Abstract
INTRODUCTION
We report a case of reconstruction of the right atrial wall using a novel bioresorbable patch derived from porcine small intestinal submucosa.
PRESENTATION OF CASE
Our patient presented with mediastinal aspergillosis as a result of chronic steroid therapy for an oligodendroglioma. Hemodynamic compromise and syncopal episodes secondary to the mass effect of the aspergilloma prolapsing through tricuspid valve necessitated palliative surgical excision.
DISCUSSION
Intraoperatively, it was confirmed that the lesion had eroded into the right atrium and partially occluded right ventricular inflow. In order to achieve appropriate palliation a wide resection of the atrial wall was necessary. The atrial reconstruction was then performed using an extracellular matrix-derived biopatch. This case was further complicated by postoperative bleeding requiring re-operation.
CONCLUSION
We describe the methods used for repair using a novel patch in this rare case of invasive aspergillosis extending into the right atrium and resulting in compromise of diastolic right ventricular filling.
Keywords: Aspergilloma, Mediastinal abscess, Atrial reconstruction, Biomaterial, Xenograft
1. Introduction
Invasive pulmonary aspergillosis remains a problem in immunocompromised patients and surgical excision is often the only definitive treatment. Involvement of the heart or great vessels in case of invasive aspergillosis is rare; incidence estimates or treatment guidelines are not available in the current literature. We report a case of mediastinal aspergillosis with invasion of the right atrium resulting in hemodynamic relevant obstruction of the right ventricular inflow tract.
2. Case report
A 49-year-old female presented to us with new onset syncopal episodes. Prior, this patient had undergone treatment for an oligodendroglioma and incomplete resection of the tumor necessitated long-term treatment with steroids. Secondary to this she developed invasive aspergillosis, initially limited to the mediastinum, and was treated conservatively with antifungal therapy. Upon presentation in our clinic a computed tomography of the chest revealed a mediastinal mass eroding through the right atrium (Fig. 1). Further imaging by echocardiography and cardiac magnetic resonance imaging demonstrated a pedunculated mass crossing the right atrial wall, telescoping into the atrium and ventricle during diastole (Video 1). Palliative surgical resection was recommended given failed conservative management, blood cultures positive for aspergillus and intra-cardiac location of a fungus ball resulting in hemodynamic compromise and syncope.
Fig. 1.

Computed tomography of the chest with intravenous contrast (coronal, transverse and sagittal reconstructions). Images demonstrate the aspergilloma mass occupying the anterior mediastinum and penetrating into the right atrium (red arrows).
Femoral venous and aortic cannulation through a median sternotomy were performed for cardiopulmonary bypass and surgical exploration. Inspection of the heart demonstrated a 5 cm × 4 cm pedicled mass extending into the right atrium and across the tricuspid valve into the right ventricle (Fig. 2). This was excised leaving a 5 mm margin of atrial wall adjacent to the tricuspid annulus. The tricuspid valve and right ventricle were inspected and showed no obvious valvular or endocardial lesions.
Fig. 2.
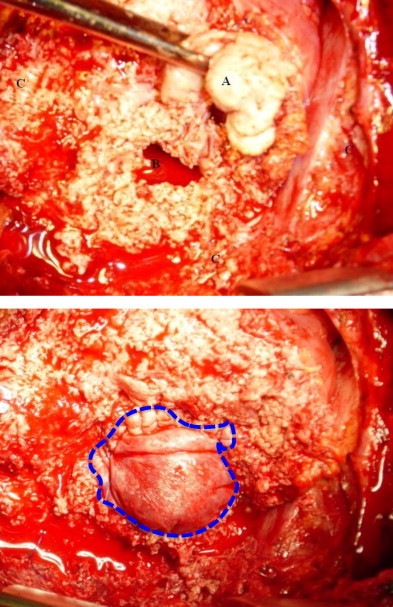
The aspergillus mass (A) is being removed and the defect in right atrium (B) is exposed. Infectious white material surrounds the atrial wall defect obscuring anatomical details (C). Complete repair of right atrial defect with the ECM implant (dashed line) sewn into place with a continuous suture line (lower panel).
To repair the atrial wall defect, an extracellular matrix (ECM) implant (CorMatrix ECM, CorMatrix Cardiovascular, Alpharetta, GA) was used (Fig. 2). This patch is fabricated from porcine small intestinal submucosa using a de-cellularization method that preserves the native structure of the extracellular matrix and provides a resorbable bioscaffold, allowing autologous repopulation and in-growth of the patch into native tissue. The patch was tailored and sewn into place with a running 4-0 polypropylene suture (Prolene, Ethicon Inc., Somerville, NJ). Intra-operative transesophageal echocardiogram (TEE) confirmed minimal tricuspid regurgitation and normal dimensions of the right atrium while the patient was re-warmed and weaned off bypass to a normal sinus rhythm.
The patient's postoperative course was complicated by a sentinel bleed without hemodynamic instability on the 10th postoperative day. Chest tubes were left in place given the continued high volume output from the infected mediastinum. Again 3 days later, she had a second episode of bleeding and was therefore taken back to the operating room for emergent exploration. Upon evaluation of the heart and great vessels no active bleeding was found. However, the running suture line holding the biopatch in place had loosened around the entire circumference. Multiple interrupted, pledgeted 4-0 polypropylene sutures were then placed to reinforce the suture line. The patient recovered from her second surgery without any further complications. The patient was discharged from the hospital on the 25th postoperative day with long-term antifungal therapy and remained free from further cardiac disease involvement at 2 months after the surgery when the patient ultimately succumbed to her recurrent pulmonary aspergillosis resulting in respiratory failure.
3. Discussion
Invasive aspergillosis is a relatively common complication of long-term immunosuppression. Surgical source control is often key for eradication of the infection, but may be challenging if the heart or large vessels are involved. Aspergillus endocarditis or partial myocardial infiltration from pulmonary disease has been described in literature.1 A systematic review of the literature using PubMed and EMBASE suggests that cardiac penetration by mediastinal aspergillosis is quite rare and has not previously been reported.
In the presented case, the surgery was undertaken as a palliative procedure in the setting of failed conservative management and new presentation with recurrent syncopes. Despite aggressive debridement, it was clear that infected tissue was left behind making recurrence of the abscess a likely outcome. The extensive resection of disease left a large defect in the right atrial wall and several reconstructive materials have been proposed including glutaraldehyde fixed pericardium, polyethylene terephthalate (PETE) and polytetrafluoroethylene (PTFE).2,3 Considering the active mediastinal infection we decided against synthetic materials and chose a biomaterial derived from the de-cellularized ECM of porcine small-intestinal submucosa. In animal studies, this patch material has proven superior to synthetic material with myocardial tissue in-growth and remodeling when used for cardiac patching.4,5 Delayed postoperative bleeding was caused by give of the running suture between the atrial wall and ECM patch. This likely resulted from resolution of infection and tissue edema in the postoperative course with insufficient tension at the suture line. An interrupted suturing technique might have prevented such a complication and may be preferable in grossly infected tissues.
Conflict of interest
No conflict of interest to declare for any of the authors.
Funding
No funding was obtained for this study.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Authors’ contributions
MWvB and GM contributed toward the collection of the data; GM made the initial draft of the manuscript; and MWvB, MG, and SM were all involved in the revision of the manuscript.
Appendix A. Supplementary data
References
- 1.Cishek M., Yost B., Schaefer S. Cardiac aspergillosis presenting as myocardial infarction. Clinical Cardiology. 1996;19:824–827. doi: 10.1002/clc.4960191012. [DOI] [PubMed] [Google Scholar]
- 2.Kolettis T., Tsourelis L., Stavridis G., Alivizatos P. Right atrial and septal reconstruction after tumor excision: the single-patch technique. Interactive CardioVascular and Thoracic Surgery. 2009;8:561–562. doi: 10.1510/icvts.2008.201624. [DOI] [PubMed] [Google Scholar]
- 3.Magnan P., Thomas P., Giudicelli R., Fuentes P., Branchereau A. Surgical reconstruction of the superior vena cava. Cardiovascular Surgery. 1994;2:598–604. [PubMed] [Google Scholar]
- 4.Badylak S., Kochupura P., Cohen I., Doronin S., Saltman A., Gilbert T. The use of extracellular matrix as an inductive scaffold for the partial replacement of functional myocardium. Cell Transplantation. 2006;15(Suppl. 1):S29–S40. doi: 10.3727/000000006783982368. [DOI] [PubMed] [Google Scholar]
- 5.Robinson K., Li J., Mathison M., Redkar A., Cui J., Chronos N. Extracellular matrix scaffold for cardiac repair. Circulation. 2005;112:I135–I143. doi: 10.1161/CIRCULATIONAHA.104.525436. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


