.E., Simon R.J., Rodriguez A. Complex duodenal injuries. Surgical Clinics of North America. 1996;76(4):797–812. doi: 10.1016/s0039-6109(05)70481-3. [DOI] [PubMed] [Google Scholar]
- 11.Lippert K.M., Coleman H.V. Duodenostomy in gastric resection for duodenal ulcer. American Journal of Surgery. 1958;95(5):781–786. doi: 10.1016/0002-9610(58)90627-5. [DOI] [PubMed] [Google Scholar]
- 12.Isik B., Yilmaz S., Kirimlioglu V., Sogutlu G., Yilmaz M., Katz D. A life-saving but inadequately discussed procedure: tube duodenostomy. Known and unknown aspects. World Journal of Surgery. 2007;31(8):1616–1624. doi: 10.1007/s00268-007-9114-3. discussion 1625-1626. [DOI] [PubMed] [Google Scholar]
- 13.Lal P., Vindal A., Hadke N.S. Controlled tube duodenostomy in the management of giant duodenal ulcer perforation: a new technique for a surgically challenging condition. American Journal of Surgery. 2009;198(3):319–323. doi: 10.1016/j.amjsurg.2008.09.028. [DOI] [PubMed] [Google Scholar]
- 14.Bhattacharjee H.K., Misra M.C., Kumar S., Bansal V.K. Duodenal perforation following blunt abdominal trauma. Journal of Emergencies, Trauma and Shock. 2011;4(4):514–517. doi: 10.4103/0974-2700.86650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Girgin S., Gedik E., Yagmur Y., Uysal E., Bac B. Management of duodenal injury: our experience and the value of tube duodenostomy. Ulusal Travma ve Acil Cerrahi Dergisi. 2009;15(5):467–472. [PubMed] [Google Scholar]
- 16.Welch C.E., Rodkey G.V. The surgeon at work. Methods of management of the duodenal stump after gastrectomy. Surgery, Gynecology and Obstetrics. 1954;98:3. [PubMed] [Google Scholar]
- 17.Larsen B.B., Foreman R.C. Syndrome of the leaking duodenal stump. AMA Archives of Surgery. 1951;63(4):480–485. doi: 10.1001/archsurg.1951.01250040490008. [DOI] [PubMed] [Google Scholar]
- 18.Merhav H., Rothstein H., Simon D., Pfeffermann R. Duodenostomy revisited. International Surgery. 1988;73(4):254–256. [PubMed] [Google Scholar]
- 19.Timaran C.H., Martinez O., Ospina J.A. Prognostic factors and management of civilian penetrating duodenal trauma. Journal of Trauma. 1999;47(2):330–335. doi: 10.1097/00005373-199908000-00019. [DOI] [PubMed] [Google Scholar]
- 20.Gupta S., Kaushik R., Sharma R., Attri A. The management of large perforations of duodenal ulcers. BMC Surgery. 2005;5:15. doi: 10.1186/1471-2482-5-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Asensio J.A., Feliciano D.V., Britt L.D., Kerstein M.D. Management of duodenal injuries. Current Problems in Surgery. 1993;30(11):1023–1093. doi: 10.1016/0011-3840(93)90063-m. [DOI] [PubMed] [Google Scholar]
- 22.Martin T.D., Feliciano D.V., Mattox K.L., Jordan G.L., Jr. Severe duodenal injuries. Treatment with pyloric exclusion and gastrojejunostomy. Archives of Surgery. 1983;118(5):631–635. doi: 10.1001/archsurg.1983.01390050097019. [DOI] [PubMed] [Google Scholar]
- 23.Fraga G.P., Biazotto G., Bortoto J.B., Andreollo N.A., Mantovani M. The use of pyloric exclusion for treating duodenal trauma: case series. Sao Paulo Medical Journal. 2008;126(6):337–341. doi: 10.1590/S1516-31802008000600009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sharma D., Saxena A., Rahman H., Raina V.K., Kapoor J.P. ’Free omental plug’: a nostalgic look at an old and dependable technique for giant peptic perforations. Digestive Surgery. 2000;17(3):216–218. doi: 10.1159/000018837. [DOI] [PubMed] [Google Scholar]
- 25.Nussbaum M.S., Schusterman M.A. Management of giant duodenal ulcer. American Journal of Surgery. 1985;149(3):357–361. doi: 10.1016/s0002-9610(85)80107-0. [DOI] [PubMed] [Google Scholar]
- 26.Wynn M., Hill D.M., Miller D.R., Waxman K., Eisner M.E., Gazzaniga A.B. Management of pancreatic and duodenal trauma. American Journal of Surgery. 1985;150(3):327–332. doi: 10.1016/0002-9610(85)90072-8. [DOI] [PubMed] [Google Scholar]
- 27.Ivatury R.R., Gaudino J., Ascer E., Nallathambi M., Ramirez-Schon G., Stahl W.M. Treatment of penetrating duodenal injuries: primary repair vs. repair with decompressive enterostomy/serosal patch. Journal of Trauma. 1985;25(4):337–341. [PubMed] [Google Scholar]
- 28.Liyanage C.A., Abeygunawardhana S., Kumarage S., Deen K.I. Duodenum-preserving local excision of a gastrointestinal stromal tumor. Hepatobiliary & Pancreatic Diseases International. 2008;7(2):214–216. [PubMed] [Google Scholar]
- 29.Kilgus M., Platz A., Trentz O. Duodenal injuries in abdominal trauma. Swiss Surgery. 1999;5(6):251–255. doi: 10.1024/1023-9332.5.6.251. [DOI] [PubMed] [Google Scholar]
- 30.Velmahos G.C., Constantinou C., Kasotakis G. Safety of repair for severe duodenal injuries. World Journal of Surgery. 2008;32(1):7–12. doi: 10.1007/s00268-007-9255-4. [DOI] [PubMed] [Google Scholar]
- 31.DuBose J.J., Inaba K., Teixeira P.G. Pyloric exclusion in the treatment of severe duodenal injuries: results from the National Trauma Data Bank. American Surgeon. 2008;74(10):925–929. doi: 10.1177/000313480807401009. [DOI] [PubMed] [Google Scholar]
- 32.Al-Sarireh B., Ghaneh P., Gardner-Thorpe J. Complications and follow-up after pancreas-preserving total duodenectomy for duodenal polyps. British Journal of Surgery. 2008;95(12):1506–1511. doi: 10.1002/bjs.6412. [DOI] [PubMed] [Google Scholar]
- 33.de Castro S.M., van Eijck C.H., Rutten J.P. Pancreas-preserving total duodenectomy versus standard pancreatoduodenectomy for patients with familial adenomatous polyposis and polyps in the duodenum. British Journal of Surgery. 2008;95(11):1380–1386. doi: 10.1002/bjs.6308. [DOI] [PubMed] [Google Scholar]
- 34.Eisenberger C.F., Knoefel W.T., Peiper M. Pancreas-sparing duodenectomy in duodenal pathology: indications and results. Hepato-Gastroenterology. 2004;51(57):727–731. [PubMed] [Google Scholar]
- 35.Asensio J.A., Petrone P., Roldan G., Kuncir E., Demetriades D. Pancreaticoduodenectomy: a rare procedure for the management of complex pancreaticoduodenal injuries. Journal of the American College of Surgeons. 2003;197(6):937–942. doi: 10.1016/j.jamcollsurg.2003.07.019. [DOI] [PubMed] [Google Scholar]
- 36.Malangoni M.A. Commentary: perforated giant duodenal ulcers: what is the best treatment? American Journal of Surgery. 2009;198(3):324. doi: 10.1016/j.amjsurg.2008.12.039. [DOI] [PubMed] [Google Scholar]
- 37.Noble F., Curtis N., Harris S. Risk assessment using a novel score to predict anastomotic leak and major complications after oesophageal resection. Journal of Gastrointestinal Surgery. 2012;16(6):1083–1095. doi: 10.1007/s11605-012-1867-9. [DOI] [PubMed] [Google Scholar]
- 38.Ivatury R.R., Nallathambi M., Gaudino J., Rohman M., Stahl W.M. Penetrating duodenal injuries. Analysis of 100 consecutive cases. Annals of Surgery. 1985;202(2):153–158. doi: 10.1097/00000658-198508000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Burch J.M., Cox C.L., Feliciano D.V., Richardson R.J., Martin R.R. Management of the difficult duodenal stump. American Journal of Surgery. 1991;162(6):522–526. doi: 10.1016/0002-9610(91)90102-j. [DOI] [PubMed] [Google Scholar]
- 40.Wu X., Zen D., Xu S., Zhang L., Wang P. A modified surgical technique for the emergent treatment of giant ulcers concomitant with hemorrhage in the posterior wall of the duodenal bulb. American Journal of Surgery. 2002;184(1):41–44. doi: 10.1016/s0002-9610(02)00889-9. [DOI] [PubMed] [Google Scholar]
- 41.So J.B., Yam A., Cheah W.K., Kum C.K., Goh P.M. Risk factors related to operative mortality and morbidity in patients undergoing emergency gastrectomy. British Journal of Surgery. 2000;87(12):1702–1707. doi: 10.1046/j.1365-2168.2000.01572.x. [DOI] [PubMed] [Google Scholar]
- 42.Shilyansky J., Pearl R.H., Kreller M., Sena L.M., Babyn P.S. Diagnosis and management of duodenal injuries in children. Journal of Pediatric Surgery. 1997;32(6):880–886. doi: 10.1016/s0022-3468(97)90642-4. [DOI] [PubMed] [Google Scholar]
- 43.McEachern C.G., Sullivan R.E., Arata J.E. Duodenostomy; a method of management of the difficult duodenal stump in certain cases of partial gastrectomy for duodenal ulcer. AMA Archives of Surgery. 1956;72(6):942–947. [PubMed] [Google Scholar]
- 44.Pearson S.C., Mackenzie R.J., Ross T. The use of catheter duodenostomy in gastric resection for duodenal ulcer. American Journal of Surgery. 1963;106:194–205. doi: 10.1016/0002-9610(63)90009-6. [DOI] [PubMed] [Google Scholar]
- 45.Herrod P.J., Kamali D., Pillai S.C. Triple-ostomy: management of perforations to the second part of the duodenum in patients unfit for definitive surgery. Annals of the Royal College of Surgeons of England. 2011;93(7):e122–e124. doi: 10.1308/147870811X602320. [DOI] [PMC free article] [PubMed] [Google Scholar]


